Incidence, risk factors, outcome and projected future burden of acute aortic dissection
Introduction
Acute aortic dissection has a high mortality rate, despite well-established treatment guidelines (1). Data on risk factors, incidence and outcome of aortic dissection are limited, largely due to a lack of contemporary population-based studies of this condition. Existing hospital-based studies, often from specialist centers or studies of retrospective registry data such as the International Registry of Acute Aortic Dissection (IRAD), may underestimate incidence and case fatality by incomplete inclusion of deaths prior to hospital admission, which might also bias assessment of risk factors and predictors of outcome.
This research highlight outlines the findings of our recent population-based research of acute aortic dissection, which is the first-ever prospective epidemiological study of this condition (2). We studied event rates, incidence, risk factors, early case fatality, and long-term outcome of all acute aortic events occurring in a population of 92,728 in Oxfordshire, UK, during 2002-2012, as part of the Oxford Vascular Study (OXVASC). Using current incidence data and Office of National Statistics (ONS) population projections (3), we went on to predict UK incidence event rates for acute aortic dissection over the next 40 years.
Methods
The OXVASC study population comprises all individuals (10-year average =92,728), irrespective of age, registered with over 100 family physicians in nine general practices in Oxfordshire, UK. In the UK, the vast majority of individuals register with a general practice, which provides their primary health care and holds a lifelong record of all medical consultations, and details of medications, blood pressure (BP) measurements and investigations. All participating practices held accurate age-sex patient registers, and allowed regular searches of their computerized diagnostic coding systems. All practices refer patients to only one secondary care center.
Case ascertainment was by prospective daily searches for acute events and overlapping retrospective searches of hospital and primary care administrative and diagnostic coding data. A study clinician assessed patients as soon as possible after the event. Informed consent was sought where possible, or assent was obtained from a relative. standardized clinical history and cardiovascular examination were recorded. We also recorded the patients’ hospital records and their general practice records details of the clinical event, medication, past medical history, all investigations relevant to their admission and all interventions occurring subsequent to the event.
If a patient died prior to assessment, we obtained eyewitness accounts and reviewed any relevant records. If death occurred outside hospital or prior to investigation, the autopsy result was reviewed. Clinical details were sought from primary care physicians or other clinicians on all deaths of possible vascular etiology. Initial clinical assessments were made by study clinical research fellows alongside the clinical teams. All diagnoses were subsequently reviewed by a vascular surgeon.
All patients with acute vascular events affecting the aorta from the 1st April 2002 to the 31st March 2012 were included. Acute aortic dissection was classified according to the Stanford system into type-A (proximal to left subclavian artery origin) or type-B (distal to left subclavian artery origin). Event rates were defined as the total number of vascular events that led to separate clinical presentations during the study period. All events were categorized as first-ever incident or recurrent and specific to territory. An incident event implied the first ever aortic dissection, irrespective of type. Second events were always recurrent, irrespective of type (i.e., a first type-A event would be classed as recurrent in a patient with only a previous type-B event). An extension of a previous dissection was not considered to be a recurrent event if it occurred within 6 months of the first event.
Statistical analysis
Analyses were done with SPSS (version 21.0; SPSS Inc, Chicago, Ill, USA). Age-specific and sex-specific rates (per 100,000 population per year) were calculated for incidence and mortality. Since all comparisons were within-population, rates were not standardised to any external populations. Numeric data were expressed as means (standard deviation, SD) or proportions, as appropriate. Group differences in continuous variables were examined with Student t test or Mann-Whitney U test for parametric and non-parametric variables, respectively. Group differences in categorical variables were examined with Fisher Exact test or χ2 test, as appropriate. Gender-differences in outcome were assessed for using multivariable binary logistic regression analysis with adjustment for age. Survival rates were derived by Kaplan-Meier analysis.
Current event rates for the whole UK population were projected based on measured OXVASC incidence rates and the 2010 UK census population. Future event rates for the UK population were projected based on current OXVASC incidence rates and the ONS national population projections by age and sex for the UK for 2030 and 2050 (3). No assumptions were made about potential trends in age-specific incidence rates or competing risks in relation to time-trends in other disease rates.
