Best surgical option for arch extension of type B aortic dissection: the open approach
Introduction
Arch extension of the aortic dissection (AD) is reported in 4-25% of patients with acute Stanford type B AD (1-4). The prognosis of this subtype of AD has been studied by several groups, however, there have been few discussions regarding the management of this particular cohort. For instance, the current practice guidelines on the treatment of aortic diseases lack statements on this specific clinical presentation (5). This perspective article will discuss the literature surrounding arch extension of acute type B AD as well as its optimal treatment options.
Definition
The two most widely accepted classification systems for AD, the DeBakey and Stanford classifications, are very useful in the characterization of the anatomy of lesions and to assist in determining the initial management strategies in most patients with acute AD. Both classifications, however, face fundamental limitations when the AD involves aortic arch but spares the ascending aorta. The DeBakey classification, based on the anatomical location of the primary intimal tear and the extent of the dissection, does not include a category with “an intimal tear in the aortic arch” (6). The Stanford classification, a more straightforward “how-to-treat” based classification, considers the presence of false lumen in the ascending aorta as the only criterion to differentiate the type A from type B AD (7). However, there is no specification available to assess the prognosis of AD extending to (or originating from) the arch but without involvement of the ascending aorta.
Some efforts have been made to accommodate classifications of AD in other locations and extents. However, they have failed to receive general acceptance due to their complex nomenclatures as well limited relevance in relation to treatment and outcomes (2,8). Currently, it is regarded as reasonable to refer to this condition simply as “type B with arch involvement” regardless of the location of intimal tear (arch vs. descending aorta) because this designation may best describe the nature, prognosis and optimal treatment option of the disease. The rationale of this idea will be described in the following two sections.
Incidence
The occurrence of arch involvement of type B AD has been reported to range from 4% to 74.2% (1-4,9), but apart from the extraordinarily high rate of 74.2% reported by a single study (3), it is most frequently reported to occur in less than 25% of patients. The discrepancy in its reported rate is most likely attributable to heterogeneous definitions. In fact, some define “arch extension” only when the intimal tear is identified in the arch, whereas others define it only by the presence of flap in the arch, regardless of the location of tears. Retrograde extension of the type B AD into the ascending aorta is also not an uncommon clinical scenario, although the exact probability of this happening among all cases of acute type B AD is uncertain because most investigations dealing with this unique clinical picture have defined these patients as acute type A (10-13).
If the AD extends in a retrograde fashion beyond the arch and to ascending aorta, the prognosis of these patients is well known to be very similar to those with acute type A AD, therefore mandating emergent surgery (5,8,14). The only exceptions may be highly selected, clinically stable patients who have a completely thrombosed false lumen in the ascending aorta with an acceptably small sized ascending aortic diameter. Several studies have shown acceptable clinical outcomes with medical therapy combined with timely surgery in these selected patients, and consequently, debates over how to treat these patients are now underway (10). This clinical setting is quite different from those who have AD extension limited to the arch, and therefore is beyond the scope of the present review. The issue regarding “retrograde extension of type B AD to ascending aorta” will be reserved to be addressed elsewhere.
Prognosis
In a study by Erbel et al., retrograde extension of type III AD was associated with poorer survival as well as increased adverse clinical events (8). Of note, the study did not separate arch extension from a more extensive form of ascending aorta involvement; therefore, the clinical outcomes of patients with arch extension in comparison to those without could not be elucidated. In a more recent study, Tsai and colleagues sought to evaluate the impact of arch extension on the outcomes through analyses of the International Registry of Acute Aortic Dissection (IRAD) database (9). Among 498 patients with acute type B AD, 25.5% of patients (n=127) had arch extension, and of this group, 37.7% were found to have intimal tear in the arch. Treatment modalities (medical, surgical or endovascular) did not differ according to the presence of arch extension, in that over 70% of patients in both groups received only medical therapy (P=0.97). Short-and long-term mortality rates were almost identical regardless of involvement of the arch (P=0.61 and 0.82, respectively). Even after adjusting for demographic profiles, comorbidities and treatment, arch extension did not affect survival (hazard ratios, 1.0; P=0.96). Several other studies, such as that by Tsai and colleagues from IRAD, have similarly shown that arch involvement did not translate to more frequent requirements for surgical intervention or increased mortality (1,3,4).
