Chordae replacement versus leaflet resection in minimally invasive mitral valve repair
Introduction
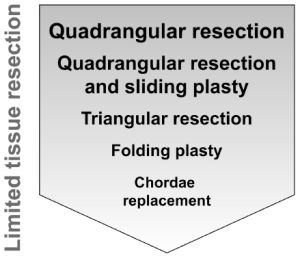
A systematic functional approach to mitral valve (MV) reconstruction was introduced by Carpentier as early as 1969 (1) and has since demonstrated excellent long-term outcomes (2). The continual evolution of mitral valve repair (MVR) and the need for improvement have led to multiple proposed modifications of the original techniques. The classic quadrangular resection technique initially proposed by Carpentier to treat prolapse of the posterior MV leaflet became the gold standard, and is still widely used at present (3,4). This technique is commonly combined with either plication of the mitral annulus, sliding annuloplasty or folding plasty (5-7). Although very safe and effective, these techniques do not respect the anatomy of the MV, and the physiological role of the posterior leaflet (8). Therefore new techniques have been proposed with the aim of preserving the MV leaflets to a greater extent. Triangular resection of the prolapsing posterior leaflet has been reported as a good alternative that significantly reduces the size of resection and thus largely eliminates the need for annular plication or sliding annuloplasty, procedures which are often required with quadrangular resection (9-11) (Figure 1).
The “respect rather than resect” techniques of MVR emerged some years later following the introduction of the original “resection” techniques. The underlying principles are based on the use of expanded polytetrafluoroethylene (ePTFE) neochordae which support the free edge of the prolapsing segments of the MV, as first reported by Frater and David in the mid-80s (12,13). A modification of this technique using premeasured ePTFE loops (“loop technique”) was introduced to facilitate implantation of neochordae (14). In addition, some other “non-resection” techniques such as folding valvuloplasty or leaflet remodeling MVR have been reported (15,16) (Figure 1).
Both types of approaches can be readily applied both in open and minimally invasive mitral valve repair. Despite the fact that the “resection” techniques are associated with excellent long-term results, there is growing evidence that “non-resection” techniques may be advantageous.
“Resection” techniques in MVR
In a milestone paper published in 1983, Carpentier summarized his collective experience with mitral valve reconstruction using the so-called “French correction” (5). He developed and elaborated a functional approach to MVR with the aim of providing sufficient leaflet coaptation and annular remodeling. One of the most important techniques proposed by Carpentier to treat prolapse of the posterior leaflet was quadrangular resection (1). This technique was originally combined with either plication of the mitral annulus or sliding annuloplasty to compensate for the often large area of resection that did not allow for a direct closure of the remnant leaflet margins. MVR was then accomplished in almost all cases by prosthetic ring annuloplasty (5). Long-term outcomes were excellent with a late mortality rate of 7% and a 9-year survival of 82% in patients with isolated MVR. Only 11% of the patients underwent reoperation due to residual or recurrent mitral regurgitation (MR). These data were supported by publication of very long-term results with a 20-year survival rate of 48%, equal to the survival rate for a normal age- and sex-matched population (17).
Johnston (4) published the experience from the Cleveland Clinic with 3,383 patients undergoing surgery for isolated posterior mitral leaflet prolapse. 3,074 quadrangular resections with or without sliding plasty and by prosthetic ring annuloplasty were performed with a repair rate of 97%. The in-hospital mortality was 0.1%, and 1-, 5-, 10-, and 15-year survival rates were 99%, 96%, 87%, and 76%, respectively, superior to the age- and sex-matched US population. Freedom from mitral reoperation was 97%, and 77% of patients had no or grade 1 MR at ten years. Recently Nardi et al. (3) reported, in a cohort of 261 patients with MVR for degenerative MR, triangular or quadrangular resections of the posterior leaflet and additional annuloplasty with ring implantation were performed in 46% of patients. The in-hospital mortality was 0.8% and 10-year survival was 89%, which is at least similar to the general Italian population matched for age and sex. Freedom from mitral reoperation was 95%, and 85% patients had no MR greater than grade 2 at ten years. Furthermore, Gazoni et al. (10) published data on 154 non-consecutive patients who underwent isolated triangular resection of either the posterior or anterior leaflet accomplished by prosthetic annuloplasty for degenerative mitral disease. The 30-day mortality was 0%, and 5-year survival rate was 98.5%. The 5-year freedom from reoperation for recurrent MR was 99%.