Results
A total of 173 events occurred in 155 patients during the study period. 54 patients had 59 thoraco-abdominal aortic dissections [52 incident events-6/100,000, 95% confidence interval (CI), 4-7] and 101 patients had 114 ruptured/symptomatic aortic aneurysms (101 incident events-11/100,000, 95% CI, 9-13). Of the 52 incident dissections, 37 (71.2%) were Stanford type-A and 15 (28.8%) were type-B.
Table 1 shows the demographics and risk factors for incident acute aortic dissections by gender and by Stanford classification. Mean (SD) age for acute aortic dissection was 72.0 (14.5) years and the male:female ratio was 1.5:1. Women suffered from acute dissections at a significantly higher mean age than men overall (79.3 vs. 67.1 years; P=0.002) and in those cases not associated with Marfan’s (79.3 vs. 69.6 years; P=0.003). Of type-B aortic dissection patients, 53.3% had prior history of stroke compared with only 13.5% of type-A dissections (P=0.005).
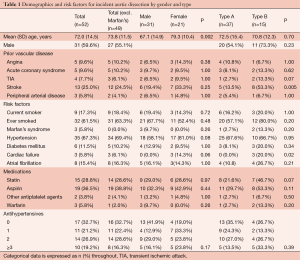
Full table
The most prevalent vascular risk factors were known hypertension (67.3%) and having ever smoked (61.5%). For hypertension, the recorded prevalence increased significantly over the 10-year study period from 42.9% in years 1 to 3 to 85.7% in years 8 to 10 (trend over 10 years, P=0.008), reflecting increased routine screening in primary care. With regards to the study population of 92,728, during years 8 to 10 of the study period, 23,633 subjects were aged ≥55, of which 8,881 (37.6%) had diagnosed hypertension and 11,097 (47.0%) had ever smoked. There were no statistically significant sex differences in risk factors for aortic dissection, although hypertension tended to be more common in women, who were also more likely to be on antihypertensive medication.
Pre-morbid control of BP was poor despite 67.3% of patients being on antihypertensive medication. Over the 5 years prior to the incident dissection, the proportion of all BPs recorded in primary care in individual patients that were greater than 140/90 mmHg averaged 56.0% and was similar for type-A (55.4%) and type-B (57.1%) dissections (P=0.84). Results were similar in analyses of measurements over the 15 years prior to the incident dissection, with an average of 58.3% >140/90 mmHg. Maximum prior recorded SBP was ≥180 mmHg in 46.0% of patients and was similar for men (41.4%) and women (52.4%), but tended to be more common in those suffering type-B dissections (60.0%) compared to type-A (40.0%) (P=0.19). Among those patients who had been started on antihypertensive treatment, 61.9% of subsequent BP readings still exceeded 140/90mmHg despite the majority of patients being on combination therapy (21.2% monotherapy; 26.9% dual, 19.2%≥ triple therapy). In patients with diagnosed hypertension, the proportion of patients on two or more antihypertensive drugs did increase during the study period from 28.6% in years 1 to 3 to 66.7% in years 8 to 10 (trend over 10 years, P=0.02). Pre-morbid BP measurements were available for 50/52 (96.2%) patients with a mean of 24.7 (±19.5) recordings per patient.
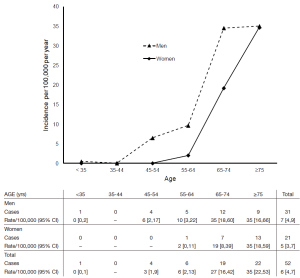
Figure 1 shows numbers and age/sex-specific incidence rates for incident dissection events. Age of onset was approximately 10 years later in women vs. men, but rates were similar at age ≥75 years.
A total of 19 interventional procedures were performed following acute dissection during the study period. Fifteen of 34 patients (44.1%) patients (11 with type-A dissection) underwent emergency surgical treatment; 12 open aortic surgical repairs, 2 endovascular aortic stenting procedures (EVAR), 1 renal artery stenting procedure and 2 open limb procedures (amputations). For patients surviving until hospital discharge (40.7% of total), median length of stay was 11.5 days (interquartile range 6-22.5 days). For incident cases, 80.8% were fully independent [modified Rankin Scale (mRS) 0-2] prior to event [mean mRS 1.5 (1.1 SD)]. For those discharged from hospital alive, mean 30-day mRS was 2.6 (1.0) and mean 6-month mRS was 2.1 (1.3), with 72.7% of these patients independent at 6 months post-event.
