Custodiol for myocardial protection and preservation: a systematic review
Introduction
Custodiol is an intracellular crystalloid cardioplegic solution used by some centres for myocardial protection in complex cardiac surgery and for organ preservation in transplant surgery. Histidine-tryptophan-ketoglutarate (HTK), Bretschneider’s, or Custodiol is attractive for cardiac surgeons because it is administered as a single dose and is claimed to offer myocardial protection for a period of up to three hours (1,2), allowing performance of complex procedures without interruption.
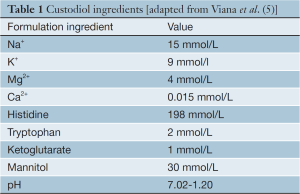
HTK was described by Bretschneider in the 1970s (3). It is classified as an intracellular, crystalloid cardioplegia due to its low sodium and calcium content. Sodium depletion of the extracellular space causes a hyperpolarization of the myocyte plasma membrane, inducing cardiac arrest in diastole. This is a different mechanism of action from conventional ‘extracellular’ cardioplegic solutions, which are high in potassium content and cause arrest by membrane depolarisation (4). The components of Custodiol are listed in Table 1. A high histidine content buffers the acidosis caused by the accumulation of anaerobic metabolites during the long ischaemic period; ketoglutarate improves ATP production during reperfusion; tryptophan stabilises the cell membrane and mannitol decreases cellular oedema and acts as a free-radical scavenger (2).
Despite its widespread use in Europe, there is very little data comparing the efficacy of Custodiol with conventional blood or crystalloid cardioplegia. There is also a paucity of data comparing Custodiol with other solutions for preservation of the heart in transplantation. There is concern about the adequacy of myocardial protection offered by only a single dose of cardioplegia. Similarly, concerns have been raised about hyponatraemia that follows the rapid administration of the requisite high volume of this low sodium cardioplegic solution (6,7).
Whilst initially introduced for myocardial protection in routine cardiac surgery, Custodiol has expanded into the field of transplantation. It has been used not only in cardiac transplantation, and adopted widely in Europe (8), but also in the preservation of multiple organs (9). Despite widespread use, its role in cardiac transplantation is as yet unclear. This is at least partially the result of the wide and expanding range of cardioplegia solutions that are used globally. A single review identified 167 different solutions in clinical use in the USA (10). There is a lack of high-quality randomised trials examining the influence of the cardioplegia solution on graft injury and early graft performance.
In this systematic review we performed a meta-analysis of outcomes related to myocardial protection reported by all studies comparing Custodiol with conventional cardioplegia (either blood or extracellular crystalloid). We reviewed results of large case series using Custodiol cardioplegia. Finally, we reviewed studies comparing Custodiol with other solutions used for organ preservation in heart transplantation.
Methods
Search methods for identification of studies
Electronic searches were performed of Ovid MEDLINE, Pubmed, EMBASE, Cochrane Central Register of Controlled Trials (CCTR), Cochrane Database of Systematic Reviews (CDSR), ACP Journal Club and Database of Abstracts of Review of Effectiveness (DARE) from inception to October 2013. The search strategy used a combination of ‘histidine-tryptophan-ketoglutarate’ or ‘Bretschneider’, or ‘Custodiol’ or ‘cardioplegic solutions’ or ‘cardiac arrest (induced)’ as keywords, MeSH and Emtree headings. Manual searches of reference lists were used to identify any studies not found in the initial search.
An extensive literature search was also performed to identify any additional large case series that used Custodial in their methods section, but was not listed in their title/abstract or MeSH/Emtree headings during the systematic search.
Selection criteria
Studies of both cardioplegia and cardiac transplantation in humans were identified. Those studies that reported the primary or secondary endpoints described in the research protocol, including mortality, myocardial protection and peri-operative morbidity, were included (11). Only studies in English language were considered for inclusion. The article types of abstract and letter were excluded. Inclusion was assessed by three independent reviewers (J.E., M.S. and B.D.), and differences of opinion were resolved by discussion with a senior investigator (J.P., M.P.V. and T.D.Y.).
