How to start a minimal access mitral valve program
Attending international meetings provides the inspiration to improve and progress one’s own practice, but we have to understand that the presenters will be experienced and well-practised and they will inevitably make it look easy. With appropriate training and experience it will become “easy”, but even the best surgeons in the world have to climb the learning curves. I will discuss the process of introducing a new procedure to a hospital and the learning curves for minimal access mitral valve surgery, with a few ideas on how to make these curves as short as possible.
In the National Health Service (NHS) in the United Kingdom, we have the seven pillars of governance (Figure 1). These were developed as a framework for good practice which is patient-centred and hence, the over-riding roof for the seven pillars is the patient-professional relationship. Underpinning the pillars are systems awareness, teamwork, communication, ownership and leadership, all of which are paramount to performing any surgery but more so with minimal access surgery, as will be highlighted throughout this paper. In selling the idea to administrators, the seven pillars are a useful guide.
Clinical effectiveness has to be proven. There is a wealth of literature which supports the effectiveness of minimal access surgery and they are sited and subjected to meta-analysis elsewhere in this journal. You should be able to quote the literature and present it to the administrators but in a way that they will find most interesting. In the NHS, length of hospital stay is of paramount importance and any reduction will be seen as positive. There will also be cost savings related to stay in intensive care unit (ICU), use of blood products and prescription of analgesia.
Risk management effectiveness has to be considered. The overall risks are probably lower than sternotomy cases but you will have to consider the learning curve and risks that are unique to this procedure. During the learning curve it is essential that you and your team have a clear understanding of time limits. If the procedure is not progressing you should have a pre-arranged plan for either extending the thoracotomy or converting to a sternotomy. This is best agreed upon before starting because the surgeon may not be watching the clock and it is safer for the patient. This will also have to be included in the consent process with the patient. Risks unique to the procedure should be considered and the worst is probably aortic dissection, although this is rare. It certainly has been reported in the early experience with the endoballoon but technology and techniques have improved. I have had one case but it was entirely iatrogenic (i.e., my fault!). I felt some resistance with the guide wire but then the resistance eased. The result was clearly evident on the trans-oesophageal echocardiogram (TEE). I immediately withdrew the wire and reversed the heparin and a subsequent CT scan demonstrated an almost resolved local dissection. After waiting a few weeks the patient underwent surgery via a sternotomy. I found solace and sympathy from the cardiologists, almost all of whom said that they have had similar sphincter tightening experiences. Nonetheless the lesson to stop with any resistance was learnt. You may read this and think this is obvious but there will be many other lessons to learn.
Patient experience is important to all. The same result with better cosmesis will be important to many patients, but in my experience a shorter recovery and quicker return to work is usually of greater importance. Patients will be your greatest advocates and therefore honesty will be the best approach. They should be given a summary of the procedure including the risks as well as the benefits, but it should also include an outline of your training program including the steps you have taken to minimise the risks and shorten the learning curves.
Communication effectiveness is overreaching as it not only involves your team but the entire unit and the patients. I think choosing a team for the first 20 or so cases is essential. You can then entrust each team member [anaesthetist, perfusionist, theatre (OR) nurses, ICU nurses, ward nurses and outpatient nurses] to communicate and educate each of their areas. Agreeing on procedures (e.g., time to conversion to larger incision or sternotomy) before starting the program is essential. I make no apologies for repeating this but I am aware of surgeons who have got into difficulty by persisting with a truly minimal access (and totally thorascopic approach) for hours and the outcome was death of the patient.
Resource effectiveness is something no administrator likes to hear but how much will it cost? This will obviously depend upon the hospital. If you already have HD stacks and the appropriate range of scopes then the costs will be considerably less. The minimal access instruments and retractors (Figure 2) will need to be purchased. Most of the costs are capital costs and the disposable costs for each procedure can be offset against the cost savings you have already identified. However there is no cheap alternative for quality! The bodies that ultimately fund the procedure (insurance companies, government etc.) need to be aware of your program and the costs to them (initially the same as sternotomy cases).
Strategic effectiveness covers two main areas. The first is audit, which also covers many of the other pillars. Audit of your outcomes, procedure time, patient hospital stay, patient recovery, patient satisfaction and the obvious negative outcomes should be continuous and repeated to demonstrate progression along the learning curves. Audit can obviously and rightly be included in all of the pillars. The second will be where you will be in one, five and ten years’ time. Will every surgeon in your hospital be contributing to the minimal access program (not all minimal access cardiac surgery is mitral)? Will you consider tricuspid valve surgery? Will you consider atrial septal defect surgery (that is not suitable for device closure)? Will you consider surgery for atrial myxomas or other atrial tumours? Such a visionary portfolio for your institution will be valued by the administrators.
Learning effectiveness includes education and training. Having a dedicated team to begin with is vital. The surgeon will have enough to think about when commencing a minimal access program without having to concentrate on other areas (e.g., anaesthesiology or perfusion). The training and education of others can proceed at pace once the original team are completely comfortable with the procedure. Having complete trust in the team will promote effective and positive teamwork. It will also give all the team ownership of the project. If during a procedure any of the team calls “halt”, then the whole team should stop and address the concern. Often it will be minor but it could be life-threatening and two minutes taken to listen to another member of the team irrespective of seniority will be two minutes well spent. It is always valuable to have a de-briefing session at the end of a procedure with every team member contributing to consider ways of improving. This not only shortens the inevitable learning curves but also reinforces ownership of the process by each team member. I believe that it is invaluable to have your entire team visit a centre that has an established program where you can pair up with your counterparts and learn first-hand. When you start your program, an established surgeon and perfusionist should attend your institution as proctors. Most companies involved with minimal access surgery have training programs which follow this model. The proctors can attend until the team are comfortable with the entire procedure. The companies often have their own training team who can attend for longer and their experience and understanding is always gratefully received. I took my team to Barcelona where in 2003 Professor Greco (now in Rome) was practising.