These findings strongly support the notion that the prognosis of patients with arch extension in acute type B AD is virtually identical to overall type B AD regardless of the location of intimal tear, and the treatment principle should therefore be similar to those with type B AD. In this sense, it seems reasonable to classify patients with such arch extension as “Stanford type B AD”.
Management
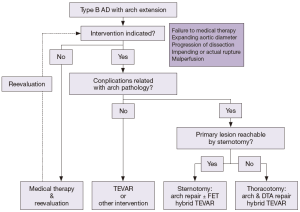
As discussed, it seems reasonable in patients presenting with acute type B AD and arch extension to follow the management guidelines for classic acute B AD, if the ascending aorta is not affected by the disease. Specifically, uncomplicated AD should be managed with medical therapy, while complicated cases are best managed by thoracic endovascular aortic repair (TEVAR). Conventional surgical therapy is reserved only for complicated cases where TEVAR approaches are not feasible based on the reported high risk of mortality in patients receiving surgical therapy in the setting of acute type B AD, even in recent series (5,14,15).
The well-established indications for surgical or interventional operation in acute type B AD are as follows: (I) failure of medical therapy (uncontrolled pain or hypertension); (II) expanding aortic diameter; (III) progression of dissection; (IV) impending or actual rupture; and (V) malperfusion syndrome (5). According to a report from IRAD, in patients who had arch involvement in acute type B AD, 15% required surgery and 13.4% required endovascular therapy. These figures were virtually identical to those without arch extension.
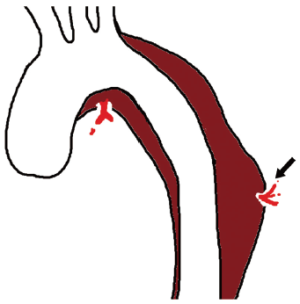
Complicated cases of acute type B AD with arch extension do not necessarily mean that the complications are directly related with the arch involvement. A study by Estrera et al. [2006] showed that only 9.5% of patients receiving surgical or endovascular therapies for complicated type B AD with arch extension underwent treatment specifically targeting the aortic arch (all conventional arch replacement surgery) while the remaining 90.5% of patients received interventions to treat the descending thoracic aorta or further downstream aorto-vascular segments (1). This figure indicates that less than 2% of all cases of acute type B AD and around 10% patients with arch extension require surgical therapy for complication related to arch involvement. In this regard, most of the complicated type B AD with arch extension will require intervention to treat the aorta distal to the arch, suggesting that TEVAR approaches are likely to be the best treatment option in most cases. Surgery on the aortic arch is performed only in few patients whose complications are directly related to the disease in the arch as shown in Figure 1. The treatment algorithm for patients with acute type B AD with arch involvement is suggested in Figure 2. Additional surgery or interventions to treat visceral/renal and limbs ischemia may be required according to the presence of such combined complications.

Surgical approach
Once surgical arch repair is indicated, one should note that the purpose of surgery at this stage is to treat fatal complications of the arch, but not to replace the whole aorta affected by AD. Exceptions to this may include patients with Marfan syndrome, in who aortic root repair concomitantly with total arch replacement may be a more reasonable option to prevent redo-sternotomy and thereby improve long-term outcomes (16).
The most important consideration to determine the surgical approach is accessibility of the proximal and distal extent of the disease. Generally, the level of tracheal carina is used as a fair anatomical landmark of distal end of anastomosis when the total arch replacement through sternotomy is planned. If the distal end of the target lesion is located proximal to this level, arch repair through sternotomy approach seems the most reasonable approach (Figure 2).
