Role of paediatric assist device in bridge to transplant
Abstract
Background: While heart transplantation has gained recognition as the gold standard therapy for advanced heart failure, the scarcity of donor organs has become an important concern. The evolution of surgical alternatives such as ventricular assist devices (VADs), allow for recovery of the myocardium and ensure patient survival until heart transplantation becomes possible. This report elaborates the role of VADs as a bridge to heart transplantation in infants and children (≤18 years old) with end-stage heart failure.
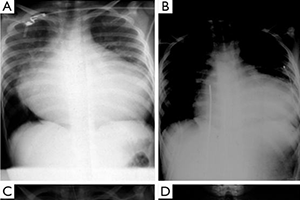
Methods: A retrospective review of the medical records of 201 heart transplant recipients between May 1986 identified 78 children (38.8%; mean age 7.2 (7.8±6.0) years old; IQR: 2.6–11.8 years) with advanced heart failure who were supported with a VAD [left VAD (LVAD) =21; biventricular VAD (BVAD) =57) as a bridge to heart transplantation. Fourteen (17.9%) patients were less than 1 year old; 15 (19.2%) children had a cardiac arrest and underwent cardiopulmonary resuscitation, with 7 of these patients also requiring extracorporeal membrane oxygenation (ECMO) support, prior to implantation of a VAD. The aetiology of heart failure was primarily cardiomyopathy (dilative, restrictive from endocardial fibrosis, idiopathic or toxicinduced), reported in 56 (71.8%) patients. The VADs employed were primarily Berlin Heart EXCOR® (n=63), HeartWare (n=13), Berlin Heart INCOR® (n=1), and Toyobo (n=1).
Results: Mean duration of VAD support was 59 (133.37±191.57) days (range, 1–945 days; IQR: 23–133 days) before a donor heart became available. The primary complication encountered while patients were being bridged to transplant was mediastinal bleeding (7.8%). The main indication for pump exchanges was thrombus formation in the valves. There was no incidence of technical failure of the blood pump or driving system components. Skin infections around the cannulae occurred in 2.5%. Adverse neurological symptoms (thromboembolism 11.1%, cerebral haemorrhage 3.6%) that occurred did not have any permanent neurological sequelae that could be detected on clinical examination in this study. Mean duration of follow-up was 9.4 (10.3±7.6) years (IQR: 3.74–15.14 years). Cumulative survival rates of patients bridged to transplantation with VAD were 93.6±2.8%, 84.6±4.1%, 79.1±4.7%, 63.8±6.2%, 61.6±7.1%, and 52.1±9.3% at 30 days, 1, 5, 10, 15 and 20 years, respectively. There was no statistically significant difference (P=0.79) in survival rates of patients bridged to heart transplantation with VAD compared to those who underwent primary heart transplantation. Post-transplant survival rates stratified according to the type of VAD implanted and number of ventricles supported were not statistically different (P=0.93 and 0.73, respectively). In addition, post-transplant survival rates were not significantly different when age, gender and diagnosis were adjusted for. Furthermore, no statistically significant difference was found when posttransplant survival rates of children who had episodes of rejection were compared to those who did not have episodes of rejection.
Conclusions: The results in this series demonstrate that VADs satisfactorily support paediatric patients with advanced heart failure from a variety of aetiologies until heart transplantation. The data further suggests that patients bridged with VADs have comparable long-term post-transplant survival as those undergoing primary heart transplantation.
Cover