Study end-points
The primary end-point for this study was mortality at 30 days. Secondary endpoints included surrogates for myocardial protection [myocardial infarction, cardiac enzyme release, low cardiac output syndrome (LCOS)/use of inotropes] and rhythm disturbances [ventricular fibrillation (VF) as the first rhythm after cross clamp release, and new post-operative atrial fibrillation (AF)].
Definitions
Myocardial infarction (MI) was defined as any two of the following: cardiac enzyme increase, new regional wall motion abnormality on echocardiogram or new Q-waves on electrocardiogram. We combined use of inotropes and LCOS as a single end-point. Criteria for inotrope use and a definition of LCOS were given by only two studies that reported these as end-points (12,13). Use of inotropes was in most studies at the treating clinician’s discretion.
Statistical analysis
For the meta-analysis, the relative risk/risk ratio (RR) was used as a summary statistic. Both fixed and random effect models were tested: when there were variations between studies, a random effect model was used as the calculated ratios have a more conservative value. Heterogeneity was tested using χ2 tests. If there was a substantial heterogeneity, the possible clinical and methodological reasons for this were explored qualitatively. Continuous variables were analyzed using inverse variance with the calculation of mean difference as the summary statistic in both fixed and random effects models, as above.
Results
Search results
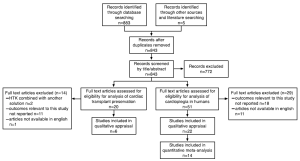
The systematic search identified 51 potentially relevant cardioplegia studies and 20 potentially relevant cardiac transplantation studies. Reasons for exclusion are detailed in the flow-diagram in Figure 1, according to the PRISMA statement (14).
Twenty-two cardioplegia studies satisfied the inclusion criteria for qualitative appraisal. Fourteen comparative studies were further selected for quantitative meta-analysis and eight large case-series were examined for qualitative appraisal. Two studies, comparing Custodiol to intermittent aortic clamping and perfused VF were not included in meta-analysis because they were not comparable to other studies using conventional cardioplegia (15,16).
Six cardiac transplantation studies satisfied inclusion criteria and were included in a qualitative review.
Meta-analysis of studies comparing Custodiol to conventional cardioplegia
Patients and demographics
Table 2 shows details of 14 comparative studies included in the meta-analysis. Twelve of the 14 studies sought primarily to determine the outcomes related to Custodiol cardioplegia and compared similar surgical procedures. The primary aim of two studies was to determine efficacy of a particular surgical technique that happened to use Custodiol as cardioplegia (19,23).
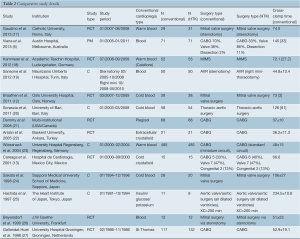
Full table
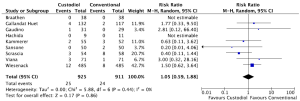
Primary endpoint—mortality
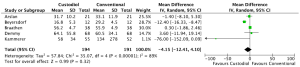
Nine studies reported mortality (5,11,18-20,23,25-27). Overall, the 925 patients receiving Custodiol had a similar risk of mortality as the 911 patients receiving conventional cardioplegia for myocardial protection. The rate of mortality was 2.70% in the Custodiol group, compared with 2.63% in the conventional group (RR 1.05, 95% CI, 0.59-1.88, P=0.86; Figure 2). There was no significant heterogeneity between the studies (I2=0%; heterogeneity P=0.55). Including studies where only similar surgical procedures were compared, there remained no difference in the rate of mortality (RR 0.89, 95% CI, 0.40-1.96, P=0.77, n=766).
Secondary endpoints
Myocardial protection
Five studies reported the rate of peri-procedural MI as per the definition listed in the methods (5,12,13,21,23). The rate of MI reported in the 677 patients given Custodiol did not differ from 677 patients receiving conventional cardioplegia (Custodiol 2.81% vs. 1.62%, RR 1.72, 95% CI, 0.82-3.60, P=0.15). There was no heterogeneity between studies (I2=0%, heterogeneity P=0.53).
