Long term outcomes of posterior leaflet folding valvuloplasty for mitral valve regurgitation
Introduction
Posterior mitral valve leaflet prolapse due to degenerative mitral valve disease is the most common cause of mitral valve regurgitation (1). Over 90% of these patients undergo successful mitral valve repair (MVR) (2). The most common classic repair consists of triangular or quadrangular resection of prolapsed segment with sliding valvuloplasty of remaining posterior leaflet (3,4). Over the years, tissue sparing repair techniques of the posterior leaflet were introduced by Calafiore et al. and Mihaljevic et al. for patients whose anatomy of posterior leaflet prevented optimal result from being achieved with resection techniques (5,6). Popularization of the foldoplasty technique for posterior leaflet prolapse was done by Tabata et al. who simplified the technique and expanded the indications (7). This technique effectively lowers the height of the redundant posterior leaflet and creates an optimal coaptation line for the anterior leaflet. Midterm results of this technique showed excellent durability and freedom from reoperation as well as excellent return of functional status (8).
We report mid to long term outcomes, including ECHO follow-up, of this simplified technique for posterior leaflet repair.
Technique
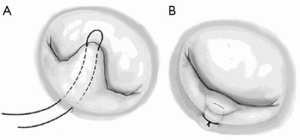
Patients were positioned and monitoring lines were placed in a regular fashion. Procedures were performed through full sternotomy (FS) or minimally invasive lower hemisternotomy (LHS). Aorta was directly cannulated in both approaches while venous cannulation was direct bicaval for FS and percutaneous femoral for minimally invasive approach. Cardiopulmonary bypass (CPB) was initiated and myocardial protection was accomplished with intermittent cold blood cardioplegia given down the aortic root. Sondergaard’s groove was opened and left atriotomy was performed exposing the mitral valve. The mitral valve was then inspected in detail and the prolapsed area was identified. Depending on the width of the prolapsed area, one to six double-armed 4-0 polypropylene sutures were placed from the leaflet edge to the annulus of the posterior leaflet (Figure 1A). These sutures were subsequently tied at the mitral annulus, thereby folding over the redundant leaflet to reduce the effective height of the leaflet by at least 50% (Figure 1B). We were able to adjust the leaflet height by changing the entry or exit points of the sutures. A flexible annuloplasty ring was subsequently inserted with 2-0 braided polyester mattress sutures in all patients. The size of the ring was based on the surface area of the anterior leaflet. An LV competency test was then done to confirm that the valve had been adequately repaired. Upon the completion of mitral repair, the left atrium was closed with 4-0 prolene suture. The patient’s heart was deaired and the patient was weaned from CPB in the standard manner. Transesophageal echocardiography (TEE) confirmed adequate MVR.
Methods
With the approval of the Brigham and Women’s Hospital Institutional Review Board, we conducted a retrospective review of all patients with myxomatous disease undergoing MVR of the posterior leaflet using the foldoplasty technique between January 2002 and May 2014. Patients with less than moderate mitral regurgitation (MR) and those who had concomitant valvular resection were excluded; 229 patients met study criteria. Patient demographics and in-hospital outcome data were extracted from electronic medical records. Long-term follow-up of the 161 patients previously reported (8) was obtained from routine clinical follow-up and/or from the cardiologist of record. Survival data was obtained by additional query of the Social Security Death Index and from our State Department of Health. Primary outcomes of interest included repair durability, recurrence of clinically significant MR, and survival. See supplementary Video 1 for footage of the procedure.
Statistical analysis
Binary variables are presented as percent and number (n); long-term follow up was compared to baseline using McNemar’s test for repeated measures. Continuous variables are presented as mean ± standard deviation (SD); follow-up data was compared to baseline using repeated measures t-test. Kaplan-Meier analyses were used to evaluate long-term outcomes; follow-up time was calculated in months between the date of surgery and the date of the first of (I) follow-up echo showing clinically significant MR (defined as greater than moderate MR); (II) failure of the foldoplasty requiring reoperation; (III) death; (IV) date of last clinical follow-up documented. Study observation ended on July 31, 2014. All analyses were conducted using SPSS version 13.0 (SPSS Inc., Chicago, IL, USA) and P≤0.05 was the criterion for significance.
