Importance of entry tears in Type B aortic dissection prognosis
Introduction
Acute type B aortic dissection (ABAD) is the most common aortic catastrophe, and is associated with high mortality rates. Besides clinical predictors, recent reports have also analyzed morphologic predictors for adverse outcomes and aortic growth. Indeed, clinical and bioengineering studies have shown that elevated pressure in the false lumen may result in increased aortic growth (1,2). The pressure in the false lumen is related to its inflow and outflow, and therefore the number of entry tears detected between the true and false lumens may be important in predicting the degree of aortic dilatation in the long term. The goal of this study was to investigate whether the number of identifiable entry tears is associated with aortic growth in long-term ABAD (3-5).
Patients and setting
Patients
We retrospectively analyzed all computed tomographic angiography (CTA) data of ABAD patients who were medically treated in four referral centers between 2005 and 2010.
Interventions
All ABAD patients received medical anti-hypertensive therapy according to the local protocol.
Objectives
To investigate whether the number of identifiable entry tears is associated with aortic growth in medically treated ABAD patients.
Methodology
All ABAD patients included in this study had a CTA obtained within 7 days of the initial diagnosis (baseline CTA) and a second CTA (follow-up CTA) obtained at least 3 months after the baseline CTA and before any possible intervention. The presence and number of entry tears between the true and false lumens were investigated on the baseline scan. An entry tear was defined as a discontinuity of the aortic flap with a clear flow of contrast between the true and false lumens on at least 2 different views (transversal, coronal, sagittal, or center vessel reconstruction). A center-line vessel reconstruction was obtained in all baseline CTA scans and the aortic diameter was measured at 5 different levels: 2 cm below the origin of the left subclavian artery (LSCA), 10 cm below the LSCA, 20 cm below the LSCA, 8 cm below the most distal renal artery and at the level of the largest point of the descending aorta. Annual growth rates were calculated by dividing the difference between the diameter on the baseline scan and the diameter on the last available CTA scan by the time interval between the 2 CTAs.
Results
Main results
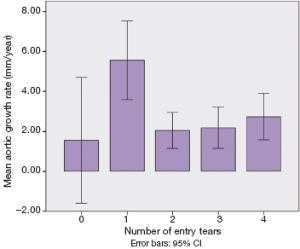
A total of sixty patients (39 male; median age at presentation 59.7 years; range 37.0-82.6 years) were included in this study with a median follow-up of 22 months (range, 3-130 months). One entry tear was present in 20 patients (33.3%), two were present in 19 patients (31.6%), three were present in 15 patients (25%), four or more entry tears were observed in 2 patients (3.3%), and no detectable entry tears were seen in 4 patients (6.7%). A total of 243 (81%) of the 300 analyzed aortic segments were dissected. The mean initial diameter was 36.1±9.5 and mean final diameter 40.3±11.2, resulting in a mean aortic growth rate of 3.3±6.3 mm/year. Based on our analysis of dissected aortic segments, aortic growth rates were significantly affected by the number of entry-tears (P=0.003). In patients with one visible entry tear, the aortic growth rate (median =5.8 mm/year) was significantly higher compared to that in patients with two entry tears (median =0.98 mm/year: P=0.01) and patients with three entry tears (median =1.31 mm/year, P=0.010) (Figure 1). Patients with four entry tears (median =2.50, P=0.992) or without visible entry tears (median =1.60 mm/year, P=0.156), which had a relatively low number of segments, did not show a significant difference in growth rate when compared to patients with one entry tear. There was good intra-observer agreement (80%) with a kappa coefficient value of 0.73, while the inter-observer agreement (75%) had a kappa coefficient of 0.65.
Study limitations
A major limitation of this study was that clinical information of the study population was unavailable, and thus a certain number of entry tears may possibly have been missed on the baseline CTAs. Additionally, entry tears can be smaller than the slice thickness of our CTA scans and other imaging predictors such as the size of the entry tears may influence aortic growth.
Generalizability to other populations
These findings are not only important in ABAD patients, but are also of significance in patients with type A aortic dissections treated with a frozen elephant trunk. The distal extent of the stent-graft remains debated and this study shows that the surgeons should make an effort to cover all detectable entry tears when possible.
Clinical bottom-line
Conservatively treated ABAD patients with one entry tear present with higher aortic growth rates and may therefore benefit from stricter surveillance and early prophylactic intervention.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Erbel R, Alfonso F, Boileau C, et al. Diagnosis and management of aortic dissection. Eur Heart J 2001;22:1642-81. [PubMed]
- Nienaber CA, Eagle KA. Aortic dissection: new frontiers in diagnosis and management: Part II: therapeutic management and follow-up. Circulation 2003;108:772-8. [PubMed]
- Tsai TT, Evangelista A, Nienaber CA, et al. Partial thrombosis of the false lumen in patients with acute type B aortic dissection. N Engl J Med 2007;357:349-59. [PubMed]
- Sueyoshi E, Sakamoto I, Uetani M. Growth rate of affected aorta in patients with type B partially closed aortic dissection. Ann Thorac Surg 2009;88:1251-7. [PubMed]
- Tolenaar JL, van Keulen JW, Trimarchi S, et al. Number of entry tears is associated with aortic growth in type B dissections. Ann Thorac Surg 2013;96:39-42. [PubMed]





