Salvage esophagectomy for persistent or recurrent disease after definitive chemoradiation
Introduction
The role of surgery in the treatment of locoregionally advanced, non-metastatic (> T1N0M0) esophageal cancer has been debated by oncologists. Because of the potential morbidity of surgical resection, some groups advocate a predominantly non-surgical approach with definitive chemoradiation (cisplatin and 5-FU and 50.4 Gy of radiation therapy, RTOG 85-01, 5 yr 18%) (1). This strategy can achieve long-term survival in predominantly squamous cell carcinoma patients but is associated with a high rate of locoregional relapse (40–60%). Subsequent attempts by cooperative groups to decrease the high locoregional relapse rate with the incorporation of induction chemotherapy and higher doses of radiation therapy (INT 122, 123) failed resulting only in increased toxicity without any improvement in survival or locoregional relapse (60%) (2,3). Two randomized European studies in predominantly squamous cell cancer patients, however, failed to demonstrate a clear survival benefit to the addition of surgery in locoregionally advanced esophageal cancer (4,5). Despite flaws in the study design of these trials, there arose a controversy about the optimal approach and some oncologists began using a predominantly non-operative strategy of definitive chemoradiation. Because of the high locoregional relapse rates of non-operative strategies, a challenging group of esophageal cancer patients arose in the 1990s with residual or recurrent esophageal cancer after definitive chemoradiation whose only curable treatment option was salvage esophagectomy.
Early salvage esophagectomy experience
Because of the high rate of locoregional relapse after definitive chemoradiation we began to see increasing numbers of predominantly squamous cell cancer patients referred to the University of Texas MD Anderson Cancer Center from outside institutions who had relapsed locoregionally and had no other curative options. Salvage esophagectomy is often a more complex and risky operation compared to planned esophagectomy which usually proceeds within a few months of the completion of neoadjuvant chemoradiation. Salvage esophagectomy for recurrent esophageal cancer after definitive chemoradiation can occur many months or years after treatment when tissue planes are often obscured by post-radiation fibrosis. The deleterious effect of radiation on the microvasculature and tissues can lead to complications in healing and increased esophageal leaks. Because of the potentially increased risks associated with the higher doses of radiation received (>60 Gy) and the prolonged time from the completion of radiation therapy, many surgeons have been reluctant to operate on this group. Additionally, many of these patients at evaluation are not eligible for salvage esophagectomy because of physiologic deterioration after definitive chemoradiation or metastases identified during restaging. Despite these potential increased risks, our group undertook salvage esophagectomies in a subset of these patients because of the lack of an alternative curative option. We reported our initial experience with salvage esophagectomy (n=13) in 2002 and compared the outcome to a control group of patients (n=99) who during the same time period underwent planned esophagectomy 4 to 6 weeks following preoperative chemoradiation. Our initial report noted an increase in perioperative morbidity and mortality compared to planned esophagectomy (anastomotic leak: 38% vs. 7%; mortality: 15% vs. 6%) (6). This increased morbidity may have been due in part to the higher doses of radiation therapy and the location of the tumors which sometimes required more extensive concomitant procedures such as laryngectomies. Importantly though, long-term survival was able to be achieved in a subset of patients (5 yr 25%) which was not significantly different from the long-term outcome of planned esophagectomy (5 yr 30%) at that time. Because of the lack of alternative curative treatments we felt these results warranted evaluation of all physiologically fit patients with esophageal cancer in an experienced high volume esophageal center who relapsed locoregionally after definitive chemoradiation.
Subsequent to our report other groups reported their initial results with salvage esophagectomy and confirmed the finding of increased morbidity and hospital use (Table 1) (11). Leak rates varied from 21 to 38% and conduit necrosis was also noted at rates up to 16%. The operative mortality, however, was acceptable and there was an ability to achieve long-term survival in a subset of patients (5 yr: 25–32%). Despite the increased short-term morbidity of salvage esophagectomy, these data suggested that salvage esophagectomy was a viable therapeutic option for physiologically fit patients whose cancer recurred locoregionally after definitive chemoradiation and who did not demonstrate systemic disease.
