After 50 years, a personal reflection on the development of internal thoracic artery (ITA) grafting
Fifty years of internal thoracic artery (ITA) grafting: a personal reflection
Full appreciation of the history of ITA grafting requires recognition of the persistent work of Arthur Vineberg [1903–1988]. Based on his studies of myocardial anatomy, Vineberg believed that implantation of the bleeding ITA into heart muscle would create a new collateral blood supply to the heart. He chose the ITA because his studies had convinced him that it rarely was affected by atherosclerosis. His experimental work in dogs began in 1945 (1). He supported his contention by postmortem injections of radio opaque medium into the implanted ITAs. On some occasions, the opaque medium was visualized in distal coronary arterial segments (2). Connections to these arterial segments were arteriolar (0.001 mm). Vineberg’s critics considered the postmortem arteriographic findings to be pressure artifacts.
In 1958, Mason Sones [1919–1985], newly appointed to the Cleveland Clinic, discovered and then refined the technique of selective coronary arteriography (3). In 1962, Sones selectively opacified ITAs implanted by the Vineberg technique. Most were patent. A few communicated with distal coronary segments (4). Sones and the cardiac surgical department directed by Donald B. Effler broadened the study to determine by pre- and postoperative angiography which patients would benefit from ITA implants. By 1965, analysis of the data confirmed that most implants were patent, but in only about 30 percent of patients were distal coronary arterial segments also visualized. The unvisualized connections were arteriolar (0.001 mm). Patients who did benefit had collateral connections (arteriolar) to distal coronary segments prior to operation. ITA implants increased this collateral circulation. The time required for new circulation ranged from weeks to three months. Effler was invited by the American Heart Association to present these data (5) at its annual convention, which was held in 1965 in Miami Florida.
I was attending that meeting to present data confirming Jacobson’s contention that with the high magnification of the surgical microscope blood vessels of 1 mm in diameter could be anastomosed with consistent success (6). My surgical interest at that time was using the technique to revascularize free grafts of jejunum transposed to the neck to replace segments of cervical oesophagus (7). Listening to Effler describe communications (arteriolar) which could develop between the implanted ITA and distal coronary branches, I thought of anastomosing the ITA directly to a distal coronary segment. The large clinical experience presented by Effler left no doubt that arteriolar connections could alleviate ischemic heart disease. The drawbacks to the procedure were the requirement for preexisting collaterals and the prolonged time required for development of the connections. I was sure that using the surgical microscope the ITA could be anastomosed to a distal coronary segment 1mm in diameter. Such an anastomosis would be effective from the moment of completion.
ITA-coronary artery anastomosis was first reported from the experimental laboratory in 1956 (8). It was repeated by many surgeons in many laboratories with many techniques, and in 1964 was reported in conjunction with the use of the heart lung machine (9). All these demonstrations were anastomoses of the ITA to proximal coronary segments, approximately 3 mm in diameter. Misunderstanding statements about the proximal location of coronary occlusions may have led to this perseverative work. Although major occlusions usually were proximal, atherosclerotic thickening extended well beyond them. These thickenings were the basis of Szilagyi’s warning that bypass surgery would require anastomosis to vessels 2 mm or less in diameter (10).
In 1965, I began a project of ITA anastomosis to 1-mm distal left anterior descending (LAD) segments. The project included proximal LAD ligation, blood flow measurement early and late after anastomosis, and late postoperative (8 months) cineangiography. The success of these experiments brought me to grips with clinical application. Despite the fact that I had conducted the work in the surgical laboratory of New York University, permission for clinical application at New York University was denied in September of 1967. The story of the search for a place for clinical application illuminates surgical thinking of the time. ITA implantation had become accepted and was performed in most university centers. It was so firmly established that extensions of ITA implants were attempted with implants of the intercostal artery (11), the right gastroepiploic artery (12) and the splenic artery (13). By contrast, direct microsuture anastomosis using the surgical microscope was not considered clinically feasible. Most of my letters of inquiry went unanswered, but there were some respondents. C. Walton Lillehei, the dynamic pioneer of cardiac surgery, was encouraging but was in the process of leaving the University of Minnesota to become Chairman of the Department of Surgery at New York Hospital of the Cornell Medical Center and wrote that he could not in transition sponsor any new projects. Adrian Kantrowitz thought the data interesting but wanted the experiments repeated in his laboratory. At Sones’ urging Donald Effler invited me to show him the postoperative cineangiograms; Dr Effler was impressed and favoured clinical application at the Cleveland Clinic, but wanted me to do so as his resident. Michael DeBakey did not reply to the letter but during one of his visits to New York City an introduction was arranged. He listened closely to my proposal. His reply was definitive: clinical application was impossible, coronary bypass surgery was not feasible.
