How to perform valve sparing reimplantation in a tricuspid aortic valve
Aortic valve sparing procedures are increasingly being used to treat aortic root pathologies. Reimplantation of the aortic valve, first described by Dr Tirone David, is a technically demanding procedure whose long-term results are critically dependent on perfect intraoperative restoration of valve anatomy and function. There exists significant variation in how this procedure is performed by different surgeons, which is likely contributory to the heterogeneity in reported results. We describe a systematic approach to aortic valve reimplantation procedure focusing on key technical aspects.
Keywords: Aortic root aneurysm; aortic regurgitation; valve sparing surgery; aortic valve reimplantation
Submitted Dec 21, 2012. Accepted for publication Jan 25, 2013.
doi: 10.3978/j.issn.2225-319X.2013.01.16
Introduction
The technique of valve sparing root replacement is a desirable option for the treatment of aortic root pathology in the absence of significant aortic cusp disease. In this article, we describe and illustrate our approach to aortic valve (AV) sparing root replacement using the reimplantation technique, originally described by David and Feindel (1). We focus on technical aspects of the reimplantation technique in the setting of tricuspid aortic valve.
The surgical steps towards the reimplantation technique are described below as the following: (I) Aortic valve exposure and assessment; (II) Root preparation and dissection; (III) Graft sizing; (IV) Proximal suture line; (V) Graft preparation and fixation; (VI) Valve reimplantation; (VII) Valve testing and leaflet management; (VIII) Coronary reimplantation; (VIIII) Distal closure.
Operative techniques - valve sparing reimplantation
Aortic valve exposure and assessment
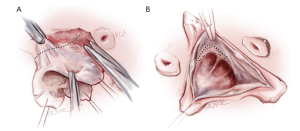
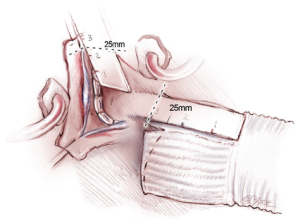
After cardio-pulmonary bypass is initiated, the aorta is cross clamped at the level of the distal ascending aorta and the heart is arrested with warm blood cardioplegia. A horizontal aortotomy is performed 1 cm above the sinotubular junction (STJ) (Figure 1). Care is taken to avoid injuring the right coronary ostium, which can be misplaced cranially in certain cases of severe aortic root aneurysm or in bicuspid aortic valve. At this stage, the aortotomy is not circumferential and posterior wall above the main stem is left intact. This connection to the posterior sinus allows pulling the aortic valve from the depth by cranial traction on the ascending aorta with a traction stitch. Then, traction stitches (4-0 polypropylene) are placed at the tip of each of the three commissures. These stitches are maintained on artery forceps and are used to assess the valve coaptation and to expose the aortic root during external dissection.
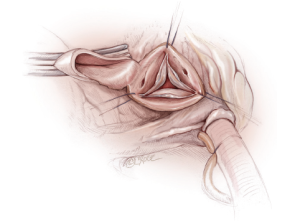
Applying an axial traction on the three commissural stitches, assessment of the valve leaflets, sinuses and annulus is performed. Careful attention is paid to leaflet tissue quality, presence of stress fenestrations or leaflet prolapse. A transverse fibrous band on a leaflet and a lower free margin in comparison to adjacent leaflet are signs of leaflet prolapse. Prolapse identified at this stage is repaired after valve reimplantation.
Root preparation and dissection
The first step of the reimplantation procedure is dissection of the aortic root as low as possible, given the natural anatomic limitations of the heart structures. The root dissection is started along the non-coronary (NC) sinus and continued towards the NC/left coronary (LC) commissure (Figure 2A, B). In this area, the ventriculo-aortic junction (VAJ) of the AV is fibrous and dissection can be carried to the level of insertion of the leaflets. The sinus of Valsalva is then resected leaving approximately 5 to 8 mm of the base of the sinus wall attached.
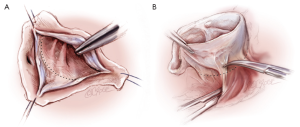
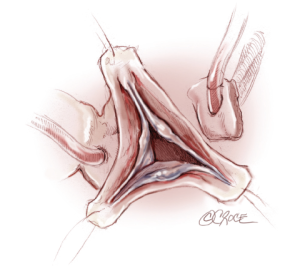
Before any external dissection of the right sinus, the right coronary button is harvested cutting it from the inside of the aortic root with a generous patch of sinus wall (Figure 3). Then, the dissection is continued towards the base of NC/right coronary (RC) commissure (Figure 4A). In this area the anatomical limit of the dissection is composed of membranous septum in relation to the NC/RC commissure and the muscular septum, in regards to the right sinus. The limit of external dissection does not reach the plane passing through the nadir of leaflet insertion (Figure 4B).