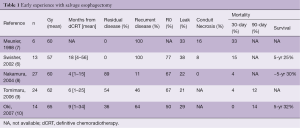
Full table
Modern era experience with salvage esophagectomy
The initial experience with salvage esophagectomies demonstrated higher than expected esophageal leak rates and even some incidents of conduit necrosis (Table 1). This increased morbidity may have been due to the high doses of radiation (>60 Gy) given in some instances to patients being treated non-operatively with definitive chemoradiation. The use of higher doses of radiation therapy occurred because of the unfounded belief by some oncologists that higher doses of radiation led to enhanced locoregional control. As INT 122 and 123 demonstrated, increased doses of radiation led only to increased toxicity with resulting decreased overall survival and no improvement in locoregional control (60% relapse) (2,3). In an effort to understand the reasons for the increased rate of esophageal anastomotic leaks, our group evaluated the risk of esophageal leak according to the location of the anastomosis within the radiated field (12). We found that the risk of “in-field” anastomotic leak was 39% vs. 2.6% for “out-of-field” anastomoses with a hazard ratio of 5.37 (95% CI, 2.21–13.04) for “in-field” anastomoses. The desire to place the anastomosis “out-of-field”, however, must be tempered by the knowledge that three field surgery has a hazard ratio of 10.01 (95% CI, 3.83–26.21) for anastomotic leaks compared to two field intrathoracic anastomoses (12). Our group began evaluating different strategies to reduce esophageal leaks. These strategies included utilizing alternative vascularized conduits, two-stage procedures when necessary and omental tissue transposition. We also worked hard to obtain radiation records to determine if the conduit or the esophageal anastomosis location was planned within the radiation field. The radiation records often allowed us to consider locations for the anastomosis outside of the radiation field or led us to consider alternative vascularized conduits for heavily irradiated stomachs.
Alternative vascularized conduits
Many salvage esophagectomies are performed using the stomach as the conduit; in some instances this is a reasonable strategy but in some cases in which the patient has had previous mediastinal or neck radiation, previous thoracic or abdominal operations or has major comorbidities that may affect the stomach (gastroparesis, gastric outlet obstruction or peptic ulcer disease) consideration for an alternative vascularized conduit may need to be considered. Other patients who have had high doses of radiation to the greater curvature or celiac access are also at increased and should be considered for an alternative conduit. Alternative vascularized conduits to the stomach include the colon, super-charged colon or a long-segment supercharged jejunal graft. A long-segment jejunal pedicle with microvascular augmentation is the procedure of choice at our institution. We perform this procedure in collaboration with an experienced plastic surgery team skilled with microvascular procedures. This technique also allows additional graft length which can be helpful in high cervical-enteric anastomoses. The long-segment supercharged jejunal graft has allowed our group to achieve reduced morbidity in patients who would be at high risk with traditional techniques (13,14).
Two-stage procedures
Salvage esophagectomies can often be technically demanding resections because of the fibrosis that has developed from the high doses of radiation or the prolonged period since the completion of chemoradiotherapy. In many instances the tissues cannot be separated easily, are indurated and bleed easily. Additionally, some salvage esophagectomies occur in previously resected patients where adhesions further obliterate tissue planes. The process of removing the tumor and esophagus in these instances can be quite challenging and time consuming. In such cases immediate re-construction may not be optimal because of the fatigue of the operating teams and the need for a difficult reconstruction sometimes involving jejunal interposition and microvascular anastomoses. In such instances, staging the resection and reconstruction may be the best option to decrease potential morbidity. The resection of the esophagus can be accompanied by placement of a proximal esophageal diversion and enteral alimentation via a gastric tube. The time to reconstruction with a jejunal interposition can be as short as 24 hours to as long as six weeks after the initial operation. With proper planning these two stage strategies can lead to low morbidity in high risk patients that is comparable to the morbidity achieved with low risk patients undergoing standard esophagectomy (15).