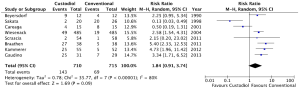
Five studies reported mean creatine kinase (CK-MB) or troponin-I (Tn-I) (12,18,21,22,26). In these studies, there was a trend towards shorter cross-clamp time in the conventional cardioplegia groups (weighted mean: Custodiol 62.9 min vs. conventional 54.8 min, P=0.11). Mean differences for both CK-MB and TnI did not differ between groups (CK-MB: mean difference –4.15 (–12.41-4.10), P=0.32, Figure 3; Tn-I: mean difference 0.90, 95% CI, –4.68-6.48, P=0.75).
Seven studies reported the need for inotropes or a low cardiac output syndrome in the immediate post-operative period, and included a total of 1,408 patients (12,13,17,20,21,23,26). The rate of inotropes/Low cardiac output syndrome (LCOS) did not differ between groups (Custodiol 15.0% vs. conventional 12.7%, RR 1.33, 95% CI, 0.86-2.05, P=0.20). Heterogeneity of the results between studies limits interpretation of the result (I2=64%, heterogeneity P=0.01). Only one study (13) reported significantly lower incidence of inotropic support in the Custodiol group. The reason for this heterogeneity in results was not immediately clear on review of the methodology. Three studies reported the use of mechanical support, with no significant difference between groups (5,21,27).
Arrhythmia
Eight studies reported the incidence of ventricular arrhythmias during reperfusion (Custodiol n=710, conventional n=715) (12,13,17,18,20,23,24,26). Six of the eight studies that reported a higher incidence of VF after removal of the cross clamp in the Custodiol group. Overall, there was a trend for increased incidence that reached statistical significance in the fixed but not the random effects model (Custodiol 20.1% vs. 9.7%, random effects RR 1.84, 95% CI, 0.91-3.74, P=0.09, Figure 4; fixed effects: RR 2.12, 95% CI, 1.63-2.76, P<0.001). Only two studies reported a lower rate of VF after Custodiol (13,24) and this resulted in significant heterogeneity between studies (I2=80%, heterogeneity P<0.001). The reason for the difference in results reported by these studies was not immediately clear on qualitative review.
Four studies (336 patients) reported the incidence of AF in the post-operative period (12,20,21,23). There was no significant difference in the rate of AF between groups (Custodiol 34.3% vs. conventional 17.7%, RR 1.36, 95% CI, 0.74-2.50, P=0.32). Only one study reported a significantly greater incidence of AF in patients given Custodiol, which contributed to the significant heterogeneity in the analysis (I2=87%, heterogeneity P<0.001).
Qualitative appraisal of large case-series of Custodiol cardioplegia
Case series of any adult cardiac surgery were included if they reported results of >100 patients and exclusively used Custodiol cardioplegia. Eight series satisfied these criteria, reporting the results from a total of 6,840 patients (28-35). The details of these studies are in Table 3. Mortality was the only outcome universally reported. The rates of mortality reported in these studies are similar to other series reporting similar surgical procedures using conventional cardioplegia.
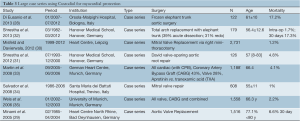
Full table
Custodiol for cardiac transplantation
Three studies were identified comparing Custodiol with other solutions for heart preservation in transplant (36-38). There were three case series, one of which duplicated results reported from one of the comparative studies (8,39,40). Mortality was reported by five studies, acute graft failure or rejection by three (Table 4).
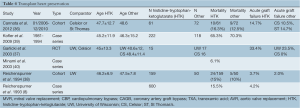
Full table
There is only one randomised study comparing Custodiol with other solutions for preservation in heart transplant (37). Forty-eight cardiac transplants were randomised to Custodiol, UW or Celsior. Cardiac index was equivalent across all three groups. The Celsior group achieved spontaneous recovery of sinus rhythm more often that the Custodiol or UW groups. Unfortunately, no data on rates of acute graft dysfunction was provided as those with acute graft dysfunction were excluded. The group reported acute rejection (67% Custodiol, 47% UW, 19% Celsior) and rates of allograft vasculopathy as assessed by IVUS at one year (100% Custodiol, 88% UW, 69% Celsior). There was no difference in ischaemic time between groups but the authors argue that inferior myocardial protection and subsequent increase in inflammatory response may have been the mechanism causing the increased rate of acute rejection and later development of allograft vasculopathy.