Many years later, DeBakey claimed precedence in coronary bypass surgery contending that he had performed the first successful coronary bypass operation in 1964 (14). In 1964, Dr. Edward Garrett was Dr. DeBakey’s associate. In conversation, Garrett told me that a patient with intractable angina had been referred to Dr. DeBakey for ITA implant surgery. Angiography showed severe left main coronary stenosis. DeBakey instructed Garrett to discharge the patient from the surgical service as he left Houston for a scheduled external lecture. While DeBakey was away the patient was readmitted to the hospital because of unstable angina. The cardiologist urged Garrett to undertake surgical intervention. Garrett explained that no benefit would come from an ITA implant for many weeks and the procedure was inappropriate for the patient. The cardiologist then suggested endarterectomy. Angiography had shown the left main coronary stenosis to be of short extent. Garrett replied that the surgical risk of endarterectomy would be 50 percent. The cardiologist thought that acceptable and so did the desperate patient. Surgery was scheduled. Garrett said it was quickly apparent that what seemed like a short left main coronary stenosis by angiography was in fact severe atherosclerotic change extending into both the anterior descending and circumflex arteries. He knew successful endarterectomy could not be done, but something now had to be done. He had done saphenous vein bypasses to distal tibial arteries. He prepared a saphenous vein segment, sewed one end to the aorta, made an incision in a soft section of the anterior descending artery and sewed the saphenous vein graft to it. The patient did well. When Dr. DeBakey returned the patient was ready for discharge from the hospital. Garrett explained the situation to Dr. DeBakey. DeBakey then told Garrett to schedule three patients for him to operate. Garrett did so. Those patients died. Dr. DeBakey forbade any further such surgery.
Two random events suddenly opened the way for clinical application of ITA-LAD anastomosis. First, the explosive impact of heart transplantation reported in December of 1967 made other cardiac procedures seem minor by comparison. Then, in December of 1967, The Journal of Thoracic and Cardiovascular Surgery published a report by the Russian surgeon Vladimir Kolessov of successful ITA-LAD anastomosis in six patients (15).
Although the procedure had been prohibited at the New York University Hospital, Dr. David Tice, Director of Surgery at the affiliated New York Veterans Administration Hospital, invited me to do it there. I did the first ITA-LAD anastomosis in the United States there in February of 1968. During that same month Bailey and Hirose did the first ITA suture anastomosis to right coronary using the right ITA (16).
Although Sones had discovered coronary arteriography in 1958 and by 1968 had brought it to a very high point, few laboratories could match his capability. In the New York city area coronary arteriography could define proximal areas of obstruction but rarely defined the status of the distal circulation. Postmortem studies had made it clear to me that although severe areas of proximal atherosclerosis were prominent, other areas extended well beyond the proximal obstruction in skip-like fashion. Placing a graft between two areas of stenosis seemed less sensible than placement far distally beyond the last atherosclerotic stenosis. My choice was placement of the ITA graft to the distal third of the LAD, usually a normal thin walled segment about 1.5 mm in diameter. My expectation was not to achieve normal myocardial perfusion but to augment flow to the ischaemic myocardium. In 1968, I operated on eighteen patients. Although all were desperately ill, no operating room fatalities occurred. Nevertheless, there were six early postoperative deaths. Postmortem examination showed patent ITA anastomoses but severe triple vessel disease.
In June of 1968 saphenous vein graft to the right coronary artery (RCA) was reported by Favaloro. I combined it with ITA anastomosis to the LAD. Although Bailey and Hirose had described right ITA artery to right coronary anastomosis in 1968, I was reluctant to use that procedure because the RCA is much larger than the ITA. The size mismatch of small ITA to large RCA would cause turbulence of flow at the anastomosis. I feared this would make anastomotic stenosis likely. Skill in very high mobilization of the ITA and routing it parallel to the phrenic nerve so that it could reach the posterior descending artery (PDA) was to come later, as was the use of free ITA grafts arising from the aorta.