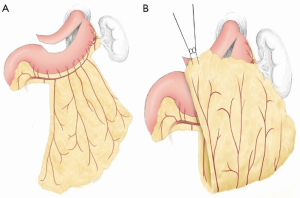
Omental transposition
Use of an omental graft to reduce anastomotic leak is another strategy that our group has evaluated. The omental graft can be based on two or three feeding vessels off the right gastroepiploic artery usually just proximal to the short gastric arteries (Figure 1). The omentum is mobilized off the transverse colon in the avascular plane. In many instances the flap can be tailored to reduce the bulk. Only the “filet” of the omentum needs to be utilized to cover the anastomosis and gastric staple line. The omental graft is fixed to the stomach prior to transposition to the chest to facilitate passage through the hiatus (Figure 1). Transposing too large of an omental graft is difficult to mobilize through the hiatus and can lead to atelectasis and unneeded bulk in the right hemi-thorax.
Several randomized studies have demonstrated a marked decrease in anastomotic leak rates with omental flap transposition (16,17). Additionally the presence of an omental graft between the anastomosis and the posterior membrane of the trachea allows placement of a stent with less risk of erosion if a leak develops. This reduces the need for re-operation with esophageal leaks. Review of our experience with omental transposition found that the use of an omental graft dramatically decreased leak rates during esophagectomy for both planned and salvage esophagectomies (18). Omental reinforcement was used in 215 of 607 patients over a 10 year period. Patients with omental flap coverage had a significantly lower risk of anastomotic leak (HR: 0.2; 95% CI, 0.12–0.56) by multivariate analysis. Salvage esophagectomy was performed in 69 patients and 23 had omental transposition. The leak rate in salvage esophagectomies with omentum was 4.6% vs. 15% without omental reinforcement. Our data corroborates that of others and suggest that the use of omental flap coverage should be considered in all patients undergoing salvage esophagectomy.
We then reviewed our experience with salvage esophagectomy in the modern era and compared it with a comparable control group during the modern era that had planned esophagectomy (19). Unlike in our initial report, we found no significant increase in esophageal leak rates or operative mortality (Table 2) compared to planned esophagectomy. This may have been due to various factors including lower radiation doses and a larger portion of adenocarcinoma histology and lower esophageal location but it may also have been due to the increased use of omental coverage, alternative vascularized conduits and two stage procedures when necessary. Importantly, the long-term survival was similar to planned esophagectomy after preoperative chemoradiation (Table 2) suggesting again that all physiologically fit patients in the modern era with persistent or recurrent esophageal cancer after definitive chemoradiation should be evaluated at a high volume esophageal center for salvage esophagectomy.
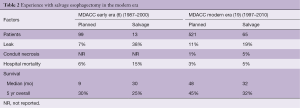
Full table
Role of selective salvage esophageal resection after definitive chemoradiation: RTOG 0246
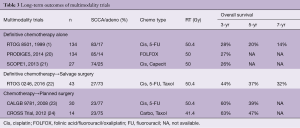
RTOG 85-01 demonstrated that long-term survival (5 yr 18%) could be obtained with definitive chemoradiation in predominantly squamous cell carcinoma esophageal cancer patients with concurrent cisplatinum and 5-FU and 50.4 Gy of radiation therapy (1). Although this allowed an organ preserving strategy without the need for esophagectomy, the locoregional recurrence rate was quite high (40–60%). Subsequent attempts by RTOG to reduce this locoregional failure rate included adding induction chemotherapy and higher doses of radiation therapy (INT 121, 122) but these attempts failed and only resulted in increased toxicity, reduced survival and locoregional relapse rates of 60% (2,3). Recently, definitive chemoradiation strategies in Europe have attempted to add the novel therapeutic agent cetuximab to chemoradiation but as Table 3 demonstrates (SCOPE1), these attempts have not led to improved results with no significant improvements in locoregional control or survival (21).
