Graft sizing for aortic valve sparing surgery
Introduction
Valve-sparing aortic root replacement has been demonstrated as an effective technique not only for the treatment of aortic root pathology, but also for facilitating repair of regurgitant aortic valves. Graft sizing is an important step for valve sparing procedures and sizing methods have generated significant controversy among surgeons. The purpose of this manuscript is to review the fundamentals of aortic root anatomy and valve function as they pertain to graft sizing, to explore the existing methods for graft sizing, and to discuss implications of inappropriate sizing on the outcome of the procedure.
Aortic valve and root anatomy and function
The aortic valve and root is a dynamic structure with complex interrelationships between the two components contributing to normal valve function (1,2). There are several important anatomic and physiologic principles that are relevant to graft sizing in valve-sparing aortic root replacement surgery. First is the concept of the functional aortic annulus (FAA), which consists of the sinotubular junction (STJ) and the ventriculo-aortic junction (VAJ). Both of these components play an important role in providing support to the valve cusps and alteration of either component can result in cusp prolapse or restriction causing aortic insufficiency (Figure 1). The second principle is that the VAJ and the STJ are roughly proportional in diameter in a normal aortic valve, with the STJ typically being approximately 10-15% smaller than the VAJ (3). In the context of aortic valve and root pathology, however, either one of these components can be dilated. The third important principle is that when these components of the FAA dilate slowly over time, cusp remodeling can take place, which prevents the occurrence of significant aortic insufficiency. Therefore, patients may occasionally present with significant dilation of the VAJ and STJ with only minimal aortic insufficiency. The cusps in these settings are often thinner and elongated and can have stress fenestrations due to increased leaflet stress. Furthermore, when the VAJ and STJ dimensions are restored to normal, the excess leaflet tissue can cause cusp prolapse, which requires correction. Lastly, it is important to distinguish between the two types of valve-sparing procedures; the reimplantation procedure affects both the VAJ and the STJ, whereas the remodeling procedure, in the absence of additional annuloplasty, affects primarily the STJ.
Methods for graft sizing
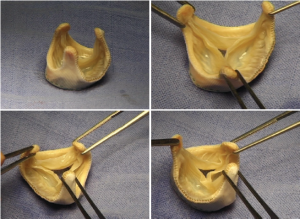
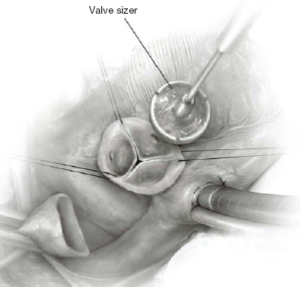
Various approaches have been proposed for graft sizing in valve sparing procedures. One approach relies on the intraoperative assessment of aortic valve function and competence. Valve assessment is performed following the institution of cardiopulmonary bypass and cardioplegic arrest. The aorta is transected 1 cm above the STJ and retraction sutures are placed at each commissure. External dissection of the aortic root is then performed as previously described (4) and the sinuses of Valsalva are resected, leaving behind a 5 mm rim of aortic tissue above the cusp insertion point. The coronary buttons are harvested. Vertical tension is placed on all commissural retraction sutures and the diameter of the STJ is manipulated to approximate a competent aortic valve with good coaptation of all cusps. The STJ diameter is measured using a Hegar dilator or any true size valve sizer (Figure 2). For a remodeling procedure, this is the size of the graft chosen. For a reimplantation procedure, 4-5 mm is added to this number as the graft is placed around the aortic valve. This approach is somewhat subjective and requires judgment and experience on the part of the operating surgeon.
In contrast to the above technique that emphasized a visual assessment of valve anatomy and function, other strategies are based on measurement of certain valve parameters. One technique, proposed by David et al. who pioneered the reimplantation procedure, is to measure the height of each aortic valve cusp, take the average, and multiply it by two. That number reflects the size of graft chosen (5). Another approach that relies on measurement estimates the distance between commissural posts. Assuming that the three posts represent corners of an equilateral triangle, Morishita et al. (6) proposed, based on geometric assumptions of an equilateral triangle, choosing a graft that is 15% greater than the average distance between commissural posts. These approaches will likely work well in the context of a trileaflet valve with reasonable function but would be difficult to apply in a bicuspid aortic valve, or in settings in which there is significant cusp pathology.
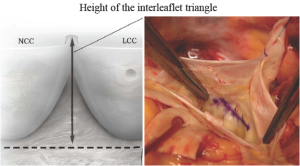
We have proposed a technique for graft sizing that is simple, objective, and reproducible even in the presence of significant root and cusp pathologies and in bicuspid aortic valves (7). Inspired by anatomic and echocardiographic studies of the aortic valve, complemented with our experience with the Valsalva prosthesis, we utilized the height of the interleaflet triangle as a basis for graft sizing. A horizontal line is drawn at the top of the non-coronary/left-coronary commissure and another line is drawn that connects the nadir of the non-coronary and left-coronary cusps (Figure 3). The distance between these two lines represents the height of the interleaflet triangle which, based on anatomic and echocardiographic studies, corresponds to the external diameter of the sinotubular junction of a competent aortic valve. If this distance does not correspond with a labelled graft size, then the next larger graft is chosen.
