Possible graft-related complications in visceral debranching for hybrid B dissection repair
Abstract
Background: Hybrid repair (HR) of thoracoabdominal aortic aneurysm (TAAA) and dissection (TAAD), consisting of rerouting renovisceral branches followed by endograft aortic repair, has been shown to be a feasible option. It is especially appealing in patients unfit for both open and total endovascular repair. In order to determine the role of dissecting etiology and intraoperative variables as risk factors for graft-related complications in visceral debranching, we retrospectively analyzed the clinical outcomes, patency rate and hemodynamic alterations of the renovisceral debranching grafts in our series.
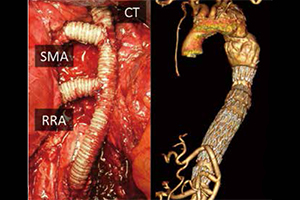
Methods: We analyzed 55 consecutive patients who underwent thoracoabdominal aortic HR between 2001 and 2013 in our center. Forty-four procedures were performed for TAAA and 11 procedures for TAAD. In TAAD patients, dissection involved 9/44 (20.5%) renovisceral vessels. One hundred and fifty-nine visceral bypasses were made (156 retrograde; three anterograde).
Results: Thirty-day mortality was 12.7% (n=7). Potential graft-related complications included four cases of pancreatitis (7.3%) and five of peri-operative renal failure (9.1%). At a mean follow-up of 36.1 months, the global rate of visceral graft occlusion was 9.4% (15/159), leading to fatal bowel infarction in two patients and kidney loss in seven patients. Actuarial primary patency in renovisceral grafts at 12, 24, and 36 months was 96.3%, 92.6%, and 90.2% respectively. At the level of the anastomosis of the graft to the superior mesenteric artery, significant flow alterations (systolic peak velocity >250 cm/s) were observed during computed flow dynamics analysis in 18.5% of cases. Overall, an additional procedure to ensure patency was required in 19 bypasses intraoperatively and three during follow-up. The presence of aortic dissection had no significant impact on debranching graft-related complications. During multivariate analysis, retropancreatic routing to CT was the only independent predictor of graft-related complications (P=0.006).
Conclusions: Specific visceral graft-related complications were not uncommon in our series and were often associated with clinical consequences. Hemodynamic alterations of debranching grafts were observed in particular at the level of the anastomosis with the superior mesenteric artery. Careful follow-up is mandatory in order to monitor visceral bypasses and facilitate patency when required.
Cover