Results
Between January 2002 and May 2014, a total of 2,193 patients underwent MVR involving the posterior leaflet for myxomatous disease. Foldoplasty was performed on 229 (10.4%) of these patients, their mean age was 60.6±13.7 years, and 105 (45.9%) were females. Clinical variables are presented in Table 1. Hypercholesterolemia was present in 147 (64.1%) foldoplasty patients, and 100 (43.7%) patients were hypertensive. Other comorbidities included diabetes (9/229; 3.9%), peripheral vascular disease (11/229; 4.8%), and previous cardiac surgery (3/229; 1.3%). Of the total cohort, 51 (22.3%) were in New York Heart Association (NYHA) class III/IV. Preoperative echocardiographic readings showed a mean PA pressure of 24±10 mmHg and severe MR in 163 (71.2%) of the patients and moderate to severe in the remainder. Concomitant coronary artery bypass graft surgery (CABG) was performed on 32 (14%) patients and the mean perfusion time was 119±40 min and the mean cross clamp time was 86±31 min. Post-operative mortality was 2/229 (0.9%), reoperation for bleeding occurred in 4/229 (1.7%) and postoperative stroke in 4/229 (1.7%).

Full table
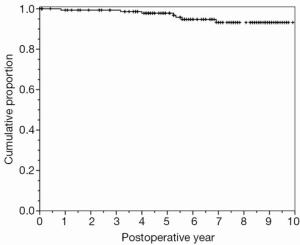
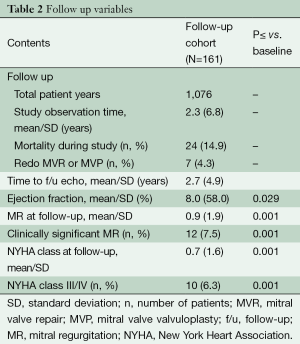
Long term follow-up was 100% and the study’s mean observation time was 6.8±2.3 years during which overall mortality was 24 (14.9%), and mitral valve reintervention was performed on seven patients (4.3%; Figure 2, Table 2). NYHA class III/IV and clinically significant MR at follow-up were significantly lower compared to preoperative values (both P<0.001).
Full table
Discussion
MVR and its traditional techniques described by Carpentier (1) more than three decades ago, has become well established therapy for degenerative mitral valve disease with excellent durability (9,10). Multiple studies have demonstrated important benefits of MVR over replacement (11,12). In the centers of excellence, repair rates for the isolated posterior leaflet prolapse are over 95% (2,3,13,14). However the number of MVR procedures and repair rates in smaller centers is not as high. Reasons for this may be due to the complexity of the techniques and irreversibility of the attempted repairs that, in case of suboptimal result, end with mitral valve replacement and decreased long-term survival.
Foldoplasty introduced by Calafiore et al., Mihaljevic et al. and Tabata et al., has been part of our toolbox for MVRs since 2002 (5-7). Due to its appealing qualities, namely technical simplicity, broad applicability and reversibility, it has quickly become one of the favored procedures for posterior mitral leaflet prolapse. As described by Cevasco et al. (8) this technique yields excellent perioperative and mid-term results with 100% repair rate for isolated posterior leaflet prolapse and only two patients requiring reoperative procedure on mid-term follow up of 3 years.
We describe our results and long-term follow-up of 229 patients who underwent mitral valve foldoplasty. Follow-up in this series was 100% complete and consisted of 1,076 patient/years. In our cohort only 4.3% of the patients required reoperative surgery over a mean period of 6.8 years and 2% had moderate regurgitation on the follow-up echocardiography that was treated conservatively.
Gillinov et al. reported the Cleveland Clinic experience of 1,072 patients with 10 years freedom from reoperation of 93% (9). In their conclusion, repair durability was greatest in patients with quadrangular resections and annuloplasty. Braunberger et al., in their paper from 2001, report on 162 patients with non-rheumatic MR with 74% freedom from cardiac events at 20 years (15) while Flameng et al. report 94% freedom from reoperation but only 71% freedom from significant MR at seven years for degenerative mitral valve disease (16).
