Aortic root and total arch replacement with frozen elephant trunk procedure, using a Thoraflex Hybrid Graft
Clinical vignette
We present a case of a 78-year-old retired physician who was under cardiology investigation for exertional dyspnea and was subsequently found to have severe aortic regurgitation and aortic root dilation on transthoracic echocardiography (Video 1). She had a background history of non-obstructive coronary artery disease, systemic hypertension, mild mitral regurgitation, mild ventricular dilatation with a preserved ventricular function and impaired respiratory function. Her contrast computed tomography (CT) scans confirmed a 5 cm aortic root, an 8 cm ascending aorta and a 6 cm aortic arch and proximal descending thoracic aorta. Informed consent was obtained for an aortic root, ascending and total arch replacement procedure with an antegrade deployment of a stented graft in the descending aorta using the Thoraflex Hybrid Graft.
Surgical techniques
Cardiopulmonary bypass was employed. Aortic root replacement was performed while cooling down towards 20 °C, using a 21-mm Perimount Magna valve fitted inside a 24-mm Vascutek® Gelweave Valsalva™ Graft. This was followed by re-implantation of the coronary buttons. Under a brief period of deep hypothermic circulatory arrest, the arch was opened longitudinally. Distal organ protection was achieved with deep hypothermic circulatory arrest. Cerebral protection was provided with additional bilateral antegrade cerebral perfusion through separate perfusion catheters.
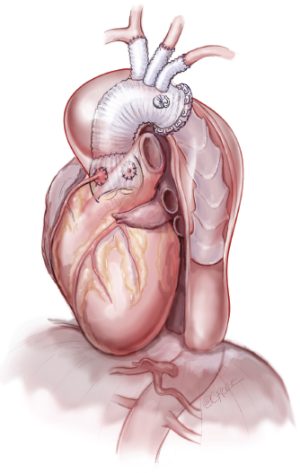
A 15 cm long, 32 mm-skirted Thoraflex hybrid™ graft from Vascutek Terumo was selected for antegrade deployment into the proximal descending thoracic aorta (Figure 1). The stented portion of the Thoraflex hybrid graft was bent slightly to conform to the curvature of the descending thoracic aorta and was guided down over a stiff Linderquist wire. The handle was used to stabilize the graft in position. The sheath was retracted back through the splitter to deploy the self-expandable stent. The splitter was then removed and the sewing collar was freed. Finally, the delivery system was released from the hybrid graft. The distal aortic reconstruction was performed with the sewing collar of the Thoraflex graft, using a 3-0 running prolene suture and was re-enforced with a second layer pledgeted 3-0 prolene sutures. Subsequently, a perfusion cannula was inserted to the side-branch of the Thoraflex graft for antegrade distal organ perfusion; the graft was then deaired and the distal aortic reconstruction was inspected for hemostasis.
The left subclavian artery, the left common carotid artery and finally the innominate artery were anastomosed to the epi-aortic branches of Thoraflex graft sequentially. Each anastomosis was performed, end-to-end, using a single layer 5-0 running prolene suture. The graft was deaired and antegrade perfusion to each supra-aortic vessel was re-established. The operation was completed with an end-to-end anastomosis between the Thoraflex graft and the Valsalva graft. The heart was deaired, and the patient was weaned from cardiopulmonary bypass. The patient was extubated uneventfully and was neurologically intact. At 3 months, the patient was doing well and follow-up CT imaging showed satisfactory repair.
Comments
Development of hybrid stent-graft has facilitated the complex management of aortic pathologies involving the arch and proximal descending aorta. By providing expansive radial force to the distal portion of the prosthesis in the descending aorta, these modern variants of the traditional elephant trunk are able to prevent anastomotic leakages prevent anastomotic leakages more effectively, reduce the risk of prosthesis twisting, and exclude proximal descending thoracic aneurysm as demonstrated in this scenario. In aortic dissection, FET provides better seal of descending aortic tears, increase graft patency in collapsed lumina, and limit subsequent dilation of the aortic diameter. These prostheses enable the completion of surgical repair in a single stage, thus obviating the cumulative mortality and interval mortality associated with two-stage approaches.
Recent findings demonstrate that the FET can be performed with acceptable mortality and morbidity risks. A systematic review of 17 studies identified a pooled mortality of 8.3%, and stroke rate of 4.9% (1). Cardiopulmonary bypass time, myocardial ischemia time, and circulatory arrest time were strongly correlated with mortality. Despite using hypothermic circulatory arrest for organ protection, spinal cord injury remains a noteworthy concern, with a pooled rate of 5.1% identified in the review. Variations existed between institutions regarding the length of the stented portion of the prostheses as part of attempts to minimize occlusion of intercostal arteries. Care must be taken when utilizing the FET approach to ensure appropriate selection of the distal landing zone in order to reduce the risk of spinal cord complications. Additionally, drainage of cerebral spinal fluid as a means of maintaining stable intrathecal pressure must be considered as an option for cord protection.
The tetrafurcate Thoraflex stent-graft offers several new technical innovations over other designs. Firstly, the four branches of the graft allow separate reimplantation of supra-aortic vessels, in lieu of en-bloc (island) reimplantation, therefore providing better individual hemostatic control of vessel anastomosis. Secondly, the collared skirt between the Dacron graft and the stent portion ensures easier anastomosis of the prosthesis to the distal aortic arch. Finally, radio-opaque markers in the stented portion simplifies future endovascular interventions (2).
The Thoraflex hybrid graft represents a suitable alternative for management of complex arch pathologies involving the arch and proximal descending aorta. Further applications with longer follow-up results will provide better understanding of the role of this graft in aortic arch surgery.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Tian DH, Wan B, Di Eusanio M, et al. A systematic review and meta-analysis on the safety and efficacy of the frozen elephant trunk technique in aortic arch surgery. Ann Cardiothorac Surg 2013;2:581-91.
- Ius F, Fleissner F, Pichlmaier M, et al. Total aortic arch replacement with the frozen elephant trunk technique: 10-year follow-up single-centre experience. Eur J Cardiothorac Surg 2013. [Epub ahead of print]. [PubMed]