Discussion
Debate continues as to the ideal cardioplegic solution for myocardial protection in cardiac surgery. A meta-analysis of randomised trials comparing intermittent blood and crystalloid cardioplegia concluded that blood offers superior myocardial protection, but none of the included studies used Custodiol in the crystalloid group (41). Similar debate continues as to the ideal solution for organ preservation in heart (and indeed other solid organ) transplantation.
Custodiol for myocardial protection
This systematic review included both randomised and non-randomised studies, comparing a total of 2,114 patients in meta-analysis and 6,840 patients in case series. The meta-analysis suggests no significant difference between Custodiol and conventional cardioplegia for the primary endpoint mortality, or the secondary endpoints used as surrogate markers of myocardial protection during cardiac surgery. The similar rate of mortality (in a comparison of 1,836 patients) and CK-MB, MI and LCOS/inotrope confirms the safety of the Custodiol in comparison to conventional cardioplegia.
Experimental animal models of cardioplegic arrest using Custodiol versus conventional cardioplegia have been critical of the myocardial protection offered by Custodiol. Fannelop and colleagues randomised 16 pigs placed on cardiopulmonary bypass (CPB) to cardioplegic arrest with a single dose of Custodiol or intermittent cold-blood cardioplegia (42). Pigs receiving Custodiol had lower cardiac indices, ventricular function and higher troponin-T release in the first four post-operative hours compared with pigs receiving cold-blood cardioplegia. A similar advantage for pigs randomised to intermittent St Thomas’ Hospital Solution compared to single dose Custodiol was reported by Aarsaether and colleagues (43). These studies contrast with that of Chen and colleagues, who in neonatal piglets randomised to Custodiol or multi-dose blood cardioplegia for protection during a 2-hour cross-clamp time show equivalent myocardial protection by biochemical and histopathological assessment (44).
Studies comparing Custodiol with conventional intermittent cardioplegia in paediatric patients have reported conflicting results. In a retrospective study of neonates undergoing arterial switch operation, Bojan and colleagues reported a higher troponin release in those who received Custodiol compared with warm blood cardioplegia (45). In contrast, Korun and colleagues reported no significant difference in clinical outcomes of paediatric patients undergoing surgery for congenital heart disease (46). However, liver enzymes and an apoptosis index (measured from biopsies taken of the right ventricle) correlated with cross clamp time in the conventional cardioplegia group, but not the Custodiol group. A similar finding was made by Liu et al., who reported lower mortality with use of Custodiol for cross clamp times >90 min when compared with conventional cardioplegia (47).
Right ventricular (RV) function after mitral valve surgery is an independent predictor of survival (48), thus its protection is of paramount importance. One small randomised study has questioned the adequacy of right ventricular myocardial protection offered by Custodiol compared with conventional cardioplegia (intermittent warm blood) (17). Patients with poor pre-operative RV function (as measured by tricuspid annular plane systolic excursion—TAPSE) randomised to myocardial protection with Custodiol had a lower RV ejection fraction and volumes, and worse clinical outcome (lower cardiac indices, higher pulmonary pressures, longer period of time on inotropes) in the post-operative period than those protected with whole blood cardioplegia. There was no difference in the outcome of those with normal pre-operative RV function protected with Custodiol versus intermittent blood (17).
The majority of comparative studies have reported an increased rate of VF as the first rhythm after reperfusion with Custodiol cardioplegia. The increased rate of ventricular arrhythmias after removal of cross-clamp in the Custodiol group did not reach statistical significance, with evidence of heterogeneity in the included studies. The reason for this is not clear. Some authors have suggested that VF after reperfusion may be an indication of inadequate myocardial protection (47), but no studies have related an initial VF rhythm to adverse outcomes.