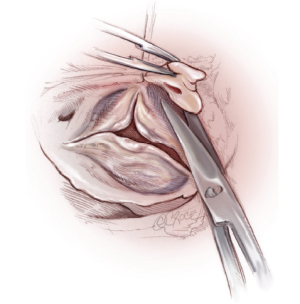
Then surgical dissection is continued towards the RC/LC commissure and around to the left sinus (Figure 5). In this area, the anatomical limit of dissection is composed of the muscular portion (interventricular septum and right ventricular outflow tract muscle) of the VAJ in relation to the RC/LC commissure and the roof of the left atrium in regards to the left sinus (Figure 5A). The limit of external dissection reaches the plane passing through the nadir of leaflet insertion at the level of the left coronary leaflet, but not at the RC/LC commissure (Figure 5B).
The left coronary button is then harvested cutting it like the right coronary button from the inside of the aortic root with a generous patch of sinus wall. Both coronary ostia are cannulated with micro osteal cannulae (DLP®, Medtronic, Inc., Minneapolis, Mn) for intermittent blood cardioplegia. The cannulae are fixed with 4-0 polypropylene suture snugged through a tourniquet (Figure 6). Finally, the external dissection of the root is achieved by dissection of the base of the left sinus.
Graft sizing
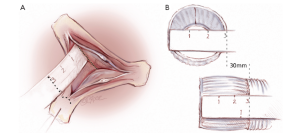
Our current graft-sizing technique is based on the principle that in a normally functioning aortic valve, the height of the commissure (measured from the base of the interleaflet triangle to the top of the commissure) is equal or slightly smaller to the diameter of the STJ. Although various components of the aortic root and the functional aortic annulus may dilate in the setting of root aneurysms, the height of the commissure remains relatively constant. The height of the commissure is most easily measured with a ruler at the NC/LC commissure by first drawing a connecting line between the nadirs of the 2 adjacent cusps (base of interleaflet triangle) and measuring the distance between this line and the top of the commissure (Figure 7A). This measurement corresponds to the size of the graft chosen. When this measurement does not correspond to a labelled graft size, the next larger size graft is chosen. Although this technique can be applied for use with any type of graft, this principle is further reinforced by the idea that in the Valsalva graft (GelweaveValsalva™ graft, Vascutek Ltd, a Terumo company, Renfrewshire, Scotland), the height of the sinus portion of the graft is equal to its diameter (Figure 7B).
Proximal suture line
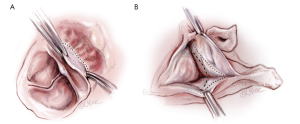
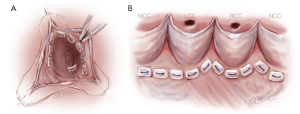
Twelve 2-0 Tycron sutures with pledgets are generally used for proximal suture line. They are distrusted along the circumference of the ventriculo-aortic junction. Sutures are passed from inside to outside the aorta with the pledgets on the inside, starting from the NC/LC commissure and moving clockwise (Figure 8A). Along the fibrous portion of the aortic annulus, these sutures are inserted along the horizontal plane formed by the base of the inter-leaflet triangles. Importantly, however, along the non-fibrous portions of the annulus where the external dissection of the aortic root is limited by muscle, these sutures are inserted along the lowest portion of the freely dissected aortic root making the proximal suture line slightly higher at the NC/RC and RC/LC commissures compared to the NC/LC commissure (Figure 8B). Attention must be paid to avoid contact between the pledgets and the cusp tissues. Thus it is safe to consider 2 mm distance in between them.
Graft preparation and fixation
A Dacron prosthesis with built-in neo-aortic sinuses is generally used. To prevent valve distortion, the three commissures must be attached to the prosthesis along the same plane that corresponds to the sinotubular junction of the graft. Due to the anatomy of the base of the aortic root, the proximal sutures are not in a plane and the proximal end of the graft need to be tailored in consequence. Therefore, the height of the freely dissected portion of the NC/RC and RC/LC commissures are measured. This height is the distance from the proximal suture to the top of the commissure (Figure 9). These measures are used to determine the amount of graft material that needs to be trimmed. Thus, the height of the trimmed portions on the graft is the difference between height of the unrestricted NC/LC commissure and the distance from the proximal suture line to the top of the respective NC/RC and RC/LC commissures. The exact shape of the trimmed portions is less important as the prosthesis will accommodate to the external limitations of the aortic root.
The pledgeted sutures are then passed through the base of the prosthesis, respecting the spaces between sutures and importantly, the curvilinear contour of the proximal suture line (Figure 10). The commissural traction sutures are passed through the graft and pulled up together while tying down the prosthesis to ensure appropriate seating around the aortic annulus.