In 1969, I began to perform anastomoses to the circumflex artery, and with the advent of triple bypasses the problem of early postoperative mortality was resolved (17). By 1969, several centers were performing coronary bypass surgery. Most used only saphenous vein grafts. I was considered odd for persisting in the use of the ITA. I persisted because in my practice when angina recurred, angiography almost invariably showed saphenous vein graft stenosis or occlusion to be the cause of the recurrent angina. Therefore, despite criticism I continued to use the ITA on a routine basis for anastomosis to the LAD. By then several other surgeons felt that ITA grafts would prove to be preferable to saphenous vein grafts. Earle Kay felt so strongly that he initiated the use of both ITAs as grafts and reported a series in 1974 (18).
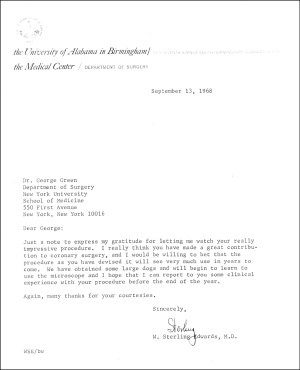
Sterling Edwards, a vigorous proponent of ITA grafts and use of the surgical microscope initiated the additional use of the splenic artery pedicled graft in 1973 in to achieve triple bypass using arteries only (19). Between 1972 and 1975, Edwards performed 15 splenic artery anastomoses. In 1973, while mobilizing the splenic artery he encountered an aneurysmal segment of the splenic artery. In its stead he mobilized and used the right gastroepiploic artery as a graft to the right coronary. He found the right gastroepiploic much easier to mobilize than the splenic and he found it to be of adequate size. He did not report the use of it. In 1974, he accepted the Chairmanship of the Department of Surgery at the University of New Mexico. In this capacity he found he could no longer practice both cardiac and vascular surgery and discontinued cardiac surgical practice in 1975.
Edwards commanded great respect in the cardiac surgical community. It had been because of his early enthusiasm and support (Figure 1) that I was allowed to extend my work to the New York University Hospital.
His prestige was such that that had he continued in cardiac surgical practice I believe the surgical microscope would have come into general use. He joked that I had seriously interfered with the work of his vascular surgery laboratory by introducing him to the microscope. His standard model for creating and studying arterial thrombosis had been endarterectomy of the canine superficial femoral artery. He told me that performing endarterectomy with a microscope ruined the model by eliminating thrombosis.
At the urging of Mason Sones, Floyd Loop began to use the ITA graft. To extend its use he introduced the free ITA graft, detached from its subclavian origin and anastomosed to the ascending aorta (20). This anastomosis was demanding because of the marked difference in thickness of the aorta and the ITA. Following the crowd, Loop ignored the need for high magnification. To resolve this problem Hendrick Barner recommended anastomosing the ITA to the hood of the vein graft (21) and George Schimert recommended anastomosing it to a vein patch in the aorta (22). Because of the difficulty of handling the thin walled and friable ITA, Alain Carpentier introduced the radial artery free graft in 1973 (23). He hoped it would have the advantages of the ITA graft and the advantage of being much easier to handle because of its thicker wall. It soon appeared that radial artery grafts were subject to a prohibitive incidence of fibrotic stenosis and occlusion, 75 per cent within one year (24). They were largely abandoned by 1990. Later renewed use and re-evaluation was based on the possible protective effect of calcium blocking agents.
Even enthusiasts of arterial grafting acknowledged that the ITA was a far more demanding graft than the saphenous vein. As skilled a surgeon as Favaloro wrote in 1970: “It is highly doubtful that full clinical application of this procedure will reach a large scale: the anastomosis is extremely difficult to perform mostly because of the fragile wall of the internal mammary artery rather than the coronary artery itself, and the limitation of the size of the anastomosis by the caliber of the internal mammary artery in its distal portion” (25).