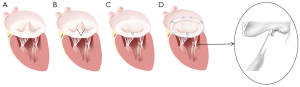
Besides the studies mentioned above, it has been well demonstrated in other publications that MVR using Carpentier’s techniques or their modifications yields excellent short- and long-term results (18,19). However, some potential disadvantages of resection techniques have been postulated. After extensive resection, the posterior leaflet mobility is often largely impaired, leading to a functional monocusp valve. On Doppler flow echocardiography, the stiff posterior leaflet remnant leads to a typical inflow pattern with flow acceleration and turbulence across the posterior leaflet. Extensive resection may also decrease the surface of coaptation, which is thought to be essential for a longstanding and good repair result (20). Changes in annular geometry and dimension are additional consequences, the latter leading to smaller size annuloplasty ring implants (Figure 2).
“Respect rather than resect” techniques in MVR
The use of polytetrafluoroethylene (ePTFE) as neochordae to restore support to the free edge of prolapsing segments in MVR was introduced experimentally by Frater in 1986 (12) and adopted early on by David (13). In the meantime, this material has been used in many different techniques, as reviewed comprehensively by Ibrahim in 2012 (21). An important modification of the standard use of ePTFE in creating neochordae has been proposed by Mohr et al. in 2000 (14). The so-called “loop technique” uses four premade ePTFE loops to facilitate chordal replacement, particularly when MVR is performed minimally invasively (22-24).
David published a 25-year experience of chordal replacement with ePTFE sutures for MVR used to repair anterior and posterior leaflet prolapse (25). The in-hospital mortality was 0.8%, and survival at 1, 10, and 18 years was 98%, 86%, and 67%, respectively. Freedom from mitral reoperation was 95% and 88% patients had no MR greater than grade 2 at ten years. Perier (26) reported his data of 225 patients who underwent MVR due to isolated posterior leaflet prolapse aiming to “transform the posterior leaflet into a smooth vertical buttress without resection”, and coined the term of a “respect rather than resect” approach. The in-hospital mortality rate was 1.3%, and 10-year survival was 88%. Freedom from mitral reoperation was 93% at ten years. Kuntze et al. (27), in a cohort of 632 patients undergoing MVR, reported the use of ePTFE chordal replacement (“loop technique”) to treat anterior and/or posterior leaflet prolapse. The majority of patients (83%) underwent a minimally invasive technique via right anterolateral mini-thoracotomy. The 30-day mortality rate was 1.4%, and 6-year survival was 86%. Freedom from mitral reoperation was 96% at six years.
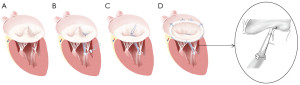
There is clear evidence that MVR using ePTFE chordal replacement technique and its various modifications can provide excellent short- and long-term results (21). It has been postulated that a “non-resection” technique is associated with (I) preserved leaflet mobility; (II) larger surface of coaptation; (III) no or only very limited changes to the annular geometry; and (IV) may allow for the implantation of larger prosthetic annuloplasty rings (Figure 3).
