Cross-sectional survey on minimally invasive mitral valve surgery
Introduction
Minimally invasive mitral valve surgery (MIMVS) has proven to be a suitable alternative to conventional full sternotomy (1-4). The term ‘minimally invasive’ summarizes a variety of different approaches to the mitral valve, including mini-thoracotomy, partial sternotomy, robotic surgery and others. In the majority of cases, MIMVS is performed through a right antero-lateral mini-thoracotomy, either under direct vision or totally endoscopically. Following the first description of MIMVS by Carpentier et al. in 1996 (5), the number of cases performed through this method has increased remarkably. There are specific advantages of the minimally invasive approach, including less postoperative pain and decreased surgical trauma leading to improved postoperative recovery and cosmesis. In the majority of cases, surgeons who perform MIMVS have a special interest in mitral valve surgery and a higher expertise compared to surgeons who do not focus on this approach. However, owing to the lack of specific guidelines, differing opinions between surgeons regarding absolute and relative contraindications to performing MIMVS still remain. Additionally, there exists a need for an overall consensus on which basic skills, training and surgical performance is required to enable an adequate surgical expertise to perform MIMVS. This Consensus Survey of expert minimally invasive mitral valve surgeons provides a summary of recommendations regarding eligibility and surgical training and research.
Methods
A group of surgeons who have published on this topic with a minimum of 100 cases were identified through electronic search of the literature. Other surgeons who are known to be experienced in this field were also added. These individuals were contacted to answer a list of multiple choice questions, which had been created by a nucleus group of authors (MM, TDY, DHT). Three groups of questions were formulated, focusing on patient factors, mitral valve pathology, and surgical skills. Emails were sent with unique links to the online survey platform, with two follow-up reminders where appropriate. Twenty experienced mini-mitral surgeons participated in the survey.
Results
Patient-related factors
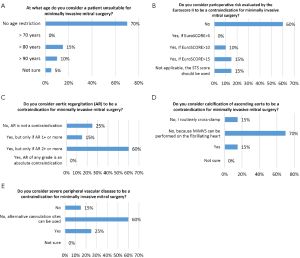
- The majority of surgeons did not consider age to be a contraindication for MIMVS at all (70%), while a minority (15%) would not perform MIMVS if the patient is older than 80 years and 10% would not if age exceeds 90 years (Figure 1A).
- Malformations of the chest (i.e., pectus excavatum) were not contraindications for MIMVS in 45% of the answers. Six colleagues (30%) considered malformations as a contraindication and four (20%) believed it to be contraindicated only if the heart is shifted to the left side.
- Preoperative risk evaluation by using EuroSCORE II prevented some surgeons from performing MIMVS, particularly if EuroSCORE II is >5 (10%) or >10 (15%), but the majority of surgeons (60%) did not consider the EuroSCORE II to influence their decision (Figure 1B).
- Obesity was not a contraindication to perform MIMVS for 50% of surgeons asked. Two surgeons would not perform MIMVS if the body mass index is ≥35 (World Health Organization criteria) and seven surgeons would not perform MIMVS in patients with a BMI ≥40.
- Aortic valve regurgitation (AR) was not a contraindication for MIMVS for five participants (25%). Three surgeons (15%) would not accept AR 1+ and the majority of surgeons (60%) would not accept patient with AR 2+ (Figure 1C).
- In cases of calcification of the ascending aorta, 70% of surgeons (n=14) stated that MIMVS can still be performed on the fibrillating heart without cross-clamping. Three surgeons (15%) cross-clamp routinely in calcified aortas and three others (15%) would not perform MIMVS if the aorta is calcified (Figure 1D).
- Severe peripheral vascular disease was considered a contraindication to MIMVS for 25% of surgeons. However, the majority (60%) do not consider it to be a contraindication as they believe alternative cannulation sites (i.e., axillary artery) can be used (Figure 1E).
- With regard to prior surgical interventions which contraindicate MIMVS, respondents were allowed to select multiple options. Respondents considered MIMVS as contraindicated in the following settings: previous mediastinal +/- right chest irradiation (35%), previous aortic valve replacement (15%), all previous coronary artery bypass grafting (CABG) (5%), not all previous CABG, but only if previous right coronary artery graft or in-situ right thoracic mammary artery graft which are still patent (20%), all previous cardiac surgery (15%), previous thoracic surgery where right chest adhesions are expected (60%), and none of the above (25%).