There is concern about the significant hyponatraemia and acidosis that results from rapid infusion of a large volume of Custodiol (Na+ 15 mmol/L) (6,7). None of the comparative studies included in the meta-analysis reported serum sodium levels, nor any outcomes that might be considered surrogates of clinical hyponatraemia. Similarly, none of the series that report (or indeed investigate) hyponatraemia were large enough to satisfy inclusion criteria for this study. In a series of 25 patients, Lindner et al. measured serum sodium and osmolality at 11 intra- and post-operative time-points (49). Whilst patients had a significant (and rapid) decrease in serum sodium (15 mmol/L), there was no significant change in osmolality, suggesting an isotonic hyponatremia. Others have observed hyponatraemia without clinical consequence (5,50). Many groups treat hyponatremia after Custodiol administration with a haemofilter on the cardiopulmonary bypass circuit, or prevent it altogether by aspirating the antegrade-directed cardioplegia from a retrograde cannula (13).
Custodiol for cardiac transplantation
The human studies on Custodiol as a preservation solution for cardiac transplantation are few in number and are (except for one) non-randomised. A number of small animal studies suggest superiority of Custodiol over UW (51), Celsior (52,53) St. Thomas’ solution and Krebs-Heinseleit Buffer (KHB) (54) with Custodiol-preserved hearts having better indices of left-ventricular function (51) and also demonstrating lower circulating levels of both TnI and CK, indicating less graft injury (52,53). There also appears to be better preservation of myocardial ATP stores (51-53) reduced markers of ischaemia-reperfusion injury as well as reduced apoptosis of myocardial cells (52,53). The mechanism by which Custodiol limits ischaemia/reperfusion injury in transplant is unclear, but may be due to the higher level of ATP-producing anaerobic glycolysis (53). One study has suggested that left ventricular function may be better preserved with Celsior cardioplegia (54), although the same paper demonstrated less myocardial oedema in Custodiol-preserved hearts.
There is, to date, only one large animal study comparing Custodiol to Celsior. This work was done with canine hearts and demonstrated that after 12 hours of ischaemia Custodiol-preserved hearts had significantly better left ventricular function, required less defibrillation in the reperfusion period to achieve sinus rhythm, were less prone to arrhythmic events once sinus rhythm was achieved and had a better myocardial ATP:ADP ratio (55).
Despite compelling evidence from small and large animal studies, solid data from human clinical trials supporting the use of Custodiol over other preservation solutions is lacking. The pre-clinical data is sufficient to encourage large-scale, quality randomised trials to answer the compelling question of which preservation solution provides optimal protection for the cardiac allograft.
Limitations
The limitations in this study reflect the relative paucity of data comparing Custodiol with conventional cardioplegia in adult cardiac surgery, and the need for a large randomised trial. The objective of two of the studies included in the meta-analysis was to compare different surgical techniques rather than the mode of cardioplegia. We were cognisant of the potential to introduce bias by including such studies but nevertheless did so due to the few studies specifically designed to investigate the efficacy of Custodiol. In these studies it is likely that surgical procedure significantly influenced the results. The majority of patients contributing to the MI and LCOS/inotrope analysis came from the study by Wiesenack et al. (23) This study concluded that the rate of MI and low cardiac output is lower by using a miniature cardiopulmonary bypass (CPB) circuit (with conventional cardioplegia) compared with a standard length CPB circuit (with Custodiol). Sansone et al. reported a trend towards lower mortality in patients undergoing minimally invasive aortic valve surgery (using Custodiol) compared with AVR via sternotomy (with blood cardioplegia) (19). This limits the conclusions that can be made by this review. A clinical trial comparing Custodiol with cold blood cardioplegia (NCT01681095) is currently recruiting patients (target 110 patients) undergoing cardiovascular surgery.