Valve reimplantation
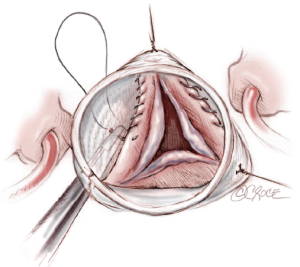
The commissures are reimplanted first using 4-0 polypropylene sutures while pulling up on the prosthesis and the native commissure and then tied into place. With our specific method of graft sizing and trimming, the tips of the three commissures should reach the same level/plane which correspond the neo-STJ in a Valsalva graft. Radial traction is then applied on two adjacent commissural sutures and this help to delineates the ‘line of implantation’. This running suture line is performed in small regular steps passing the suture from outside the prosthesis to inside and through the aortic wall, staying close to the annulus, and then back out of the prosthesis (Figure 11).
Valve testing and leaflet management
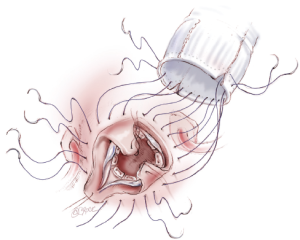
After valve reimplantation, it is critical to re-examine the leaflets for any unmasked prolapse, symmetry, and the height and depth of coaptation. After placing the leaflets into their closure position, using a syringe of water, the valve is flushed with force and observed after suction of the water (Figure 12). Attention is focused on the mid portion of the leaflets free-edges. Prolapse is present when the level of a free-edge is lower than the adjacent one(s). Prolapse can be confirmed by pushing gently the middle of the free-edge towards the ventricle. If one or two leaflet are prolapsing, the normal one(s) is taken as reference for the repair. If all three leaflets show low free-edge level (e.g., annulus level), then all three are repaired taking the mid-height of the sinus of Valsalva as reference. Prolapses are repaired using central free-edge plication technique with a 6-0 polypropylene suture. If an important amount of tissue needs to be excluded, the top of the plication may be resected and a blocked running 6-0 polypropylene suture is used to close the defect from the middle of the leaflet belly towards the free-edge. Free-edge resuspension technique, with running suture of 7-0 Goretex, may be used in presence of stress fenestrations to correct the prolapse, reinforce the free-edge and close the fenestration. The running suture is passed over and over the free-edge and the fenestration from one commissure to the other. The suture is then tied on the external side of the aorta after adjusting the free-edge length by pulling on each side of the suture.
Coronary reimplantation
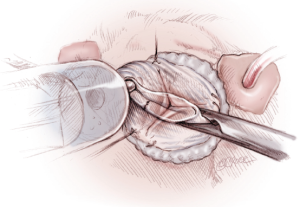
The left coronary button is the first to be reimplanted. A hole of approximately 6 to 8 mm of diameter is made in the graft in regards to the coronary button. Reimplantation is performed with a running suture of 5-0 polypropylene (Figure 13). The suture starts on the inferior portion of the button (Figure 13A). The cannula can remain in the ostia to avoid backflow from the coronary while suturing this portion. At this level, the stitches are passed close to the opening of the ostium (Figure 13B). After several passages, the superior portion of the button is cut from the ascending aorta and trimmed. The cannula is removed from the ostia and the inferior portion of the button is approximated to the graft by tightening the suture (Figure 13C). The suture is continued on both sides and on the superior portion of the button where stitches are passed distant from the opening of the ostia. A free autologous pericardial strip can be used on the button side to improve haemostasis. A similar technique is used for right coronary reimplantation. We believe this technique of suturing coronary buttons allows to minimize kinking or twisting of the proximal portions of the coronaries.

Cardioplegia is then administered through the distal end of the graft with partial clamping in order to distend the new aortic root. This maneuver allows to assess sutures haemostasis and valve competence by indirect sign such as root pressure and left ventricular dilatation. A limited echocardiographic view may also be obtained at this time. The cardioplegia solution is then slowly aspirated out of the prosthesis without distorting the leaflets for a last check of valve configuration.
Distal closure
Finally, the distal anastomosis is performed at the level of normal aorta with 4-0 polypropelene on a small needle. A Teflon felt strip is used as external reinforcement on the native aorta if this one is judged fragile.
Conclusions
The main concept of our valve sparing reimplantation technique is to restore the functional anatomy of the aortic valve and root while respecting heart’s anatomy. Therefore, several key technical aspects are followed including adequate remodeling and support of the ventriculoaortic junction, creation of neo-aortic sinuses, cusp repair and respect of coronary anatomy. This results in a standard operative technique which is reproducible and when applied systematically can result in consistent and excellent long-term outcome (2).
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- David TE, Feindel CM. An aortic valve-sparing operation for patients with aortic incompetence and aneurysm of the ascending aorta. J Thorac Cardiovasc Surg 1992;103:617-21;discussion 622.
- de Kerchove L, Boodhwani M, Glineur D, et al. Effects of preoperative aortic insufficiency on outcome after aortic valve-sparing surgery. Circulation 2009;120:S120-6.