Mitral valve-related factors
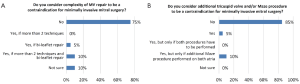
- The complexity of mitral valve repair was not considered as a contraindication to MIMVS by 50% of respondents (Figure 2A).
- Annular calcification was seen as a contraindication to MIMVS for 20% of surgeons. Nine surgeons (45%) stated that they would not perform MIMVS if a decalcification procedure (with or without a patch plasty) has to be performed. Overall, 35% of surgeons (n=7) do not consider annular calcification as a contraindication for MIMVS.
- With regard to mitral valve endocarditis, three surgeons would not perform MIMVS in this setting. Seven (35%) would perform a conventional sternotomy in cases with annular abscess formation. 50% of surgeons do not consider endocarditis as a contraindication for MIMVS.
- Participants were asked whether additional left ventricular hypertrophy requiring myectomy should be a contraindication for MIMVS. Nine surgeons (45%) answered that myectomy can be performed through minimally invasive access during mitral valve surgery. Twenty percent of surgeons would not perform this procedure during MIMVS and 25% would only when the hypertrophy is limited to the subvalvular (aortic valve) area.
- With regard to left ventricular ejection fraction (EF) as a contraindication to perform MIMVS, the answers were as follows: only if EF<30% (N=2, 10%), EF<20% (N=7, 35%), or no contraindication at all (N=11, 55%).
- An enlarged left atrium was not seen as a contraindication for MIMVS in 95% of answers.
- Eight-five per cent of surgeons do not consider additional tricuspid surgery or Maze procedure to be a contraindication to MIMVS (Figure 2B).
Surgical skills and research
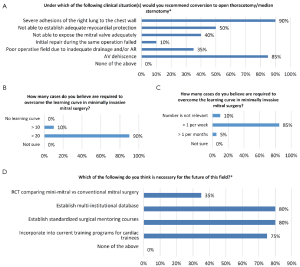
- Surgeons were surveyed regarding situations in which conversion to full sternotomy is required, with the majority recommending conversion if there are severe adhesions of the right lung to the chest wall (90%), or if aortic valve dehiscence occurs (85%) (Figure 3A).
- To overcome the learning curve in MIMVS, the majority of surgeons (90%) believed that more than 20 cases are necessary to overcome the learning curve. Two surgeons believed that more than ten cases is enough (Figure 3B).
- To maintain surgical skills for MIMVS, a surgeon should perform more than one case per week (85%) and more than one cases per month (5%). Two surgeons believed that the number of cases is not relevant at all (Figure 3C).
- All surgeons believed that some form of training and supervision is required to commence a MIMVS program safely. Specifically, they believed that wet-lab courses (65%), proctorship (70%), mini-fellowship with exposure to at least ten cases (50%), or full fellowship lasting a year (30%) are required.
- Participants were questioned regarding the future direction of MIMVS. The majority believed that a multi-institutional database (80%) and standardized surgical mentoring courses should be created (80%), and that MIMVS should to be incorporated into current training programs for cardiac trainees (75%) (Figure 3D).
Discussion
We have shown that there currently exists a broad variation in opinions with regards to contraindications, mitral valve-related factors and surgical skills for performing MIMVS. While the participating surgeons represent colleagues with proven expertise in this field, it is difficult to assess the true consensus of the entire MIMVS community. The variation in answers may mirror the individual criteria and patient selection processes of when to perform MIMVS. As some answers did not exclude any of the stated criteria to be contraindications to perform MIMVS, this may reflect the principle feasibility to perform MIMVS in almost all patients, including complex cases, re-operations and high risk patients. Indeed, we and others have demonstrated that MIMVS can be performed in complex mitral valve pathologies (2,4,6), patients with low ejection fraction (7), elderly patients (8) and even reoperations (9,10).
Owing to the relatively recent introduction of MIMVS, there exists a paucity of high-level clinical evidence for much of this field. More comparative studies are required to thoroughly evaluate the specific advantages of MIMVS over conventional mitral valve repair, especially for high risk cases such as obese patients who are known to have an increased risk for wound complications following conventional sternotomy. While there are a number of such studies in the literature (1,11), more are required to provide a conclusive answer to some of the questions posed in this survey.