Favaloro’s statement highlights the difference in technique required for ITA grafts as compared to the saphenous vein grafts that he pioneered at the Cleveland Clinic. As I observed at the Cleveland Clinic, that technique (using little or no magnification) was based on placement of interrupted sutures deep into the saphenous vein, shallowly into the coronary artery and deeply into surrounding epicardium. Placement of sutures deep into the ITA will result in anastomotic stricture. The ITA does not have sufficient size to be spatulated under a cuff of epicardium. Precision of approximation to a small coronary segment increases with increasing magnification. The difficulty of this anastomosis led to a damping of enthusiasm for it. In 1975, Claude Grondin expressed these reservations because in his hands ITA patency was no better than saphenous vein graft patency one year after operation (26). Issues of surgical technique were not considered. Between 1976 and 1983 few surgeons used the ITA.
In 1970, I left New York University to initiate the coronary surgery program at St. Luke’s Hospital. Simultaneously a clinical follow-up program was initiated by Dr. Airlie Cameron of the Division of Cardiology. Soon thereafter, Dr. Julio Sosa who had worked with Sones during the development of coronary angiography, and who had participated in the first angiographic studies of ITA implants, expressed interest in referring patients to me for ITA anastomosis and restudying them after ITA anastomosis. The restudies were not done arbitrarily. They were done to evaluate recurrence of angina, recurrent myocardial infarction, or signs of ischemia on electrocardiographic stress tests. Few restudies were performed prior to 1975. During the latter part of the decade restudies became more frequent. By 1981, Sosa had restudied 37 patients who had both ITA and saphenous vein grafts. The mean time following operation was seven years. Analysis of the data was striking: 94 percent of the ITA grafts were widely patent; 50 percent of the saphenous vein grafts were occluded and 50 percent of those patents showed atherosclerotic stenosis within the body of the graft. In 1981, the data was submitted for presentation at the annual meeting of the American Association for Thoracic Surgery. It was not selected for presentation. I was persistent and submitted the data again in 1982. The resubmission was selected, presented in spring of 1983 and published later that year (27). By then similar angiographic studies had come from Montreal. In 1984 Grondin, whose 1975 publication dampened enthusiasm for ITA grafts, reversed his position and became a champion of the procedure (28). The use of sequential ITA grafts was described by Tector in 1984 (29) and John Pym described the use of the right gastroepiploic artery for anastomosis to the distal RCA in 1987 (30).
In 1985, Cameron collated the 15-year follow-up data of the 748 patients operated at St. Luke’s Hospital between 1970 and 1973. There was a highly significant advantage conferred to those patients who had single ITA anastomosis in combination with saphenous vein grafts as compared to those who had saphenous vein grafts alone. There was even further advantage to those patients who had bilateral ITA grafts (31). The number of patients having bilateral ITA anastomoses was too small to reach statistical significance but I found the trend compelling. I was eager to understand why ITA grafts fared so much better than saphenous vein grafts.
One obvious difference between the vein graft and the ITA graft was that of nutrient vessels. All vasa vasorum were disrupted in the process of removing a saphenous vein graft from the leg. It was known to take many weeks before nutrition of the wall of the vein graft was reconstituted. This seemed a plausible explanation for the 10 percent of saphenous grafts that suffered early fibrotic occlusion, but the explanation for late atherosclerosis which affected the majority of saphenous vein grafts was not apparent until the publication of the work of Frank Sims [1921–2013]. Sims, a pathologist, accepted the resistance of the ITA to atherosclerosis as a known fact. Wanting to study the incidence and severity of coronary atherosclerosis in residents of the Fiji islands he used each subject’s ITA as a standard of normality and then compared the intimal thickness of the coronary to that of the ITA, in age groups ranging from the first to the eighth decade. In so doing he noticed that the defining boundary between the intima and the media, the internal elastic lamina (IEL), was radically different in ITAs from that in the coronaries (32). The IEL of the ITA was usually dense and unbroken. The IEL of the coronary was usually fragmented. Smooth muscle cells migrated through gaps in the IEL and changed from a synthetic to a hyperplastic mode in their new locale. He later showed that endothelium of ITAs was stable. Endothelium anchored to the IEL. When the IEL was broken and discontinuous endothelial slough ensued. He showed that all the arteries of domestic animals are similar to the ITA. Human arteries are similar to the coronary. Human veins have even more deficiencies of IEL than human arteries (33).
