Hemiarch versus total aortic arch replacement in acute type A dissection: a systematic review and meta-analysis
Abstract
Background: Despite recent advances in aortic surgery, acute type A aortic dissection remains a surgical emergency associated with high mortality and morbidity. Appropriate management is crucial to achieve satisfactory outcomes but the optimal surgical approach is controversial. The present systematic review and meta-analysis sought to access cumulative data from comparative studies between hemiarch and total aortic arch replacement in patients with acute type A aortic dissection.
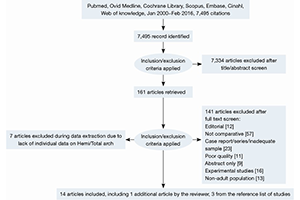
Methods: A systematic review of the literature using six databases. Eligible studies include comparative studies on hemiarch versus total arch replacement reporting short, medium and long term outcomes. A meta-analysis was performed on eligible studies reporting outcome of interest to quantify the effects of hemiarch replacement on mortality and morbidity risk compared to total arch replacement.
Result: Fourteen retrospective studies met the inclusion criteria and 2,221 patients were included in the final analysis. Pooled analysis showed that hemiarch replacement was associated with a lower risk of post-operative renal dialysis [risk ratio (RR) =0.72; 95% confidence interval (CI): 0.56–0.94; P=0.02; I2=0%]. There was no significant difference in terms of in-hospital mortality between the two groups (RR =0.84; 95% CI: 0.65–1.09; P=0.20; I2=0%). Cardiopulmonary bypass, aortic cross clamp and circulatory arrest times were significantly longer in total arch replacement. During follow up, no significant difference was reported from current studies between the two operative approaches in terms of aortic re-intervention and freedom from aortic reoperation.
Conclusions: Within the context of publication bias by high volume aortic centres and non-randomized data sets, there was no difference in mortality outcomes between the two groups. This analysis serves to demonstrate that for those centers doing sufficient total aortic arch activity to allow for publication, excellent and equivalent outcomes are achievable. Conclusions on differences in longer term outcome data are required. We do not, however, advocate total arch as a primary approach by all centers and surgeons irrespective of patient characteristics, but rather, a tailored approach based on surgeon and center experience and patient presentation.
Cover