A thoracotomy approach provides better exposure for the repair of distal arch and downstream descending aorta, nevertheless, the presence of acute dissection flap in the arch hinders the clamping around this region, making circulatory arrest unavoidable for surgery. The challenges of providing selective cerebral perfusion and comprehensive myocardial protection during the procedure as well as the extensive nature of the exposure are among the most significant weaknesses of the thoracotomy approach. The high risks of operative mortality and morbidity of this approach in the treatment of acute type B AD have been well recognized throughout the history of aortic surgery, as well as in the current era (4,14,17-19). Therefore, it seems reasonable to save this approach as a last resort for patients meeting both of following conditions: (I) Distal locations of target lesion (multiple lesions or arch lesion extending too far distally) where sternotomy alone cannot allow approach to these lesions (Figure 3) and (II) TEVAR is not feasible, including cases where concomitant sternotomy and TEVAR approaches are not available (Figure 2). Candidates for this approach are most likely cases where AD develops on preexisting complex thoracoabdominal aneurysms. Expected surgical mortality is very high, and therefore, the decision on whether to plan this surgery should be made very judiciously considering the balance between the risks and benefits.
Total arch replacement is the standard surgical option in most cases because of the location of the target pathology. The use of adjunctive cerebral perfusion techniques is reasonable in extensive arch surgeries as demonstrated by a recent German Registry [2011] study showing the improved survival and neurologic outcomes by the use of such methods in AD surgery requiring prolonged (>30 min) circulatory arrest (20). A more limited approach of performing exclusive hemi-arch replacement with distal beveling may be feasible in very selected cases if the target lesion is confined within the lesser curvature of the arch, however, candidates for this approach will be much fewer than those with acute type A dissections. Furthermore, it is still controversial whether such an approach will decrease the operative risks in patients with acute AD (11,12,21-24).
Stent-graft insertion in the descending aorta concomitant with total arch replacement, the so-called frozen elephant trunk technique, is another option in the surgical management of a complicated arch in type B AD. The more frequent distal location of intimal tear, rather than those confined to the arch, favors the frozen elephant technique as an option to cover these lesions, which are often unapproachable by conventional surgery through sternotomy. While this new surgical method has been evaluated mostly in the setting of acute type A AD (22,23,25,26), a very recent multi-center study by Weiss and his colleagues evaluated its outcomes in the very specific setting of complicated type B AD with involvement of the aortic arch where TEVAR was not amendable (27). In the cited study, 16 out of 57 subjects (28.1%) had acute type B AD. In this cohort, in-hospital mortality and stroke occurred in 12% and 12% of patients, respectively, while no patients experienced spinal cord injury. In the late period, complete thrombosis of the false lumen was observed in 100% in the arch, 75% in the distal descending aorta and 33% in the abdominal aorta. At 3 years, survival and freedom from secondary aortic reintervention rates were 75% and 79%, respectively, showing no significant differences between acute and chronic AD. These findings indicate that the frozen elephant trunk approach combined with total arch repair is a promising surgical approach for treating complicated aortic arch in acute type B AD.
Hybrid arch repair
Arch vessel debranching combined with stent-grafting in the aortic arch, defined as “hybrid arch repair”, has emerged as a new alternative approach in the treatment of aortic aneurysm, and is associated with acceptable mid-term outcomes (28). Indeed, it is an appealing treatment modality as it minimizes the invasiveness of treatment for patients with complicated type B AD, thus supporting the effort to reduce the treatment-related morbidity and mortality. Several studies have shown the early results of such an approach to treat complicated type B AD with arch extension, including series with acute AD (29-32) (Table 1). If confined to the distal part of the arch (Zone 1-3), the dissection can be treated in a less invasive way via small neck incisions and even under local anesthesia (30). Therefore, it seems reasonable to undertake this hybrid approach when the arch involvement is confined in the distal area rather than conventional arch replacement surgery.