I had avoided using free grafts of the ITA because I feared that the disruption of the pedicled graft would make it no better than saphenous vein grafts. Sims’ emphasis on the internal structure of the vessel caused me to think again. Loop had introduced the use of the free ITA graft in 1973. In 1985, I was eager to know if there had been late studies of these grafts. Did they become atherosclerotic? Loop, then in the process of evaluating the late studies, assured me there were no signs of atherosclerotic change. Nor had there been fibrous strictures as had occurred in radial artery grafts. He confided that anastomotic stricture at the aorta had been a problem. The absence of early stricture in free ITA grafts was striking. I had thought such stricture in saphenous vein grafts as well as in radial artery grafts were a consequence of disruption of vasa vasorum. I undertook a small study of vasa vasorum of ITAs in comparison to radial arteries. Injection of barium gel into ITAs revealed multiple prominent branches throughout their length. Histological study of these same vessels revealed the vasa vasorum of the adventitia of the ITAs to be filled with the barium. Clearly the vasa vasorum of the ITA originated within 2 mm of the origins of its own branches. As soon as an ITA graft was anastomosed to the aorta the nutrition of its wall would be restored. In contrast, radial arteries showed no prominent branches and vasa vasorum were not filled by injection of the artery. Moreover, the IEL of the radial artery did not have the integrity of the ITA. Cameron’s clinical follow-up studies of pedicled ITA grafts, Loop’s angiographic follow-up studies of free ITA grafts (34) and the logic of Sims’ studies compelled me to resolve to evaluate the use of ITAs for as many grafts as feasible in all patients, using free grafts when pedicle grafts were not feasible, and including the use of sequential techniques.
Putting that resolution into practice was relatively easy in 1985 because enthusiasm for arterial grafting in both the cardiologic and cardiac surgical communities was growing. Synchronous with Cameron’s (15-year) study from Saint Luke’s in New York, a similar (10-year) study from the Cleveland Clinic was published (35). Robert Dion’s work on the broad application of bilateral and sequential grafts was published in 1989 (36).
Recognition of the superiority of the ITA graft created such a demand for its use that it became the standard graft to the all-important LAD in many surgical practices. Because the ITA graft remains patent even if its anastomotic site to the LAD is stenotic, angiographic scrutiny of the surgical result may not have been optimal, but it did show ITA narrowing that were usually called “spasm” limiting blood flow and causing “hypoperfusion”. “Spasm” may well have been late stricture caused by damage to the ITA during mobilization or rupture of the IEL by forceful dilatation (mechanical or hydrostatic) prior to anastomosis. Such dilatation was advocated by many surgeons.
The small size of the ITA also posed problems to its mobilization from the chest wall. Too often, instead of meticulous mobilization within 2 mm (37) of the ITA a broad pedicle was quickly mobilized using high intensity cautery. This left devitalized tissue on the chest wall, impaired blood flow to the sternum, and may have been the cause of high rates of postoperative sternal dehiscence and mediastinal infection reported by some surgeons.
The first study that statistically demonstrated the clinical advantage of bilateral ITA grafts was that of Earle Kay (18). It was based on surgery performed in 1972 when mobilization of the ITA to its origin from the subclavian artery and avoiding damage the nearby phrenic nerve had not been perfected. Nor had proper routing of pedicle grafts to posterior areas of the heart. More dramatic advantage of multiple ITA grafts including free and sequential grafts was published in 1994 (38). It reported a consecutive series of 143 patients requiring multiple grafts. Three hundred and seventeen of the 441 anastomoses were constructed from ITAs. Of the 143 patients 103 had bilateral, 51 sequential and 49 free ITAs grafts. During 5 years of follow-up, postoperative angina and myocardial infarction were significantly more common in those patients who had been operated with just one ITA compared to those who received multiple ITA grafts. Use of the operating microscope at 8–12× magnification was essential to these anastomoses. By first anastomosing the free ITA to the aorta unrestricted blood flow into the ITA was ascertained.
Currently, increasing numbers of surgeons are using the surgical robot. The robot uses adjustable, high magnification (10–15×) but the surgeon loses the sensory feedback of her/his hands in order to have the use of that high magnification. Although the surgical microscope is now used in most surgical specialties and it affords both the sensory feedback of the surgeon’s hands and the advantages of high magnification, it is still rarely used by cardiac surgeons. For a specialty that led in surgical innovation, this seems a paradox.
Postscript
Dr. George Green has presented his carefully documented personal memories of the development of ITA grafting. He played a critical role himself in this grand saga, having performed the first ITA-LAD anastomosis in the United States in 1968. In 1970 he introduced coronary surgery to Saint Luke’s Hospital in New York City, where I now have the privilege of leading the Department of Cardiovascular Surgery.