Of the 52 patients with incident events, 33 died during the study period. The 30-day and 5-year fatality rates (Figure 2) were 55.8% and 64.5%, but were higher for type-A dissections (73.0% and 76.8% respectively) than for type-B dissections (13.3% and 33.3% respectively). The incident dissection was immediately fatal in 18 cases (13 were certified as dead at home and 5 were dead on arrival at hospital), all with type-A dissections. In patients with incident type-A dissections who survived to hospital admission, 30-day mortality was 47.4%. Among those who survived to hospital discharge, subsequent 5-year survival rates were high (85.7% for type-A; 83.3% for type-B). After adjustment for age, immediate death, 30-day, and 5-year mortality rates were higher in women vs. men (adjusted OR: 6.4, 95% CI, 1.5-26.5, P=0.01 and 3.6, 0.95-13.6, P=0.06; and adjusted HR: 2.0, 0.95-4.3, P=0.07 respectively). During the 5 years prior to the event, BP control was poorer in patients with type-A dissections that were immediately fatal than in those cases who survived to admission: mean (SD) pre-event SBP =151.2 (19.3) vs. 137.9 (17.9); P<0.001.

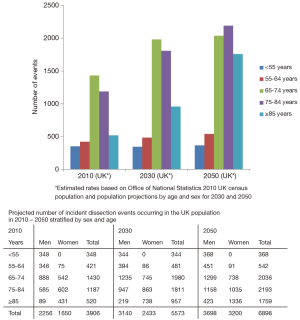
Based on current incidence rates and projected evolution of age/sex population structure, annual incident events in the UK will increase from 3,892 in 2010 to as many as 6,893 in 2050 (Figure 3). Projections also show that over the next 40 years the number of events in the over-85 age group may more than triple, with over 50% of events likely to occur in patients of age ≥75 years, and that the sex distribution will shift, with more type-A dissection events occurring in women than in men, and an equal sex-ratio to be expected overall.
Discussion
Previous studies of aortic dissection have been hospital-based, restricted by age or vascular territory, and have had incomplete ascertainment due to exclusion of out-of-hospital cases. Previous epidemiological studies of aortic dissection also predated widespread use of modern diagnostic technology such as CT angiography, and so diagnostic accuracy was potentially questionable. Of the two studies of the epidemiology of aortic dissection commenced since 1980 (4,5), both were retrospective and used only routinely collected diagnostic or mortality coding data to ascertain subjects and neither assessed pre-morbid risk factors or functional outcome. Our study is the first prospective population-based study with comprehensive case-ascertainment and high levels of patient participation (6).
We have reported four main findings. First, the incidence of acute dissection in our study was higher than previously estimated, probably due to more complete inclusion of deaths prior to hospital admission. It is also possible that improvements in vascular imaging might have contributed and that the incidence of acute dissection may have increased since previous studies. Second, we showed that the incidence of acute aortic dissection is now approximately half that of ruptured/symptomatic aortic aneurysms and therefore represents a significant clinical burden. Third, we showed that hospital-based databases, such as the IRAD which include only patients who reach designated tertiary referral centers alive, will miss a substantial proportion (~50%) of patients with acute type-A dissections who die at home or before hospital admission, thereby underestimating overall disease incidence and both short- and long-term case fatality. This selection bias is also likely to account for the lower in-hospital mortality rates found in IRAD compared to other studies where a significant transfer time to a specialist center is not required.
Finally, although patients with dissections had low rates of prior vascular disease, including ischaemic heart disease, diabetes, and peripheral arterial disease, we confirmed previous observations that hypertension is very strongly associated with aortic dissection. Moreover, in the first detailed analysis of pre-morbid BP control in patients presenting with acute dissection, we showed that prior control of BP was poor, despite the majority of patients being on combination antihypertensive therapy, particularly in immediately fatal cases. This high rate of treatment-resistant hypertension may reflect increased aortic stiffness or other pathophysiological mechanisms responsible for the development of acute aortic syndromes. However, better control of BP would nevertheless be likely to reduce incidence and case fatality. Trials of BP-lowering drugs should include aortic dissection in composite outcomes intended to determine the overall impact of treatment.