“Resection” versus “respect rather than resect” techniques in MVR
There are some studies comparing both approaches. In 2009, Padala et al. (28) published a very interesting bench experiment using an in vitro heart simulator to compare quadrangular resection versus triangular resection versus neochordoplasty in the setting of posterior leaflet prolapse resulting from chordal rupture. Although they found comparable hemodynamics in all three repairs, valve function and leaflet kinematics were significantly better after non-resection or limited resection techniques. Complete restoration of normal coaptation length was found only with chordal replacement. To date, there is only one small prospective randomized trial comparing the use of ePTFE neochordae for posterior mitral valve prolapse (“loop technique”) versus leaflet resection in 129 patients (29). Patients operated on using a minimally invasive technique had a repair rate of 100%, while both techniques resulted in good echocardiographic outcomes with low rates of morbidity and mortality. The only statistically significant finding was that patients undergoing the loop technique had a longer line of leaflet coaptation. In a retrospective comparison between chordae replacement (“loop technique”) and resection for repair of isolated posterior leaflet prolapse within a cohort of 1,708 patients undergoing minimally invasive MVR (30), the implanted annuloplasty ring size was significantly larger in the loop group than in the resection group. This supports the notion that in the absence of a large resection and unaltered annular geometry, larger rings can be implanted. This may allow for the biggest possible MV orifice area and hence provide lower gradients especially under exercise conditions. These findings were confirmed by Lange, who compared data of 397 patients who underwent either quadrangular resection or chordal replacement for repair of posterior leaflet prolapse (31). The authors found that while both techniques were equally effective, the chordal replacement technique permitted the use of larger size annuloplasty rings. The conclusion of both studies was that chordal replacement offers a potentially superior physiological repair with preserved leaflet mobility, and can be performed with excellent mid-term results and a low incidence of reoperation. Very recently, a comparison of both techniques for robotic posterior mitral leaflet repair due to degenerative disease has been reported by Mihaljevic et al. (24). The resection and neochordae groups consisted of 248 and 86 patients, respectively, and outcomes were compared using propensity score matching. Repair rate was 100% and there was no in-hospital mortality. The authors concluded that robotic posterior mitral leaflet repair with neochordae is associated with shorter operative times and no occurrence of systolic anterior motion (SAM) compared to the resection technique. The versatility, effectiveness and safety justify this repair approach as a good choice for patients with advanced multisegment disease.
Conclusions
Both the “resection” and “non-resection” techniques of MVR have been shown to have comparable excellent short-, mid- and long-term results in open but also in minimally invasive or robotic approaches. There is growing evidence showing that the “non-resection” technique has some potential advantages including: (I) preserved leaflet mobility; (II) larger surface of coaptation; (III) no changes in annular geometry; and (IV) implantation of larger prosthetic annuloplasty ring. The “respect rather than resect” approach may therefore find widespread utilization in the near future.
Acknowledgements
The authors want to thank Mr. Stefan Schwyter for his tremendous efforts in preparing the medical illustrations.
Disclosure: The authors declare no conflict of interest.
References
- Carpentier A. Reconstructive valvuloplasty. A new technique of mitral valvuloplasty. Presse Med 1969;77:251-3. [PubMed]
- Carpentier A, Chauvaud S, Fabiani JN, et al. Reconstructive surgery of mitral valve incompetence: ten-year appraisal. J Thorac Cardiovasc Surg 1980;79:338-48. [PubMed]
- Nardi P, Pellegrino A, Scafuri A, et al. Survival and durability of mitral valve repair surgery for degenerative mitral valve disease. J Card Surg 2011;26:360-6. [PubMed]
- Johnston DR, Gillinov AM, Blackstone EH, et al. Surgical repair of posterior mitral valve prolapse: implications for guidelines and percutaneous repair. Ann Thorac Surg 2010;89:1385-94. [PubMed]
- Carpentier A. Cardiac valve surgery--the “French correction”. J Thorac Cardiovasc Surg 1983;86:323-37. [PubMed]
- Jebara VA, Mihaileanu S, Acar C, et al. Left ventricular outflow tract obstruction after mitral valve repair. Results of the sliding leaflet technique. Circulation 1993;88:II30-4. [PubMed]
- Grossi EA, Galloway AC, Kallenbach K, et al. Early results of posterior leaflet folding plasty for mitral valve reconstruction. Ann Thorac Surg 1998;65:1057-9. [PubMed]
- Dreyfus GD, Corbi P, Rubin S, et al. Posterior leaflet preservation in mitral valve prolapse: a new approach to mitral repair. J Heart Valve Dis 2006;15:528-30. [PubMed]
- Suri RM, Orszulak TA. Triangular resection for repair of mitral regurgitation due to degenerative disease. Op Tech Thorac Cardiovasc Surgery 2005;10:194-9.
- Gazoni LM, Fedoruk LM, Kern JA, et al. A simplified approach to degenerative disease: triangular resections of the mitral valve. Ann Thorac Surg 2007;83:1658-64; discussion 1664-5.