Conclusions
The results of the available evidence suggest that Custodiol offers myocardial protection that is equivalent to that of conventional cardioplegia. However, the body of evidence available from which to draw conclusions is limited by the small number of randomised patients. A single dose cardioplegia strategy for myocardial protection has significant benefits for the performance of minimally invasive or complex cardiac surgery and the results of this review support its ongoing use. However, there is not enough evidence to recommend the routine use of Custodiol for the performance of coronary artery bypass grafting (CABG) or other simple open cardiac surgical procedures. There is not enough evidence from human studies to assess the efficacy of Custodiol for organ preservation. Large, randomised trials are required to determine the efficacy of Custodiol for both myocardial protection in cardiac surgery and myocardial preservation in cardiac transplant.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Gebhard MM, Preusse CJ, Schnabel PA, et al. Different effects of cardioplegic solution HTK during single or intermittent administration. Thorac Cardiovasc Surg 1984;32:271-6. [PubMed]
- Bretschneider HJ. Myocardial protection. Thorac Cardiovasc Surg 1980;28:295-302. [PubMed]
- Bretschneider HJ, Hübner G, Knoll D, et al. Myocardial resistance and tolerance to ischemia: physiological and biochemical basis. J Cardiovasc Surg (Torino) 1975;16:241-60. [PubMed]
- Chambers DJ. Mechanisms and alternative methods of achieving cardiac arrest. Ann Thorac Surg 2003;75:S661-6. [PubMed]
- Viana FF, Shi WY, Hayward PA, et al. Custodiol versus blood cardioplegia in complex cardiac operations: an Australian experience. Eur J Cardiothorac Surg 2013;43:526-31. [PubMed]
- Ji B, Liu J, Long C, et al. Potential risk of hyponatremia using histidine-tryptophan-ketoglutarate solution during pediatric cardiopulmonary bypass. Ann Thorac Surg 2012;93:2120-1; author reply 2121. [PubMed]
- Kim JT, Park YH, Chang YE, et al. The effect of cardioplegic solution-induced sodium concentration fluctuation on postoperative seizure in pediatric cardiac patients. Ann Thorac Surg 2011;91:1943-8. [PubMed]
- Reichenspurner H, Russ C, Uberfuhr P, et al. Myocardial preservation using HTK solution for heart transplantation. A multicenter study. Eur J Cardiothorac Surg 1993;7:414-9. [PubMed]
- Hölscher M, Groenewoud AF. Current status of the HTK solution of Bretschneider in organ preservation. Transplant Proc 1991;23:2334-7. [PubMed]
- Demmy TL, Biddle JS, Bennett LE, et al. Organ preservation solutions in heart transplantation--patterns of usage and related survival. Transplantation 1997;63:262-9. [PubMed]
- Edelman JJ, Seco M, Dunne B, et al. Systematic review protocol: single-dose histidine-tryptophan-ketoglutarate vs. intermittent crystalloid or blood cardioplegia. Ann Cardiothorac Surg 2013;2:677. [PubMed]
- Braathen B, Jeppsson A, Scherstén H, et al. One single dose of histidine-tryptophan-ketoglutarate solution gives equally good myocardial protection in elective mitral valve surgery as repetitive cold blood cardioplegia: a prospective randomized study. J Thorac Cardiovasc Surg 2011;141:995-1001. [PubMed]
- Careaga G, Salazar D, Téllez S, et al. Clinical impact of histidine-ketoglutarate-tryptophan (HTK) cardioplegic solution on the perioperative period in open heart surgery patients. Arch Med Res 2001;32:296-9. [PubMed]
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009;6:e1000100. [PubMed]
- Sunderdiek U, Feindt P, Gams E. Aortocoronary bypass grafting: a comparison of HTK cardioplegia vs. intermittent aortic cross-clamping. Eur J Cardiothorac Surg 2000;18:393-9. [PubMed]
- Imanaka K, Kyo S, Ogiwara M, et al. Mitral valve surgery under perfused ventricular fibrillation with moderate hypothermia. Circ J 2002;66:450-2. [PubMed]
- Gaudino M, Pragliola C, Anselmi A, et al. Randomized trial of HTK versus warm blood cardioplegia for right ventricular protection in mitral surgery. Scand Cardiovasc J 2013. [Epub ahead of print]. [PubMed]
- Kammerer I, Nagib R, Hipp G, et al. Myocardial Protection in Minimally Invasive Mitral Valve Surgery: Comparison of the Cold-Blood Cardioplegia of the Bretschneider Solution and the Warm-Blood Cardioplegia of the Calafiore Protocol. Arch Clin Exp Surg 2012;1:14-21.