Dr Green’s story is one of rigorous step-wise scientific inquiry; his first clinical application of ITA grafting was preceded by careful histological and animal surgical studies. Those preclinical experiments followed careful learning about the predicate Vineberg procedure and a thorough understanding of the nascent field of graft angiography. He adopted newly available technology, including operating microscopes, to perfect his ability to construct reliably patent vascular anastomoses with 1-mm vessels. Having applied his new technique clinically, he consistently studied his clinical outcomes and refined his technique relentlessly, including a rapid push to graft all three territories of the coronary system, which yielded a striking improvement in early operative mortality. He persisted in studying the limitations of ITA grafting and arterial grafting in general, expanding application of these techniques while continuously monitoring his clinical outcomes. His report in 1986 of 15-year outcomes with ITA grafting remains a seminal publication in the field of surgical coronary revascularization. His dedication to innovation, despite harsh criticism and significant political obstacles, is an inspiration to all those who seek to improve the care of patients with cardiovascular disease.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Vineberg AM. The development of an anastomosis between the coronary vessels and a transplanted internal mammary artery. Can Med Assoc J 1946;55:117-9. [PubMed]
- Vineberg A. Coronary vascular anastomoses by internal mammary artery implantation. Can Med Assoc J 1958;78:871-9. [PubMed]
- Sones FM Jr, Shirey EK. Cine coronary arteriography. Mod Concepts Cardiovasc Dis 1962;31:735-8. [PubMed]
- Green GE, Singh RN, Sosa JA. Surgical Revascularization of the heart: the internal thoracic arteries. New York: Igaku-Shoin, 1991:12.
- Effler DB, Sones FM, Groves LK, et al. Myocardial revascularization by Vineberg’s internal mammary artery implant: evaluation of postoperative results J Thorac Cardiovasc Surg 1965;50:527-33. [PubMed]
- Green GE, Som ML, Wolff WI. Experimental microvascular suture anastomosis. Circulation 1966;33:I199-203. [Crossref] [PubMed]
- Green GE, Som ML. Free grafting and revascularization of intestine. I. Replacement of the cervical esophagus. Surgery 1966;60:1012-6. [PubMed]
- Absolon KB, Aust JB, Varco RI, et al. Surgical treatment of occlusive coronary disease by endarterectomy or anastomotic replacement. Surg Gynecol Obstet 1956;103:180-5. [PubMed]
- Spencer FC, Young NK, Prachmusbmoh K. Internal mammary –coronary artery anastomosis performed during cardiopulmonary bypass. J Cardiovasc Surg (Torino) 1964;5:292-7. [PubMed]
- Szilagyi DE, McDonald RT, France LT. The applicability of angioplastic procedures in coronary atherosclerosis. An estimate through postmortem injection studies. Ann Surg 1958;148:447-61. [Crossref] [PubMed]
- Pearce CW, Hyman AL, Brewer P, et al. Myocardial revascularizatiion: Implantation of intercostal artery J Thorac Cardiovasc Surg 1966;52:809-12. [PubMed]
- Bailey CP, Hirose T, Brancato R, et al. Revascularization of the Posterior (Diaphragmatic) Portion of the Heart. Ann Thorac Surg 1966;2:791-805. [Crossref]
- Bloomer WE, Beland AJ, Cope J. Clinical use of the splenic artery for myocardial revascularization. Technical considerations. Ann Thorac Surg 1968;5:419-28. [Crossref] [PubMed]
- Garrett HE, Diethrich EB, DeBakey ME. Aortocoronary bypass with saphenous vein graft. Seven-year follow-up. JAMA 1973;223:792-4. [Crossref] [PubMed]
- Kolessov VI. Mammary artery-coronary artery anastomosis as method of treatment for angina pectoris. J Thorac Cardiovasc Surg 1967;54:535-44. [PubMed]