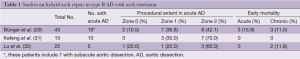
Full table
In a recent study, Bünger and his colleagues evaluated the outcomes of hybrid approach in 45 patients with type B AD with arch extension, and identified the Zone 0 procedure (vs. Zone 1 or 2) and emergency operation as significant risk factors for periprocedural mortality (29). Of note, both of the two patients who underwent Zone 0 hybrid procedure in the setting of acute AD died postoperatively. Therefore, the safety and efficacy of this procedure in cases with more extensive arch involvement needs to be assessed in further studies in comparison with other treatment modalities. Furthermore, stent-related complications in the long-term are now becoming a more and more important clinical issue in the TEVAR era. In this sense, there is a need for further investigations to test the validity of the hybrid approach in acute type B AD with arch extension, where greater anatomical complexity is encountered for TEVAR than in the treatment of descending thoracic aortic segments.
Conclusions
Arch extension of AD is not an uncommon clinical scenario in acute type B AD. The prognosis as well as management guidelines of acute type B AD will also most likely apply to this particular set of patients. Arch repair surgery should be reserved for those with complicated arch caused by the AD, and total arch replacement combined with FET through sternotomy seems to be the most reasonable approach to treat these complications in many cases. Extensive arch and DTA repair via thoracotomy should be reserved as a last option only for the few patients whose anatomy of target lesions is not manageable through sternotomy or TEVAR because of high operative risks.
Acknowledgements
This work was supported by the “American Association for Thoracic Surgery’s Evarts A. Graham Memorial Traveling Fellowship.”
Disclosure: The authors declare no conflict of interest.
References
- Estrera AL, Miller CC 3rd, Safi HJ, et al. Outcomes of medical management of acute type B aortic dissection. Circulation 2006;114:I384-9. [PubMed]
- Lansman SL, McCullough JN, Nguyen KH, et al. Subtypes of acute aortic dissection. Ann Thorac Surg 1999;67:1975-8; discussion 1979-80.
- Sueyoshi E, Sakamoto I, Hayashi K, et al. Growth rate of aortic diameter in patients with type B aortic dissection during the chronic phase. Circulation 2004;110:II256-61. [PubMed]
- Umaña JP, Lai DT, Mitchell RS, et al. Is medical therapy still the optimal treatment strategy for patients with acute type B aortic dissections? J Thorac Cardiovasc Surg 2002;124:896-910. [PubMed]
- Hiratzka LF, Bakris GL, Beckman JA, et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease: executive summary. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. Catheter Cardiovasc Interv 2010;76:E43-86. [PubMed]
- Debakey ME, Henly WS, Cooley DA, et al. Surgical management of dissecting aneurysms of the aorta. J Thorac Cardiovasc Surg 1965;49:130-49. [PubMed]
- Daily PO, Trueblood HW, Stinson EB, et al. Management of acute aortic dissections. Ann Thorac Surg 1970;10:237-47. [PubMed]
- Erbel R, Oelert H, Meyer J, et al. Effect of medical and surgical therapy on aortic dissection evaluated by transesophageal echocardiography. Implications for prognosis and therapy. The European Cooperative Study Group on Echocardiography. Circulation 1993;87:1604-15. [PubMed]
- Tsai TT, Isselbacher EM, Trimarchi S, et al. Acute type B aortic dissection: does aortic arch involvement affect management and outcomes? Insights from the International Registry of Acute Aortic Dissection (IRAD). Circulation 2007;116:I150-6. [PubMed]
- Kaji S, Akasaka T, Katayama M, et al. Prognosis of retrograde dissection from the descending to the ascending aorta. Circulation 2003;108 Suppl 1:II300-6. [PubMed]
- Kazui T, Tamiya Y, Tanaka T, et al. Extended aortic replacement for acute type A dissection with the tear in the descending aorta. J Thorac Cardiovasc Surg 1996;112:973-8. [PubMed]
- Kim JB, Chung CH, Moon DH, et al. Total arch repair versus hemiarch repair in the management of acute DeBakey type I aortic dissection. Eur J Cardiothorac Surg 2011;40:881-7. [PubMed]
- Lansman SL, Raissi S, Ergin MA, et al. Urgent operation for acute transverse aortic arch dissection. J Thorac Cardiovasc Surg 1989;97:334-41. [PubMed]
- Booher AM, Isselbacher EM, Nienaber CA, et al. The IRAD classification system for characterizing survival after aortic dissection. Am J Med 2013;126:730.e19-24.