The survey also evaluated situations when conversion to full sternotomy is indicated (Figure 3A). It has been demonstrated that in experienced centers the overall conversion rate of MIMVS to full sternotomy is low (6,12). This obviously requires adequate training of surgeons who perform MIMVS. At our institution, there are designated surgeons who focus on this procedure and have undergone specialized training. We have demonstrated in our series that there is a minimum of cases required to perform MIMVS to achieve adequate surgical outcomes. Additionally, we have found that it is beneficial to maintain surgical skills with an average number of cases per week (13). In the present survey, all surgeons believed the necessity of specialized training programs to provide adequate familiarity for MIMVS (Figure 3D). Intuitively, it is highly advisable to gain exposure to some expertise before one starts to build up a MIMVS program.
Complex mitral valve repair has been shown to have the same excellent results as conventional mitral valve surgery. The decision to perform MIMVS in individual patients should be based on patient profile and surgical expertise. However, it is likely that experienced surgeons will perform MIMVS as a standard procedure in almost all mitral valve surgical cases, and therefore do not specifically select the technique to a specific patient profile. Continuous training and proper education are required to achieve equal results as compared to conventional sternotomy and to benefit from the specific advantages of MIMVS, including decreased surgical trauma, less pain, better cosmesis and overall improved postoperative recovery.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Modi P, Hassan A, Chitwood WR Jr. Minimally invasive mitral valve surgery: a systematic review and meta-analysis. Eur J Cardiothorac Surg 2008;34:943-52. [PubMed]
- Seeburger J, Borger MA, Doll N, et al. Comparison of outcomes of minimally invasive mitral valve surgery for posterior, anterior and bileaflet prolapse. Eur J Cardiothorac Surg 2009;36:532-8. [PubMed]
- Goldstone AB, Atluri P, Szeto WY, et al. Minimally invasive approach provides at least equivalent results for surgical correction of mitral regurgitation: a propensity-matched comparison. J Thorac Cardiovasc Surg 2013;145:748-56. [PubMed]
- Casselman FP, Van Slycke S, Wellens F, et al. Mitral valve surgery can now routinely be performed endoscopically. Circulation 2003;108 Suppl 1:II48-54. [PubMed]
- Carpentier A, Loulmet D, Carpentier A, et al. Open heart operation under videosurgery and minithoracotomy. First case (mitral valvuloplasty) operated with success. C R Acad Sci III 1996;319:219-23. [PubMed]
- McClure RS, Athanasopoulos LV, McGurk S, et al. One thousand minimally invasive mitral valve operations: early outcomes, late outcomes, and echocardiographic follow-up. J Thorac Cardiovasc Surg 2013;145:1199-206. [PubMed]
- Santana O, Reyna J, Pineda AM, et al. Outcomes of minimally invasive mitral valve surgery in patients with an ejection fraction of 35% or less. Innovations (Phila) 2013;8:1-5. [PubMed]
- Holzhey DM, Shi W, Borger MA, et al. Minimally invasive versus sternotomy approach for mitral valve surgery in patients greater than 70 years old: a propensity-matched comparison. Ann Thorac Surg 2011;91:401-5. [PubMed]
- Murzi M, Kallushi E, Tiwari KK, et al. Minimally invasive mitral valve surgery through right thoracotomy in patients with patent coronary artery bypass grafts. Interact Cardiovasc Thorac Surg 2009;9:29-32. [PubMed]
- Seeburger J, Borger MA, Falk V, et al. Minimally invasive mitral valve surgery after previous sternotomy: experience in 181 patients. Ann Thorac Surg 2009;87:709-14. [PubMed]
- Lucà F, van Garsse L, Rao CM, et al. Minimally invasive mitral valve surgery: a systematic review. Minim Invasive Surg 2013;2013:179569.
- Vollroth M, Seeburger J, Garbade J, et al. Minimally invasive mitral valve surgery is a very safe procedure with very low rates of conversion to full sternotomy. Eur J Cardiothorac Surg 2012;42:e13-5; discusson e16.
- Holzhey DM, Seeburger J, Misfeld M, et al. Learning minimally invasive mitral valve surgery: a cumulative sum sequential probability analysis of 3895 operations from a single high-volume center. Circulation 2013;128:483-91. [PubMed]