Full table
Because of these failures to improve survival and reduce locoregional relapse through increasing chemotherapy, radiation therapy or adding novel agents, RTOG 0246 was proposed. The hypothesis was that the selective use of salvage surgery for persistent or recurrent esophageal cancer after definitive chemoradiation could improve the results of definitive chemoradiation alone while still allowing an organ-preserving approach in a subset of patients (21). Patients were therefore treated with an aggressive regimen of chemotherapy followed by concurrent chemoradiation and then evaluated by a multi-disciplinary panel of medical oncology, radiation oncology and surgery for suspicion of persistent disease. If patients were suspected of having persistent disease after definitive chemoradiation (Clin Non-CR) then they were taken immediately to surgery. If they were felt to be free of disease (Clin CR) then they were followed very closely with serial endoscopy, CT scans and CT-PET when available for recurrent disease. If recurrent locoregional disease developed without evidence of systemic disease and the patients were physiologically fit then they were offered salvage esophagectomy. This strategy differed from other definitive chemoradiation strategies because of the multidisciplinary evaluation of patients after chemoradiation and the immediate resection of patients who had suspected persistent disease (Clin Non-CR). Additionally, this trial emphasized a very careful surveillance program (every 3 months ×2, then every 6 months × then yearly) for Clin CR patients so that salvage esophagectomy could be identified at the earliest possible time point of locoregional recurrence. Recently, long-term results of this selective resection strategy (8.1 yrs of median follow-up) have been published (Table 3) (25). Compared to other modern trials with definitive chemoradiation alone (SCOPE1 and PRODIGES1/ACCORD17), RTOG 0246 had improved survival and locoregional control (20,21). The addition of selective salvage surgery with careful surveillance may therefore be an important adjunct to definitive chemoradiation approaches. Whereas higher doses of chemotherapy, radiation therapy and novel agents have failed to improve outcomes of definitive chemoradiation, selective salvage surgery does appear to enhance this outcome.
Forty-one patients were entered in RTOG 0246 and of the 37 patients who completed concurrent chemoradiation 21 were felt to have persistent disease (52%). Seventeen patients (41%) were taken immediately to surgery and were all found to have residual disease. Of the 15 patients who were felt to be Clin CR, 3 patients (20%) developed recurrent locoregional disease without distant metastases on surveillance and underwent salvage resection 3 to 18 months after the completion of definitive chemoradiation. The overall survival of the group at 5 years is 37% which is better than other modern day definitive chemoradiation alone studies (20,21) and is comparable to most trimodality studies except for the CROSS trial (Table 3) (24). Importantly, 20 out of 41 patients (49%) on RTOG 0246 did not require esophagectomy.
Personal view
How are we to interpret these studies? The CROSS study has certainly set a high bar for the trimodality approach with concurrent chemoradiation and planned esophagectomy resulting in 5 year survivals of 47% for adenocarcinoma and squamous cell carcinoma patients. Given these impressive results in the CROSS study with trimodality, our group’s approach is usually to recommend chemoradiation with planned esophagectomy to all physiologically fit patients who are willing to undergo resection and do not have high esophageal tumors that would require concomitant laryngectomy. The observation in the CROSS study that squamous cell carcinoma patients had very high pathologic complete response rates does not in our opinion preclude a trimodality approach for squamous cell cancer since our experience at MDACC with pathologic complete response has not found such a drastic difference between adenocarcinoma and squamous cell carcinoma.