- Sansone F, Punta G, Parisi F, et al. Right minithoracotomy versus full sternotomy for the aortic valve replacement: preliminary results. Heart Lung Circ 2012;21:169-73. [PubMed]
- Scrascia G, Guida P, Rotunno C, et al. Myocardial protection during aortic surgery: comparison between Bretschneider-HTK and cold blood cardioplegia. Perfusion 2011;26:427-33. [PubMed]
- Demmy TL, Molina JE, Ward HB, et al. Custodiol versus Plegisol: A phase 3 multicentre myocardial protection study. Int J Angiol 2008;17:149-53. [PubMed]
- Arslan A, Sezgin A, Gultekin B, et al. Low-dose histidine-tryptophan-ketoglutarate solution for myocardial protection. Transplant Proc 2005;37:3219-22. [PubMed]
- Wiesenack C, Liebold A, Philipp A, et al. Four years' experience with a miniaturized extracorporeal circulation system and its influence on clinical outcome. Artif Organs 2004;28:1082-8. [PubMed]
- Sakata J, Morishita K, Ito T, et al. Comparison of clinical outcome between histidine-triptophan-ketoglutalate solution and cold blood cardioplegic solution in mitral valve replacement. J Card Surg 1998;13:43-7. [PubMed]
- Hachida M, Nonoyama M, Bonkohara Y, et al. Clinical assessment of prolonged myocardial preservation for patients with a severely dilated heart. Ann Thorac Surg 1997;64:59-63. [PubMed]
- Beyersdorf F, Krause E, Sarai K, et al. Clinical evaluation of hypothermic ventricular fibrillation, multi-dose blood cardioplegia, and single-dose Bretschneider cardioplegia in coronary surgery. Thorac Cardiovasc Surg 1990;38:20-9. [PubMed]
- Gallandat Huet RC, Karliczek GF, van der Heide JN, et al. Clinical effect of Bretschneider-HTK and St. Thomas cardioplegia on hemodynamic performance after bypass measured using an automatic datalogging database system. Thorac Cardiovasc Surg 1988;36:151-6. [PubMed]
- Di Eusanio M, Pantaleo A, Murana G, et al. Frozen elephant trunk surgery-the Bologna’s experience. Ann Cardiothorac Surg 2013;2:597-605. [PubMed]
- Minami K, Zittermann A, Schulte-Eistrup S, et al. Mitroflow synergy prostheses for aortic valve replacement: 19 years experience with 1,516 patients. Ann Thorac Surg 2005;80:1699-705. [PubMed]
- Misfeld M, Davierwala P. Crystalloid-based cardioplegia for minimally invasive cardiac surgery. Semin Thorac Cardiovasc Surg 2012;24:305-7. [PubMed]
- Shrestha M, Baraki H, Maeding I, et al. Long-term results after aortic valve-sparing operation (David I). Eur J Cardiothorac Surg 2012;41:56-61; discussion 61-2. [PubMed]
- Shrestha M, Martens A, Krüger H, et al. Total aortic arch replacement with the elephant trunk technique: single-centre 30-year results. Eur J Cardiothorac Surg 2013. [Epub ahead of print]. [PubMed]
- Martin K, Wiesner G, Breuer T, et al. The risks of aprotinin and tranexamic acid in cardiac surgery: a one-year follow-up of 1188 consecutive patients. Anesth Analg 2008;107:1783-90. [PubMed]
- Salvador L, Mirone S, Bianchini R, et al. A 20-year experience with mitral valve repair with artificial chordae in 608 patients. J Thorac Cardiovasc Surg 2008;135:1280-7. [PubMed]
- Weis F, Kilger E, Beiras-Fernandez A, et al. Association between vasopressor dependence and early outcome in patients after cardiac surgery. Anaesthesia 2006;61:938-42. [PubMed]
- Cannata A, Botta L, Colombo T, et al. Does the cardioplegic solution have an effect on early outcomes following heart transplantation? Eur J Cardiothorac Surg 2012;41:e48-52; discussion e52-3.