- George KM, Mihaljevic T, Gillinov AM. Triangular resection for posterior mitral prolapse: rationale for a simpler repair. J Heart Valve Dis 2009;18:119-21. [PubMed]
- Frater RW. 10th goretex chorda anniversary. J Heart Valve Dis 1996;5:348-51. [PubMed]
- David TE. Replacement of chordae tendineae with expanded polytetrafluoroethylene sutures. J Card Surg 1989;4:286-90. [PubMed]
- von Oppell UO, Mohr FW. Chordal replacement for both minimally invasive and conventional mitral valve surgery using premeasured Gore-Tex loops. Ann Thorac Surg 2000;70:2166-8. [PubMed]
- Mihaljevic T, Blackstone EH, Lytle BW. Folding valvuloplasty without leaflet resection: simplified method for mitral valve repair. Ann Thorac Surg 2006;82:e46-8. [PubMed]
- Woo YJ, Macarthur JW Jr. Simplified nonresectional leaflet remodeling mitral valve repair for degenerative mitral regurgitation. J Thorac Cardiovasc Surg 2012;143:749-53. [PubMed]
- Braunberger E, Deloche A, Berrebi A, et al. Very long-term results (more than 20 years) of valve repair with carpentier’s techniques in nonrheumatic mitral valve insufficiency. Circulation 2001;104:I8-11. [PubMed]
- Mohty D, Orszulak TA, Schaff HV, et al. Very long-term survival and durability of mitral valve repair for mitral valve prolapse. Circulation 2001;104:I1-7. [PubMed]
- DiBardino DJ, ElBardissi AW, McClure RS, et al. Four decades of experience with mitral valve repair: analysis of differential indications, technical evolution, and long-term outcome. J Thorac Cardiovasc Surg 2010;139:76-83; discussion 83-4. [PubMed]
- David TE, Armstrong S, Mccrindle BW, et al. Late outcomes of mitral valve repair for mitral regurgitation due to degenerative disease. Circulation 2013;127:1485-92. [PubMed]
- Ibrahim M, Rao C, Athanasiou T. Artificial chordae for degenerative mitral valve disease: critical analysis of current techniques. Interact Cardiovasc Thorac Surg 2012;15:1019-32. [PubMed]
- Seeburger J, Kuntze T, Mohr FW. Gore-tex chordoplasty in degenerative mitral valve repair. Semin Thorac Cardiovasc Surg 2007;19:111-5. [PubMed]
- Gillinov AM, Banbury MK. Pre-measured artificial chordae for mitral valve repair. Ann Thorac Surg 2007;84:2127-9. [PubMed]
- Mihaljevic T, Pattakos G, Gillinov AM, et al. Robotic posterior mitral leaflet repair: neochordal versus resectional techniques. Ann Thorac Surg 2013;95:787-94. [PubMed]
- David TE, Armstrong S, Ivanov J. Chordal replacement with polytetrafluoroethylene sutures for mitral valve repair: a 25-year experience. J Thorac Cardiovasc Surg 2013;145:1563-9. [PubMed]
- Perier P, Hohenberger W, Lakew F, et al. Toward a new paradigm for the reconstruction of posterior leaflet prolapse: midterm results of the “respect rather than resect” approach. Ann Thorac Surg 2008;86:718-25; discussion 718-25. [PubMed]
- Kuntze T, Borger MA, Falk V, et al. Early and mid-term results of mitral valve repair using premeasured Gore-Tex loops (‘loop technique’) Eur J Cardiothorac Surg 2008;33:566-72. [PubMed]
- Padala M, Powell SN, Croft LR, et al. Mitral valve hemodynamics after repair of acute posterior leaflet prolapse: quadrangular resection versus triangular resection versus neochordoplasty. J Thorac Cardiovasc Surg 2009;138:309-15. [PubMed]
- Falk V, Seeburger J, Czesla M, et al. How does the use of polytetrafluoroethylene neochordae for posterior mitral valve prolapse (loop technique) compare with leaflet resection? A prospective randomized trial. J Thorac Cardiovasc Surg 2008;136:1205; discussion1205-6.
- Seeburger J, Falk V, Borger MA, et al. Chordae replacement versus resection for repair of isolated posterior mitral leaflet prolapse: à ègalité. Ann Thorac Surg 2009;87:1715-20. [PubMed]
- Lange R, Guenther T, Noebauer C, et al. Chordal replacement versus quadrangular resection for repair of isolated posterior mitral leaflet prolapse. Ann Thorac Surg 2010;89:1163-70; discussion 1170. [PubMed]