The surgeon is the leader of the team and this has to be recognised, but each team member should be chosen so they can be leaders of their own area, which again gives ownership of the process to each individual. This will produce greater interest from the new team members who will want to be involved with the second phase of the training program and volunteer for new training programs.
For the readers familiar with the NHS I must point out that I decided to use the original seven pillars of governance. The underpinning and the roof remain the same but the pillars have changed to audit, clinical effectiveness, risk management, patient/service user & public involvement, education & training, information management and staff management. I prefer the original pillars and they essentially cover all the same areas. The new pillars make direct reference to the “payers” (i.e., insurance companies, government, etc.). These have varying importance in different health systems but all the arguments outlined above still apply.
The second part of this article will concentrate on the learning curves and how they can be shortened. I believe there are (at least) seven new learning curves (Table 1) and it is unlikely that experienced cardiac surgeons have encountered as many in one procedure since the days of their own training. Nonetheless, recognition of these learning curves and considering the ways of shortening them will make the introduction of minimal access mitral valve surgery a less stressful experience.
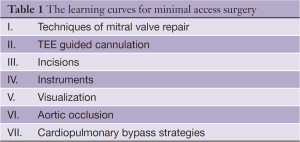
Full table
Mitral valve repair
This may be obvious but one should not embark on a minimal access program if one is unfamiliar with the mitral valve. The majority (over 90%) of degenerative mitral valves should be repaired and the techniques of repair should not be part of the learning curve for minimal access surgery. It is wise to be selective initially and sticking to straight forward P2 prolapse for the first twenty or so cases would be advisable because these are the most common of cases with which most surgeons would be comfortable. Do not try to change technique for the minimal access cases; the surgeon will have enough to be concerned with! When the surgeon is comfortable and relaxed with the whole minimal access procedure, he/she can perform any procedure on the mitral valve that they would attempt via a sternotomy approach. Remember it is far easier to learn to walk before running.
TEE guided cannulation
It is now more frequent than not that the anaesthetist is competent with the TEE. The specific views required for cannulation are a bicaval view, a long axis aortic root view and a short axis view of the descending aorta. The anaesthetist will also be required to measure the diameter of the ascending aorta if an endoballon is to be used. With patient consent it is reasonable to practise with the femoral cannula (percutaneously) in sternotomy cases or try the cannulae for redo cases.
Incisions
This will probably be the shortest and least concerning learning curve. Most surgeons will have performed thoracotomies and groin dissection for cannulation. The aim is, however, to achieve a thoracotomy incision that is less than five cm in length, which will require careful thought with regards to positioning. Initially the incisions will be larger—8 to 10 cm—but the ribs will not be spread so the positioning is important. Too high and it will be difficult siting the port for the thoracoscope in the same rib space, which is important as one of the aims will be to reduce the number of dermatomes that contribute to post-operative pain. Too low and the diaphragm will impair access. The diaphragm can be retracted but only within reason. Too anterior and the atrial retractor will impair access to the mitral valve. Too posterior and access to the valve will be difficult. Most incisions are centred on the nipple a centimetre below the areola with either the 4th or the 5th intercostal space entered. The groin access is also worth considering as it seems contrary to have a small chest incision if the groin incision is large. I usually make a 3 to 4 cm incision in the groin crease at the level of the inguinal ligament with minimal dissection of the femoral vessels. Many surgeons perform the femoral cannulation percutaneously.
Instruments
The instruments for minimal access surgery are all single shafted (Figure 2) and the ergonomics are different to standard instruments. This is the easiest learning curve to shorten. Simply using the instruments in a sternotomy case will rapidly increase familiarity and make the transition to minimal access use seamless.
Visualization
This may be unfamiliar to many cardiac surgeons but practice will improve your skill. During sternotomy cases, after becoming comfortable with the single shafted instruments, it is simple to cover the wound with towels and position a thoracoscope beneath the towels (Figure 3). The open procedure can be performed partly or wholly using the thoracoscope. The view (and access) is much superior via a mini-thoracotomy but this will definitely shorten the learning curve.
Aortic occlusion
Whether it is with a clamp or an endoballon, aortic occlusion will be unfamiliar and this is the only learning curve that the surgeon has to climb entirely during minimal access cases.
Cardio-pulmonary bypass strategies
Venous drainage usually requires vacuum assistance and this is not in common use but can be tried during sternotomy cases. The biggest mistake is to simply increase the vacuum if the drainage is sub-optimal because there may be a problem with the position of the cannula; this requires communication. The femoral artery cannulae may have higher line pressures than those seen in the ascending aorta, especially if the patient is small and an endoballon has been passed through the cannula. There are strategies for managing this problem but these need to be discussed before starting a minimal access case. With the endoballoon, the perfusionist will be required to monitor the balloon pressure and be aware and communicate when there is a change as this may signify that the balloon has moved.
This is a short and concise guide to starting a minimal access program. I apologise if I have missed any important steps as there may be issues that are institution or country specific. The most important learning points are knowing how to reduce the learning cases and practising with the instruments and visualization in sternotomy cases as a sure way of enjoying the experience of starting a minimal access program.
Acknowledgements
Disclosure: The author declares no conflict of interest.