- Garlicki M. May preservation solution affect the incidence of graft vasculopathy in transplanted heart? Ann Transplant 2003;8:19-24. [PubMed]
- Reichenspurner H, Russ C, Wagner F, et al. Comparison of UW versus HTK solution for myocardial protection in heart transplantation. Transpl Int 1994;7 Suppl 1:S481-4. [PubMed]
- Kofler S, Bigdeli AK, Kaczmarek I, et al. Long-term outcomes after 1000 heart transplantations in six different eras of innovation in a single center. Transpl Int 2009;22:1140-50. [PubMed]
- Minami K, Omoto T, Böthig D, et al. Creatine kinase and troponin after myocardial preservation using HTK solution (Custoidol) for clinical heart transplantation. J Heart Lung Transplant 2003;22:192-4. [PubMed]
- Guru V, Omura J, Alghamdi AA, et al. Is blood superior to crystalloid cardioplegia? A meta-analysis of randomized clinical trials. Circulation 2006;114:I331-8. [PubMed]
- Fannelop T, Dahle GO, Salminen PR, et al. Multidose cold oxygenated blood is superior to a single dose of Bretschneider HTK-cardioplegia in the pig. Ann Thorac Surg 2009;87:1205-13. [PubMed]
- Aarsaether E, Stenberg TA, Jakobsen Ø, et al. Mechanoenergetic function and troponin T release following cardioplegic arrest induced by St Thomas’ and histidine-tryptophan-ketoglutarate cardioplegia-- an experimental comparative study in pigs. Interact Cardiovasc Thorac Surg 2009;9:635-9. [PubMed]
- Chen Y, Liu J, Li S, et al. Which is the better option during neonatal cardiopulmonary bypass: HTK solution or cold blood cardioplegia? ASAIO J 2013;59:69-74. [PubMed]
- Bojan M, Peperstraete H, Lilot M, et al. Cold histidine-tryptophan-ketoglutarate solution and repeated oxygenated warm blood cardioplegia in neonates with arterial switch operation. Ann Thorac Surg 2013;95:1390-6. [PubMed]
- Korun O, Özkan M, Terzi A, et al. The comparison of the effects of Bretschneider's histidine-tryptophan-ketoglutarate and conventional crystalloid cardioplegia on pediatric myocardium at tissue level. Artif Organs 2013;37:76-81. [PubMed]
- Liu J, Feng Z, Zhao J, et al. The myocardial protection of HTK cardioplegic solution on the long-term ischemic period in pediatric heart surgery. ASAIO J 2008;54:470-3. [PubMed]
- Haddad F, Couture P, Tousignant C, et al. The right ventricle in cardiac surgery, a perioperative perspective: II. Pathophysiology, clinical importance, and management. Anesth Analg 2009;108:422-33. [PubMed]
- Lindner G, Zapletal B, Schwarz C, et al. Acute hyponatremia after cardioplegia by histidine-tryptophane-ketoglutarate--a retrospective study. J Cardiothorac Surg 2012;7:52. [PubMed]
- Lueck S, Preusse CJ, Welz A. Clinical relevance of HTK-induced hyponatremia. Ann Thorac Surg 2013;95:1844-5. [PubMed]
- Saitoh Y, Hashimoto M, Ku K, et al. Heart preservation in HTK solution: role of coronary vasculature in recovery of cardiac function. Ann Thorac Surg 2000;69:107-12. [PubMed]
- Lee S, Huang CS, Kawamura T, et al. Histidine-tryptophan-ketoglutarate or celsior: which is more suitable for cold preservation for cardiac grafts from older donors? Ann Thorac Surg 2011;91:755-63. [PubMed]
- Lee S, Huang CS, Kawamura T, et al. Superior myocardial preservation with HTK solution over Celsior in rat hearts with prolonged cold ischemia. Surgery 2010;148:463-73. [PubMed]
- Lima ML, Fiorelli AI, Vassallo DV, et al. Comparative experimental study of myocardial protection with crystalloid solutions for heart transplantation. Rev Bras Cir Cardiovasc 2012;27:110-6. [PubMed]
- Ackemann J, Gross W, Mory M, et al. Celsior versus custodiol: early postischemic recovery after cardioplegia and ischemia at 5 degrees C. Ann Thorac Surg 2002;74:522-9. [PubMed]