Selective salvage esophagectomy as utilized in RTOG 0246 is a viable approach and is reserved for patients who are at higher risk of esophageal resection or refuse to undergo surgery. In these high risk patients selective salvage resection is done only for those patients who have definitively proven persistent or recurrent esophageal cancer and understand the increased risks of resection. One of the challenges of selective salvage resection strategies is the inability to definitively prove that there is no residual microscopic disease. Endoscopic ultrasound with biopsies, CT-PET and CT scans are not sensitive enough to detect microscopic residual disease (26). Clinical intuition may be the best (esophageal stricture, dysphagia, etc.) but it is not definitive. Perhaps in the future molecular assays or blood biomarkers will allow us to selectively identify those patients with a pathologic complete response who we would feel comfortable observing without surgery. Until then our recommendation for physiologically fit patients with locoregional esophageal cancer continues to be a trimodality approach with induction chemoradiation followed by planned esophagectomy.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Cooper JS, Guo MD, Herskovic A, et al. Chemoradiotherapy of Locally Advanced Esophageal Cancer: Long-term Follow-up of a Prospective Randomized Trial (RTOG 85-01). JAMA 1999;281:1623-7. [Crossref] [PubMed]
- Minsky BD, Neuberg D, Kelsen DP, et al. Neoadjuvant Chemotherapy Plus Concurrent Chemotherapy and High-Dose Radiation for Squamous Cell Carcinoma of the Esophagus: A Preliminary Analysis of the Phase II Intergroup Trial 0122. J Clin Oncol 1996;14:149-55. [Crossref] [PubMed]
- Minsky BD, Pajak TF, Ginsberg RJ, et al. INT 0123 (Radiation Therapy Oncology Group 94-05) Phase III Trial of Combined-Modality Therapy for Esophageal Cancer: High-Dose Versus Standard-Dose Radiation Therapy. J Clin Oncol 2002;20:1167-74. [Crossref] [PubMed]
- Mariette C, Dahan L, Mornex F, et al. Surgery Alone Versus Chemoradiotherpy Followed by Surgery for Stage I and II Esophageal Cancer: Final Analysis of Randomized controlled Phase III Trial FFCD 9901. J Clin Oncol 2014;32:2416-22. [Crossref] [PubMed]
- Stahl M, Stuschke M, Lehmann N, et al. Chemoradiation with and without surgery in patients with locally advanced squamous cell carcinoma of the esophagus. J Clin Oncol 2005;23:2310-7. [Crossref] [PubMed]
- Swisher SG, Wynn P, Putnam JB, et al. Salvage Esophagectomy for Recurrent Tumors after Definitive Chemotherapy and Radiotherapy. J Thorac Cardiovasc Surg 2002;123:175-83. [Crossref] [PubMed]
- Meunier B, Raoul J, Le Prise E, et al. Salvage esophagectomy after unsuccessful curative chemoradiotherapy for squamous cell cancer of the esophagus. Dig Surg 1998;15:224-6. [Crossref] [PubMed]
- Nakamura T, Hayashi K, Ota M, et al. Salvage esophagectomy after definitive chemotherapy and radiotherapy for advanced esophageal cancer. Am J Surg 2004;188:261-6. [Crossref] [PubMed]
- Tomimaru Y, Yano M, Takachi K, et al. Factors affecting the prognosis of patients with esophageal cancer undergoing salvage surgery after definitive chemoradiotherapy. J Surg Oncol 2006;93:422-8. [Crossref] [PubMed]
- Oki E, Morita M, Kakeji Y, et al. Salvage esophagectomy after definitive chemoradiotherapy for esophageal cancer. Dis Esophagus 2007;20:301-4. [Crossref] [PubMed]