- Bailey CP, Hirose T. Successful internal mammary-coronary arterial anastomosis using a ‘minivasular’ sutureing technique. Int Surg 1968;49:416-27. [PubMed]
- Green GE, Spencer F, Tice DA, et al. Arterial and venous microsurgical bypass grafts for coronary artery disease. J Thorac Cardiovasc Surg 1970;60:491-503. [PubMed]
- Kay EB, Naraghipour H, Beg RA, et al. Internal mammary artery bypass graft--long-term patency rate and follow-up. Ann Thorac Surg 1974;18:269-79. [Crossref] [PubMed]
- Edwards WS, Lewis CE, Blakely WR. Coronary artery bypass with internal mammary and splenic artery grafts. Ann Thorac Surg 1973;15:35-40. [Crossref] [PubMed]
- Loop FD, Spaminato N, Cheanvechai C, et al. The free internal mammary artery bypass graft. Use of the IMA in the aorta –to-coronary artery position. Ann Thorac Surg 1973;15:50-5. [Crossref] [PubMed]
- Barner HB. The internal mammary artery as a free graft. J Thorac Cardiovasc Surg 1973;66:219-21. [PubMed]
- Schimert G, Vidne BA, Lee AB Jr. Free internal mammary artery graft. An improved surgical technique. Ann Thorac Surg 1975;19:474-7. [Crossref] [PubMed]
- Carpentier A, Guermonprez JL, Deloche A. The aorta-to-coronary radial artery bypass graft. A technique avoiding pathological changes in grafts. Ann Thorac Surg 1973;16:111-21. [Crossref] [PubMed]
- Curtis JJ, Stoney WS, Alfred WCJ. Inimal hyperplasia: a cause of radial artery aorto-coronary bypass graft failure. Ann Thorac Surg 1975;20:628-35. [Crossref] [PubMed]
- Favaloro RG. Surgical treatment of coronary arteriosclerosis. Baltimore: Williams and Wilkins, 1970.
- Grondin CM, Lesperance J, Bourassa MG, et al. Coronary artery grafting with the saphenous fein or internal mammary artery. Ann Thorac Surg 1975;20:605-18. [Crossref] [PubMed]
- Singh RN, Sosa JA, Green GE. Long-term fate of the internal mammary artery and saphenous vein grafts. J Thorac Cardiovasc Surg 1983;86:359-63. [PubMed]
- Campeau L, Enjalbert M, Lespérance J, et al. Atherosclerosis and late closure of aortocoronary saphenous vein grafts: sequential angiographic studies at 2 weeks, 1 year, 5 to 7 years, and 10 to 12 years after surgery. Circulation 1983;68:II1-7. [PubMed]
- Tector AJ, Schmahl TM, Canino VR, et al. The role of the sequential internal mammary artery grafts in coronary surgery. Circulation 1984;70:I222-5. [PubMed]
- Pym J, Brown PM, Charette EJ. Gastroepiploic-coronary anastomosis. J Thorac Cardiovasc Surg 1987;94:256-9. [PubMed]
- Cameron A, Kemp HG Jr, Green GE. Bypass surgery with the internal mammary artery graft: 15 year follow-up. Circulation 1986;74:III30-6. [PubMed]
- Sims FH. A comparison of coronary and internal mammary arteries, and implications of the results in the etiology of atherosclerosis. Am Heart J 1983;105:560-6. [Crossref] [PubMed]
- Sims FH. The pathology of the internal thoracic artery and its contribution to the study of atherosclerosis. In: GE Green, RN Singh, JA Sosa. Surgical revascularization of the heart: the internal thoracic arteries. New York: Igaku-Shoin, 1991:18-62.
- Loop FD, Lytle BW, Cosgrove DM, et al. Free aorta-coronary internal mammary artery graft. Late results. J Thorac Cardiovasc Surg 1986;92:827-31. [PubMed]
- Loop FD, Lytle BW, Cosgrove DM, et al. Influence of the internal mammary artery graft on 10-year survival and other cardiac events. New Engl J Med 1986;314:1-6. [Crossref] [PubMed]
- Dion R, Verheist R, Rouseau M. Sequential mammary grafting J Thorac Cardiovasc Surg 1989;98:80-8. [PubMed]
- Green GE, Swistel DG, Castro J, et al. Sternal blood flow during mobilization of the internal thoracic arteries. Ann Thorac Surg 1993;55:967-70. [Crossref] [PubMed]
- Green GE, Cameron AC, Goyal A, et al. Five-year follow-up of microsurgical multiple internal thoracic artery grafts. Ann Thorac Surg 1994;58:74-8. [Crossref] [PubMed]