Similar results observed with the foldoplasty, as well as reproducibility and forgiveness due to tissue sparing repairs, encourage further use of this technique in patients with isolated posterior leaflet prolapse.
Limitations of this study include its retrospective observational nature and the lack of a control group. Further randomized studies that compare foldoplasty with other types of posterior mitral leaflet repair may be needed to further validate our results for this technique.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Carpentier A. Cardiac valve surgery--the "French correction". J Thorac Cardiovasc Surg 1983;86:323-37. [PubMed]
- Seeburger J, Borger MA, Doll N, et al. Comparison of outcomes of minimally invasive mitral valve surgery for posterior, anterior and bileaflet prolapse. Eur J Cardiothorac Surg 2009;36:532-8. [PubMed]
- DiBardino DJ, ElBardissi AW, McClure RS, et al. Four decades of experience with mitral valve repair: analysis of differential indications, technical evolution, and long-term outcome. J Thorac Cardiovasc Surg 2010;139:76-83; discussion 83-4. [PubMed]
- Carpentier A, Relland J, Deloche A, et al. Conservative management of the prolapsed mitral valve. Ann Thorac Surg 1978;26:294-302. [PubMed]
- Calafiore AM, Di Mauro M, Actis-Dato G, et al. Longitudinal plication of the posterior leaflet in myxomatous disease of the mitral valve. Ann Thorac Surg 2006;81:1909-10. [PubMed]
- Mihaljevic T, Blackstone EH, Lytle BW. Folding valvuloplasty without leaflet resection: simplified method for mitral valve repair. Ann Thorac Surg 2006;82:e46-8. [PubMed]
- Tabata M, Ghanta RK, Shekar PS, et al. Early and midterm outcomes of folding valvuloplasty without leaflet resection for myxomatous mitral valve disease. Ann Thorac Surg 2008;86:1388-90. [PubMed]
- Cevasco M, Myers PO, Elbardissi AW, et al. Foldoplasty: a new and simplified technique for mitral valve repair that produces excellent medium-term outcomes. Ann Thorac Surg 2011;92:1634-7; discussion 1637-8. [PubMed]
- Gillinov AM, Cosgrove DM, Blackstone EH, et al. Durability of mitral valve repair for degenerative disease. J Thorac Cardiovasc Surg 1998;116:734-43. [PubMed]
- Cohn LH, Couper GS, Aranki SF, et al. Long-term results of mitral valve reconstruction for regurgitation of the myxomatous mitral valve. J Thorac Cardiovasc Surg 1994;107:143-50; discussion 150-1. [PubMed]
- Enriquez-Sarano M, Schaff HV, Orszulak TA, et al. Valve repair improves the outcome of surgery for mitral regurgitation. A multivariate analysis. Circulation 1995;91:1022-8. [PubMed]
- Gillinov AM, Blackstone EH, Nowicki ER, et al. Valve repair versus valve replacement for degenerative mitral valve disease. J Thorac Cardiovasc Surg 2008;135:885-93, 893.e1-2.
- David TE, Armstrong S, Sun Z, et al. Late results of mitral valve repair for mitral regurgitation due to degenerative disease. Ann Thorac Surg 1993;56:7-12; discussion 13-4. [PubMed]
- Deloche A, Jebara VA, Relland JY, et al. Valve repair with Carpentier techniques. The second decade. J Thorac Cardiovasc Surg 1990;99:990-1001; discussion 1001-2 [PubMed]
- Braunberger E, Deloche A, Berrebi A, et al. Very long-term results (more than 20 years) of valve repair with carpentier's techniques in nonrheumatic mitral valve insufficiency. Circulation 2001;104:I8-11. [PubMed]
- Flameng W, Herijgers P, Bogaerts K. Recurrence of mitral valve regurgitation after mitral valve repair in degenerative valve disease. Circulation 2003;107:1609-13. [PubMed]