Our findings also have implications for future clinical service provision. Over the next 40 years the UK population aged 75 or above will double (from 8% to 15%). Our data suggest that over 50% of incident dissection events will occur at age >75 years by 2050 and that the total number of incident events each year may almost double if pre-morbid risk factors are not better controlled. Improved primary prevention, in particular more aggressive management of hypertension and smoking cessation, may reduce future incidence rates, but treatment-resistant hypertension is likely to remain a challenge.
Although we consider our findings to be valid, our study has some potential shortcomings. First, the OXVASC population is 94% white and the proportions of other racial groups are too small (3.1% Asian, 1.5% Chinese and 1.4% Afro-Caribbean) to determine separate event rates and outcomes. However, the proportion of whites is similar in the UK as a whole (88% white) and in many other western countries (Australia 90%; France 91%; Germany 93.9%), although our results will not necessarily apply in the United States (72.4% White, 12.6% African American, 4.8% Asian, 0.9% American Indian, 6.2% Chinese/Other). However, there are few differences in the demographics and outcome of aortic dissections between the IRAD centers in Europe (99% white) and those in North America (91% white). Second, our projections of the likely numbers of future incident aortic dissections in the UK were simplistic, particularly our assumption that current age/sex-specific incidence rates will remain constant. However, in the absence of any reliable data on past trends in incidence of dissections in the UK, this assumption was necessary. Rather than introduce more assumptions about possible future trends in incidence rates (which are unknown), we projected current rates (which are at least known). It is quite possible therefore that our projections will be overestimates.
In conclusion, in the first ever prospective population-based study of acute aortic disease, we have shown that incidence of acute aortic dissection is higher than previous estimates, and have demonstrated the importance of inclusion of out-of-hospital deaths if incidence and outcome are to be reliably determined. We have also identified the critical association between acute aortic dissection and hypertension, particularly hypertension resistant to medication. Ageing of populations and demographic changes indicate future increased rates of disease over the next few decades, with implications for health service provision and future research, especially since surgical outcome has not improved substantially in the recent past despite significant progress in diagnosis and endovascular treatment.
Acknowledgements
We are grateful to all the staff in the general practices that collaborated in OXVASC: Abingdon Surgery, Stert St, Abingdon; Malthouse Surgery, Abingdon; Marcham Road Family Health Centre, Abingdon; The Health Centre, Berinsfield; Kidlington Health Centre; Kidlington; Yarnton Health centre, Kidlington; 19 Beaumont St, Oxford; East Oxford Health Centre, Oxford; Church Street Practice, Wantage.
Funding: The Oxford Vascular Study is funded by the Wellcome Trust, UK Medical Research Council, the Dunhill Medical Trust, the Stroke Association, the National Institute for Health Research (NIHR), the Thames Valley Primary Care Research Partnership, and the NIHR Biomedical Research Centre, Oxford. DPJH is funded by the NIHR Biomedical Research Centre, Oxford. PMR has a Wellcome Trust Senior Investigator Award and an NIHR Senior Investigator Award.
Ethics: The Oxford Vascular Study has been approved by our local research ethics committee.
Disclosure: The authors declare no conflict of interest.
References
- Golledge J, Eagle KA. Acute aortic dissection. Lancet 2008;372:55-66. [PubMed]
- Howard DP, Banerjee A, Fairhead JF, et al. Population-based study of incidence and outcome of acute aortic dissection and premorbid risk factor control: 10-year results from the oxford vascular study. Circulation 2013;127:2031-7. [PubMed]
- Office for National Statistics. National Population Projections. National population projections by age and sex for the UK and constituent countries. Available online: http://www.statistics.gov.uk/hub/population/index.html
- Olsson C, Thelin S, Ståhle E, et al. Thoracic aortic aneurysm and dissection: increasing prevalence and improved outcomes reported in a nationwide population-based study of more than 14,000 cases from 1987 to 2002. Circulation 2006;114:2611-8. [PubMed]
- Clouse WD, Hallett JW Jr, Schaff HV, et al. Acute aortic dissection: population-based incidence compared with degenerative aortic aneurysm rupture. Mayo Clin Proc 2004;79:176-80. [PubMed]
- Rothwell PM, Coull AJ, Silver LE, et al. Population-based study of event-rate, incidence, case fatality, and mortality for all acute vascular events in all arterial territories (Oxford Vascular Study). Lancet 2005;366:1773-83. [PubMed]





