Frozen elephant trunk surgery in type B aortic dissection
Introduction
The frozen elephant trunk (FET) technique combines surgical replacement of the aortic arch with simultaneous stenting of the descending thoracic aorta. This approach has been rarely indicated in patients with type B aortic dissection (TBAD). We herein report on our experience with FET surgery in selected TBAD patients.
Methods
Patients
Between January 2007 and July 2012, 19 TBAD patients (acute =1; chronic =18) underwent complete arch replacement with FET at our institution. The mean age was 58±11 years; 18 patients were male, four had undergone previous cardiac or aortic procedures, and two were operated on emergently. The dissection process involved the entire thoraco-abdominal aorta in all cases and extended to the iliac arteries in seven. The proximal intimal tear was located in the proximal descending thoracic aorta in all cases. The maximal diameter of the descending thoracic aorta was 51±9 mm; the maximal diameters of the ascending aorta and aortic arch aorta were 44±10 mm, and 43±11 mm, respectively. The remaining two patients had no suitable vascular access for TEVAR. Additional intimal tears on the left subclavian artery, which would have prevented optimal false lumen exclusion after TEVAR, were an indication for the FET technique in the remaining patient with acute dissection.
Surgical techniques
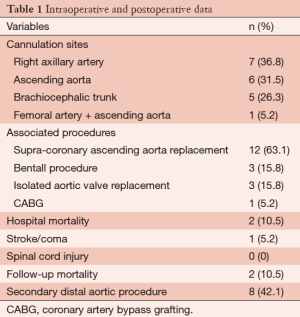
Our technique for complete arch replacement with FET has already been described (1). The E-vita Open and E-vita Open Plus (JOTEC® GmbH, Germany) were used in all cases for the FET construction. Median sternotomy was used to approach the aorta in all cases; cardiopulmonary bypass (CPB) was established using the right axillary artery, brachiocephalic trunk, proximal arch or femoral artery for arterial CPB inflow, and the right atrium or the femoral vein as venous drainage. Antegrade selective cerebral perfusion (ASCP) and moderate hypothermia (26 °C) were used for brain protection. After arch resection, the proximal descending aorta was prepared with obliteration of the false lumen. The stent-graft system was introduced and released in an antegrade fashion into the true lumen of the descending aorta over the previously positioned stiff guide-wire. The incorporated Dacron graft was pulled back and sutured to the previously prepared descending aorta. The arch vessels were re-implanted using an E-vita Open Plus graft or a separate graft when the E-vita Open was employed. The proximal anastomosis is usually completed the aortic repair. Associated cardiac or aortic procedures are shown in Table 1. Mean CPB and ASCP times were 215.2±41.9 minutes and 82.2±26.6 minutes, respectively.
Full table
Statistical analysis
Continuous variables were expressed as the mean ±1 standard deviation (SD) and categorical variables as percentages.
Results
Two patients died due to multi-organ failure. Postoperatively, one patient suffered from a coma, while there were no cases of spinal cord injury.
Two patients died during follow-up (100% complete; mean time ± SD: 22±13 months), one from aortic rupture during an emergent abdominal aortic stenting procedure, the other from an unknown cause. Of the 17 surviving patients, eight underwent secondary distal aortic procedures (TEVAR in six, infra-renal abdominal aorta stent-graft repair in one, and abdominal aorta replacement in one patient).
Discussion
In patients with complicated acute and chronic TBAD, TEVAR is acknowledged as the mainstay of therapy (2). However, anatomical conditions such as a proximal landing zone >40 mm, an angulated aortic arch or a dissected left subclavian artery with additional distal intimal tears (which may maintain perfusion of the false lumen despite correct stent-graft deployment), may hamper TEVAR and necessitate alternative procedures. In this setting, aortic graft replacement of the descending thoracic aorta through a left thoracotomy represents the most common procedure offered.
We have extended the use of FET surgery to selected patients with TBAD, and used it as an alternative to standard open surgery. In our experience, anatomic contraindications to TEVAR represented an indication for the FET technique in all cases. In our series of 19 patients, concomitant proximal aneurysmal disease (Figure 1) was present in 16 cases, unsuitable vascular access in two cases, and severe involvement of the left subclavian artery in one patient. Of note, four patients underwent an associated Bentall procedure, four underwent an aortic valve replacement, and one underwent coronary artery bypass grafting (CABG). These data demonstrate the added value that the FET technique can offer as compared to standard open surgery—namely the opportunity to treat, with a single intervention, concomitant aneurysms of the proximal thoracic aorta. We also believe that in TBAD patients, the FET technique, by allowing graft replacement of the aortic arch and ascending aorta, eliminates the risk of retrograde ascending aortic dissection. This infrequent but catastrophic complication, which has extremely high mortality (approximately 40%), is most prone in TEVAR-managed TBAD patients (3).

In our limited series of 19 patients, early outcomes were satisfactory as demonstrated by hospital mortality, stroke and spinal cord injury rates of 10.5%, 5.2% and 0%, respectively. A recent systematic review which reported on a subgroup of chronic TBAD patients undergoing open surgery a pooled early mortality rate of 8.0% and pooled rates of early stroke and spinal cord ischemia of 5.7% and 5.5%, respectively. The pooled early mortality rate for TEVAR in TBAD was 6.6%; pooled rates of early stroke and spinal cord ischemia were 1.9% and 1.5%, respectively (2). While we acknowledge that no definitive conclusions can be drawn by a case series such as ours, we believe that the excellence of our results using the FET technique compares favorably with those reported after the less extensive TEVAR and open surgical interventions in this setting.
It is well known that patients with chronic TBAD, compared to those with acute dissections, have less potential for aortic remodeling and more often require late surgical or stent-graft re-interventions (4). Considering that 18 out of 19 patients were treated for chronic TBADs, our results in terms of distal aorta remodeling rates and freedom from distal re-interventions, are in line with those obtained by TEVAR.
In conclusion, our data showed the feasibility and safety of the FET technique in selected TBAD patients.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Di Bartolomeo R, Pacini D, Savini C, et al. Complex thoracic aortic disease: single-stage procedure with the frozen elephant trunk technique. J Thorac Cardiovasc Surg 2010;140:S81-5; discussion S86-91.
- Fattori R, Cao P, De Rango P, et al. Interdisciplinary expert consensus document on management of type B aortic dissection. J Am Coll Cardiol 2013;61:1661-78. [PubMed]
- Eggebrecht H, Thompson M, Rousseau H, et al. Retrograde ascending aortic dissection during or after thoracic aortic stent graft placement: insight from the European registry on endovascular aortic repair complications. Circulation 2009;120:S276-81. [PubMed]
- Eggebrecht H, Nienaber CA, Neuhäuser M, et al. Endovascular stent-graft placement in aortic dissection: a meta-analysis. Eur Heart J 2006;27:489-98. [PubMed]