- Nishimura M, Daiko H, Yoshida J, et al. Salvage Esophagectomy Following Definitive Chemoradiotherapy. Gen Thorac Cardiovasc Surg 2007;55:461-4. [Crossref] [PubMed]
- Juloori A, Tucker SL, Komaki R, et al. Influence of preoperative radiation field on postoperative leak rates in esophageal cancer patients after trimodality therapy. J Thorac Oncol 2014;9:534-40. [Crossref] [PubMed]
- Ascioti AJ, Hofstetter WL, Miller MJ, et al. Long-segment, supercharged, pedicled jejunal flap for total esophageal reconstruction. J Thorac Cardiovasc Surg 2005;130:1391-8. [Crossref] [PubMed]
- Swisher SG, Hofstetter WL, Miller MJ. The supercharged microvascular jejunal interposition. Semin Thorac Cardiovasc Surg 2007;19:56-65. [Crossref] [PubMed]
- Morita M, Nakanoko T, Kubo N, et al. Two-stage operation for high-risk patients with thoracic esophageal cancer:an old operation revisited. Ann Surg Oncol 2011;18:2613-21. [Crossref] [PubMed]
- Bhat MA, Dar MA, Lone GN, et al. Use of pedicled omentum in the esophagogastric anastomosis for prevention of anastomotic leak. Ann Thorac Surg 2006;82:1857-62. [Crossref] [PubMed]
- Dai JG, Zhang ZY, Min JX, et al. Wrapping of the omental pedicle flap around anastomosis after esophagectomy for esophageal cancer. Surgery 2011;149:404-10. [Crossref] [PubMed]
- Sepesi B, Swisher SG, Walsh GL, et al. Omental reinforcement of the thoracic esophagogastric anastomosis: An analysis of leak and reintervention rates in patients undergoing planned and salvage esophagectomy. J Thorac Cardiovasc Surg 2012;144:1146-50. [Crossref] [PubMed]
- Marks JL, Hofstetter W, Correa AM, et al. Salvage esophagectomy after failed definitive chemoradiation for esophageal adenocarcinoma. Ann Thorac Surg 2012;94:1126-32. [Crossref] [PubMed]
- Conroy T, Galais MP, Raoul JL, et al. Definitive Chemoradiotherapy with FOLFOX versus Fluorouracil and Cisplatin in Patients with Oesophageal Cancer (PRODIGE5/ACCORD17): Final Results of a Randomised Phase 2/3 Trial. Lancet Oncol 2014;15:305-14. [Crossref] [PubMed]
- Crosby T, Hurt CN, Falk S, et al. Chemoradiotherapy with or without Cetuximab in Patietns with Oesophageal Cancer (SCOPE1): A Multicentre, Phase 2/3 Randomised Trial. Lancet Oncol 2013;14:627-37. [Crossref] [PubMed]
- Swisher SG, Moughan J, Komaki RU, et al. Final Results of NRG Oncology RTOG 0246: An Organ-Preserving Selective Resection Strategy in Esophageal Cancer Patients Treated with Definitive Chemoradiation. J Thorac Oncol 2017;12:368-74. [Crossref] [PubMed]
- Tepper J, Krasn MJ, Niedzwiecki D, et al. Phase III Trial of Trimodality Therapy with Cisplatin, Fluorouracil, Radiotherapy, and Surgery Compared With Surgery Alone for Esophageal Cancer: CALGB 9781. J Clin Oncol 2008;26:1086-92. [Crossref] [PubMed]
- van Hagen P, Hulshoff MC, van Lanschot JJ, et al. Preoperative Chemoradiotherapy for Esophageal or Junctional Cancer. N Engl J Med 2012;366:2074-84. [Crossref] [PubMed]
- Swisher SG, Winter KA, Komaki RU, et al. A phase II study of a paclitaxel-based chemoradition regimen with selective surgical salvage for resectable locoregionally advanced esophageal cancer: initial reporting of RTOG 0246. Int J Radiat Oncol Biol Phys 2012;82:1967-72. [Crossref] [PubMed]
- Swisher SG, Maish M, Erasmus JJ, et al. Utility of PET, CT, and EUS to identify pathologic responders in esophageal cancer. Ann Thorac Surg 2004;78:1152-60. [Crossref] [PubMed]