Overall Essen’s experience with the E-vita open hybrid stent graft system and evolution of the surgical technique
Abstract
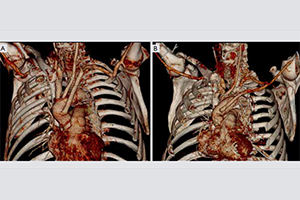
Background: The hybrid stent graft prosthesis E-vita open was designed and introduced by us in 2005 to avoid a two-stage surgical approach in the surgical treatment of complex thoracic aortic disease. Experience in ascending aortic and arch replacement with simultaneous stent grafting of the descending aorta was accumulated over the past 8 years. Facilitation of surgical technique by moving the distal suture line from Zone 3 into Zone 2 took place in 2009. We report our mid-term single-center experience comparing both surgical periods.
Methods: Between January 2005 and July 2013 a total of 132 patients (mean age 59±11 years) underwent one stage surgery for acute (AAD, n=74), chronic aortic dissection (CAD, n=35) or an extensive thoracic aortic aneurysm (TAA, n=23). Patients were separated in two groups according to distal anastomosis level in Zone 2 (Z2, 41/132) and Zone 3 (Z3, 91/132). Outcome, ischemic and operative times as well as adverse events were monitored during follow up.
Results: Overall in-hospital mortality was 13% (17/132) without difference between the groups. However, Zone 2 anastomosis resulted in reduction of cardioplegic arrest (117±39 vs. 147±35 minutes; P<0.001), selective cerebral perfusion (52±15 vs. 68±18 minutes; P<0.001) and visceral ischemic time (51±19 vs. 72±23 minutes; P<0.001). The incidence of postoperative temporary hemodialysis decreased from 40% to 20% in Z2 (P=0.028), postoperative re-exploration rate from 15% to 2% (P=0.037). No difference was found in dissection with complete false lumen thrombosis in 83% (90/109) within 10 days, as well as in TAA, where 100% aneurysm exclusion was observed. Three-year survival, freedom from thoracoabdominal aortic surgery and endovascular repair was 93%, 88%, 88%, respectively. Overall 5 year survival was 76% in AAD, 85% in CAD and 79% in TAA patients.
Conclusions: The dimension of surgery could be successfully reduced, indicated by significantly shortened ischemic times and postoperative complications. Durable one-stage repair of complex thoracic aortic disease could be achieved in the majority of cases with acceptable mortality. Distal reintervention is infrequent but associated with low risk when indicated.
Cover