Partial thrombosis of the false lumen influences aortic growth in type B dissection
Background
In the acute setting, the majority of patients affected by uncomplicated acute type B aortic dissection (ABAD) can be managed with medical therapy. In these patients, in-hospital outcome is generally acceptable, with mortality rates of 1-10% (1,2). However, long-term outcomes in this group is less positive, with a mortality rates reported as 20- 25% within 3 years. Predictors of long-term complications have been a highly debated topic in recent years.
Reports from the International Registry of Acute Aortic Dissection (IRAD) have shown that a partially thrombosed false lumen is associated with increased surgical mortality. Among ABAD patients discharged alive, those presenting with a partially thrombosed false lumen had an increased rate of mortality, after adjusting for age, gender and type of in-hospital treatment (3). One hypothesis for this observation is that partial thrombosis of the false lumen may occlude distal re-entry tears (“sac formation”), resulting in higher diastolic pressure (4). The purpose of this study was to determine whether partial thrombosis of the false lumen in ABAD patients is associated with increased aortic expansion (5).
Methods and patients
Patients
Imaging studies of all uncomplicated type B dissection patients admitted to four referral centers between 1998 and 2011 were analyzed for this study.
Interventions
All ABAD patients received medical anti-hypertensive therapy according to the local protocol.
Objectives
To investigate the influence of a partially thrombosed false lumen on aortic growth in medically treated ABAD patients.
Methodology
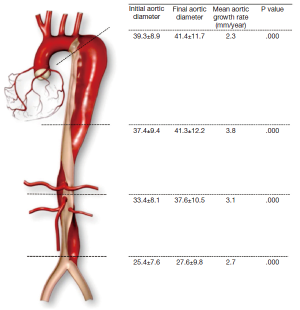
All imaging studies, either CT or MRI, at admission (<7 days after symptom onset) and follow-up (>3 months), were selected for analysis, and diameters of the affected aortas were measured at the following levels: proximal descending aorta, defined as the level 2 cm below the origin of the left subclavian artery; distal descending aorta, defined as 20 cm below the origin of the left subclavian artery; visceral aorta, between the origin of the celiac trunk and superior mesenteric artery; and infra-renal aorta, measured below the origin of the most distal renal artery (Figure 1). The annual aortic growth rate was calculated at each affected level by dividing the difference in maximum aortic diameter in millimeters between the initial and final measurements by the time interval between both imaging examinations in years.
Results
Eighty-four patients were included, of which 40 (47.6%) had a partially thrombosed false lumen, 7 patients (8.3%) a completely thrombosed false lumen, and 37 patients (44.0%) a patent false lumen. Median length of follow-up was 19.5 months (IQR 43.7, range, 1-149.5 months). A total of 273 of the 336 (81.3%) evaluated aortic levels were dissected. The mean aortic diameter at baseline was significantly larger in the partial lumen thrombosis group (38.0±12.0) compared to the complete thrombosis group (35.2±8.4), and the patent false lumen group (32.0±6.9, P<0.001). The mean aortic expansion rate was 3.0±8.1 mm/year, with significant growth at all levels (Figure 1). Mean annual aortic growth rates were 4.3±10.2 mm/year in the partial thrombosis group, 2.1±5.6 mm in the segments with a patent false lumen and 1.5±5.6 in those with a completely thrombosed false lumen.
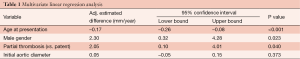
Univariate analysis showed that age, male gender and partial thrombosis of the false lumen (vs. patent false lumen) had a significant effect on the annual aortic growth rate (P<0.05 in all). Annual aortic expansion was significantly larger in patients with a partially thrombosed false lumen compared to patent false lumen (P=0.035). No significant difference between the annual aortic growth rates of dissections with a partially thrombosed false lumen and completely thrombosed false lumen were observed (P=0.745). Multivariate analyses showed that older age at presentation had a 0.17 mm per year decrease in aortic growth with every year increase in age. (95% CI, –0.026 to –0.08, P<0.001). Partial lumen thrombosis resulted in a 2.05 mm/year increase in aortic growth compared with patients with a patent false lumen (95% CI, 0.10 to 4.01, P=0.040) (Table 1).
Full table
The findings of the present study should be viewed in light of its limitations. We did not include other morphologic characteristics of the aortic dissection, which may have affected the aortic growth, except for the status of the false lumen. Also, clinical data regarding baseline co-morbidities and medical treatment were not available for analysis.
Clinical bottom line
The aortic growth rate among ABAD patients with a partially thrombosed false lumen appears to be higher during follow-up when compared to patients with complete thrombosis or a patent false lumen. These patients may require more intensive follow-up and prophylactic aortic interventions.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Elefteriades JA, Lovoulos CJ, Coady MA, et al. Management of descending aortic dissection. Ann Thorac Surg 1999;67:2002-5; discussion 2014-9.
- Suzuki T, Mehta RH, Ince H, et al. Clinical profiles and outcomes of acute type B aortic dissection in the current era: lessons from the International Registry of Aortic Dissection (IRAD). Circulation 2003;108 Suppl 1:II312-7. [PubMed]
- Tsai TT, Evangelista A, Nienaber CA, et al. Partial thrombosis of the false lumen in patients with acute type B aortic dissection. N Engl J Med 2007;357:349-59. [PubMed]
- Tsai TT, Schlicht MS, Khanafer K, et al. Tear size and location impacts false lumen pressure in an ex vivo model of chronic type B aortic dissection. J Vasc Surg 2008;47:844-51. [PubMed]
- Trimarchi S, Tolenaar JL, Jonker FH, et al. Importance of false lumen thrombosis in type B aortic dissection prognosis. J Thorac Cardiovasc Surg 2013;145:S208-12. [PubMed]