Implications of graft sizing
While techniques for graft sizing are an important component of valve-sparing procedures, what is of equal and perhaps greater importance is the understanding of the implications of graft sizing for the outcome of the procedure. An important distinction between valve sizing for valve replacement and valve-sparing procedures is that in valve-sparing surgery the graft is not rigid and can be adapted to the valve. Ultimately, the graft size will be a major determinant of the final annular diameter, both of the STJ and the VAJ. Let us consider the implications of incorrect sizing. If the graft size is too small, this will reduce the annular size and the cross-sectional area of the valve. Therefore, the surface area of cusp tissue available will be too large for the new, down-sized annulus and cusp coaptation level of all the cusps will be low, leading to cusp prolapse and aortic insufficiency. Even in cases when there is no significant residual aortic insufficiency, the coaptation reserve of that valve will be small. Some correction of this can be performed by reducing free margin length and elevating the free margin of all the cusps. However, in severe cases of down-sizing, this will typically not be effective and can lead to procedural failure. Having an annulus that is too small such that it results in aortic valve stenosis is a theoretical concern, but rarely observed in the clinical setting.
On the other hand, if the graft chosen is too large, the consequences are less severe. Since the graft is flexible, tying down of the sutures for the proximal suture line will reduce its diameter at the VAJ, thereby adapting it to the valve. With appropriate tailoring of the second suture line, the excess graft material can typically be accommodated to the valve. Having an STJ that is too large can be problematic as it will result in valve cusps stretching outwards and may induce a central coaptation defect. This is easily corrected, however, by using a second smaller graft anastomosed at the level of the STJ. Indeed, this is how the creation of neo-sinuses has been advocated by some surgeons (8). Thus, if one has a choice between a graft that is too small and one that is too large, the larger size is less likely to cause significant problems with valve function.
Another important message related to sizing is that the range of graft sizes used for valve-sparing procedures vary between 26 and 34 mm, with an average between 28 and 30 mm. The extremes of size (i.e. 26 and 34 mm) are rarely used and therefore, the choice is typically between 28-32 mm. Small errors in graft size can induce minor leaflet pathology, most commonly, leaflet prolapse which underscores the need for a thorough valve assessment and correction of cusp pathology following graft implantation. These general principles are applicable to straight Dacron grafts as well as to the Valsalva graft with built-in aortic sinuses.
Lastly, a thorough understanding of graft sizing and its implications can be extremely useful when undertaking more complex repairs of the aortic valve. For example, in cases where leaflet restriction is present (e.g., bicuspid aortic valve with a restrictive raphe), deliberate down-sizing can allow for more cusp tissue to be available to relieve the degree of cusp restriction present.
Conclusions
Graft sizing is an important step in a valve-sparing procedure. Correct graft sizing requires an understanding of normal aortic valve anatomy and the role of the functional aortic annulus. Multiple methods have been proposed for graft sizing - one simple and versatile method relies simply on the measurement of the height of the interleaflet triangle. It is critical to appreciate the implications of graft size on cusp geometry and valve function as this understanding can aid in the correction of errors in sizing and can also facilitate complex aortic valve repairs.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Anderson RH. Clinical anatomy of the aortic root. Heart 2000;84:670-3.
- Boodhwani M, El Khoury G. Aortic Valve Repair. Op Tech Thorac Cardiovasc Surg 2009;14:266-80.
- Kunzelman KS, Grande KJ, David TE, et al. Aortic root and valve relationships. Impact on surgical repair. J Thorac Cardiovasc Surg 1994;107:162-70.
- Boodhwani M, de Kerchove L, El Khoury G. Aortic root replacement using the reimplantation technique: tips and tricks. Interact Cardiovasc Thorac Surg 2009;8:584-6.
- David TE, Feindel CM, Webb GD, et al. Long-term results of aortic valve-sparing operations for aortic root aneurysm. J Thorac Cardiovasc Surg 2006;132:347-54.
- Morishita K, Abe T, Fukada J, et al. A surgical method for selecting appropriate size of graft in aortic root remodeling. Ann Thorac Surg 1998;65:1795-6.
- de Kerchove L, Boodhwani M, Glineur D, et al. A new simple and objective method for graft sizing in valve-sparing root replacement using the reimplantation technique. Ann Thorac Surg 2011;92:749-51.
- Demers P, Miller DC. Simple modification of “T. David-V” valve-sparing aortic root replacement to create graft pseudosinuses. Ann Thorac Surg 2004;78:1479-81.





