Frozen elephant trunk surgery using the Vascutek Thora-flex hybrid prosthesis
Introduction
The Vascutek Thoraflex hybrid graft (Vascutek, Scotland) is a novel commercially available 4-branched frozen elephant trunk (FET) graft used to treat patients with extensive diseases of the thoracic aorta (1).
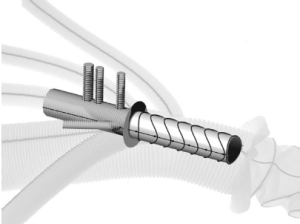
This hybrid prosthesis is composed of a distal endograft sealed to a proximal 4-branched gelweave graft with an incorporated sewing collar (Figure 1).
The text of this manuscript describes our FET technique with the Vascutek Thoraflex hybrid graft in detail (Video 1).
Clinical vignette
A 73-year-old man who had undergone a supra-coronary ascending aorta replacement for a DeBakey type 1 acute aortic dissection in a different Institution in 1997 was recently referred to our hospital for a residual chronic post-dissection aneurysm of the thoraco-abdominal aorta. Upon admission, the angio CT scan showed severe dilatation of the thoracic (48 mm) and abdominal (72 mm) aorta. The false lumen of the abdominal aorta was completely thrombosed; all the visceral vessels originated from the true lumen of the dissection with the exception of the left renal artery; large intimal tears were identified at the origin of the innominate artery and at the level of distal descending thoracic aorta. The native aortic root measured 33 mm (Figure 2). A trans-thoracic echocardiogram showed a competent tricuspid aortic valve and a normal left ventricular ejection fraction (62%). The preoperative coronary angiogram revealed severe 3-vessel coronary artery disease with critical stenoses of the left anterior descending, obtuse marginal and right coronary arteries.

The patient was scheduled for a 3-staged hybrid treatment involving complete arch replacement with the FET and myocardial revascularization (stage 1), replacement of the abdominal aorta with visceral vessel de-branching (stage 2), and endovascular stenting of the remaining aortic segments from the FET to the abdominal aortic graft (stage 3). This video focuses on the stage-one procedure.
Surgical techniques
Re-sternotomy was performed using an oscillating saw. The left pleural space was opened and extensive isolation of the innominate vein (ligated and divided), the aortic arch, arch vessels and the heart was carried out. The left internal thoracic artery (LITA) and the saphenous vein grafts (SVG) were harvested for coronary artery bypass grafting (CABG). A guidewire was introduced from the right femoral artery into the true lumen of the dissection under transesophageal echocardiographic control.
A right sub-clavicular incision was performed and the axillary artery was cannulated with a direct technique (Axillary Perfusion Cannula, 24F, Edwards Lifesciences, Irvine, USA). After right atrial cannulation with a single two-stage cannula, cardiopulmonary bypass (CPB) was established, and cooling initiated with a target nasopharyngeal temperature of 26 °C. The right superior pulmonary vein was cannulated for left ventricle venting. The ascending aorta was clamped and cardioplegic arrest was achieved by means of antegrade infusion of crystalloid cardioplegia (Custodiol, Koehler Chemie, Alsbach-Haenlein, Germany). Myocardial revascularization was carried out by means of 3 single distal anastomoses (LITA to LAD, SVG to the marginal branch and the right coronary artery).
Our protocol for brain perfusion has already been described (2,3). At the nasopharyngeal temperature of 26 °C, the pump flow was reduced to 0.8-1.0 liter while the left subclavian and the left common carotid arteries were occluded with a tourniquet. Finally, the innominate artery was gently clamped, the aortic clamp was removed and, under unilateral right brain perfusion, the aortic arch was opened. The guide wire, previously introduced through the femoral artery, identified the small true lumen. An additional cardiotomy sucker was introduced into the descending thoracic aorta, and the left common carotid and left subclavian arteries were cannulated (RDB Cannula True Flow, MED-EUROPE, Bologna, Italy). Total antegrade selective cerebral perfusion was started at a flow rate of 10 mL/kg/min, equally distributed to the right and the left hemispheres, and adjusted to maintain a right radial arterial pressure of between 40 and 80 mmHg.
The aortic arch was completely resected. A robust distal aortic stump was created by obliterating the false lumen with 4 pledgeted 3-0 polypropylene U-stiches with a Teflon felt on the outside of the aorta. The Thoraflex system was gently bent and then advanced over the guidewire into the descending thoracic aorta.
The sheath was pulled back and removed while the delivery system was anchored at the handle. The splitter was removed from the device, and the release clip and wire were pulled to fully release the device from the delivery system. Once the stent-graft was deployed, the distal anastomosis was performed with a 3-0 polypropylene running suture using the incorporated sewing collar. The fourth branch of the graft was cannulated and lower body reperfusion and rewarming were initiated. The third branch of the graft was anastomosed to the left subclavian artery using a 5-0 polypropylene running suture. A proximal prosthesis-to prosthesis anastomosis was performed. The two vein grafts were anastomosed to the aortic graft using a 6-0 polypropylene running suture. After careful deairing using a 20G needle, the aortic clamp was removed and the myocardium was reperfused. The arch reconstruction was carried out by means of left common carotid and innominate artery reconstructions using the 2nd and 1st branches of the graft respectively. Subsequently, CPB was easily weaned off with no need for inotropic support. Operative times were as follows: CPB time: 223 minutes; myocardial ischemic time: 179 minutes; lower body ischemia time: 53 minutes and ASCP time: 129 minutes.
Outcome
At the writing of this manuscript, the patient is still being treated at our department (post-operative day 14). The post-operative course has been uneventful and the post-operative CT scan has shown complete thrombosis of the persistent false lumen in the descending thoracic aorta. In the absence of unforeseen complications, the stage-2 intervention will be performed within the next 4 weeks.
Comments
The Vascutek Thoraflex hybrid prosthesis represents a valuable graft for the treatment of patients with extensive diseases of the thoracic aorta. In particular, the proximal 4-branched graft can be appreciated for its sewing collar, which facilitates and reinforces the distal anastomosis, and allows for a separate reconstruction of the arch vessels. This may be relevant when their origins are distant from one another, and in patients with connective diseases or severe calcifications and/or clots at the proximal portions of the arch vessels for whom a radical aortic resection may be needed.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Shrestha M, Pichlmaier M, Martens A, et al. Total aortic arch replacement with a novel four-branched frozen elephant trunk graft: first-in-man results. Eur J Cardiothorac Surg 2013;43:406-10. [PubMed]
- Di Eusanio M, Schepens MA, Morshuis WJ, et al. Antegrade selective cerebral perfusion during operations on the thoracic aorta: factors influencing survival and neurologic outcome in 413 patients. J Thorac Cardiovasc Surg 2002;124:1080-6. [PubMed]
- Di Bartolomeo R, Pellicciari G, Cefarelli M, et al. Frozen elephant trunk surgery using the E-vita open plus prosthesis. Ann Cardiothorac Surg 2013;2:656-9.