- Fattori R, Tsai TT, Myrmel T, et al. Complicated acute type B dissection: is surgery still the best option?: a report from the International Registry of Acute Aortic Dissection. JACC Cardiovasc Interv 2008;1:395-402. [PubMed]
- Rylski B, Bavaria JE, Beyersdorf F, et al. Type A aortic dissection in Marfan syndrome: extent of initial surgery determines long-term outcome. Circulation 2014;129:1381-6. [PubMed]
- Jex RK, Schaff HV, Piehler JM, et al. Early and late results following repair of dissections of the descending thoracic aorta. J Vasc Surg 1986;3:226-37. [PubMed]
- Neya K, Omoto R, Kyo S, et al. Outcome of Stanford type B acute aortic dissection. Circulation 1992;86:II1-7. [PubMed]
- Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA 2000;283:897-903. [PubMed]
- Krüger T, Weigang E, Hoffmann I, et al. Cerebral protection during surgery for acute aortic dissection type A: results of the German Registry for Acute Aortic Dissection Type A (GERAADA). Circulation 2011;124:434-43. [PubMed]
- Easo J, Weigang E, Hölzl PP, et al. Influence of operative strategy for the aortic arch in DeBakey type I aortic dissection: analysis of the German Registry for Acute Aortic Dissection Type A. J Thorac Cardiovasc Surg 2012;144:617-23. [PubMed]
- Sun LZ, Qi RD, Chang Q, et al. Surgery for acute type A dissection using total arch replacement combined with stented elephant trunk implantation: experience with 107 patients. J Thorac Cardiovasc Surg 2009;138:1358-62. [PubMed]
- Uchida N, Shibamura H, Katayama A, et al. Operative strategy for acute type a aortic dissection: ascending aortic or hemiarch versus total arch replacement with frozen elephant trunk. Ann Thorac Surg 2009;87:773-7. [PubMed]
- Westaby S, Saito S, Katsumata T. Acute type A dissection: conservative methods provide consistently low mortality. Ann Thorac Surg 2002;73:707-13. [PubMed]
- Sun LZ, Qi RD, Chang Q, et al. Is total arch replacement combined with stented elephant trunk implantation justified for patients with chronic Stanford type A aortic dissection? J Thorac Cardiovasc Surg 2009;138:892-6. [PubMed]
- Shrestha M, Fleissner F, Ius F, et al. Total aortic arch replacement with frozen elephant trunk in acute type A aortic dissections: are we pushing the limits too far?†. Eur J Cardiothorac Surg 2014. [Epub ahead of print]. [PubMed]
- Weiss G, Tsagakis K, Jakob H, et al. The frozen elephant trunk technique for the treatment of complicated type B aortic dissection with involvement of the aortic arch: multicentre early experience. Eur J Cardiothorac Surg 2014. [Epub ahead of print].[PubMed]
- Bavaria J, Vallabhajosyula P, Moeller P, et al. Hybrid approaches in the treatment of aortic arch aneurysms: postoperative and midterm outcomes. J Thorac Cardiovasc Surg 2013;145:S85-90. [PubMed]
- Bünger CM, Kische S, Liebold A, et al. Hybrid aortic arch repair for complicated type B aortic dissection. J Vasc Surg 2013;58:1490-6. [PubMed]
- Iannelli G, Monaco M, Di Tommaso L, et al. Complicated acute type B aortic dissection involving the arch: treatment by simultaneous hybrid approach under local anesthesia. J Thorac Cardiovasc Surg 2008;135:1380-2. [PubMed]
- Kefeng Z, Xudong P, Yongmin L, et al. Hybrid operation for type B aortic dissection involving distal aortic arch. J Card Surg 2014;29:359-63. [PubMed]
- Lu Q, Jing Z, Zhao Z, et al. Endovascular stent graft repair of aortic dissection type B extending to the aortic arch. Eur J Vasc Endovasc Surg 2011;42:456-63. [PubMed]





