Minimally invasive aortic valve replacement: 12-year single center experience
Introduction
Aortic valve disease is a prevalent disorder that affects approximately 2% of the adult general population (1). Aortic stenosis is one of the most frequently acquired diseases of the cardiac valves, and most commonly affects the elderly (2). Surgical aortic valve replacement (AVR) via complete median sternotomy is a safe and time-tested technique associated with excellent short- and long-term outcome. It remains the gold standard treatment for symptomatic aortic valve disease and improves the life quality and life expectancy in the operated patients. To reduce surgical trauma, over the last two decades, different minimally-invasive approaches for AVR have been developed and are increasingly being utilized (3,4).
Several minimally invasive approaches (including the right parasternal approach, upper and lower ministernotomy (MS), V-shaped, Z-shaped, inverse-T, J-, reverse-C and reverse-L partial MS, transverse sternotomy and right minithoracotomy,) have been developed for AVR since 1993 (5-8) and have been associated with better outcomes and lower perioperative morbidity compared to full sternotomy (9-16). Minimally invasive approaches enable equally successful valve procedures, while reducing bleeding, pain, infection, and length of stay, as well as improving cosmesis, recovery, and patient satisfaction. Furthermore, economic (17) and survival (18) benefits have been reported for the minimally invasive against conventional sternotomy AVR. Subsequently, minimally invasive surgery for aortic valve disease has become a standard approach in several centers all over the world because of its proven advantages. Partial sternotomy seems to be the most widely adopted option for minimally invasive AVR (6,10,19-24). Although most surgeons that perform less invasive aortic valve surgery prefer a “J-shaped” partial upper sternotomy with entry into the third or the fourth right intercostal space (ICS) (25,26), the right anterior minithoracotomy (RAMT) has the potential to be associated with improved outcomes (7,12,14,16,27,28). The excellent results of minimally invasive valve surgery have been proposed as the reference standard to which emerging technologies should be compared (4,23,24,29-31).
This study reports the single centers experience on minimally invasive aortic valve replacement (MIAVR) through a RAMT or MS approach and describes the surgical technique, complication rates, and patient outcomes.
Methods
Study population and design
This was a retrospective, observational, cohort study of prospectively collected data from 853 consecutive patients (448 males, median age 73.8 years) with aortic valve disease who underwent minimally invasive AVR from September 2002 to May 2014. Patients who underwent aortic valve repair, aortic root replacement, ascending aorta replacement, valve-preserving aortic root replacement, or transcatheter aortic valve implantation were excluded. All patients were seen 2 to 3 months postoperatively and thereafter, were contacted for follow-up data. Follow-up information was obtained by telephone calls, e-mail, surface mail, or interview.
Interventions
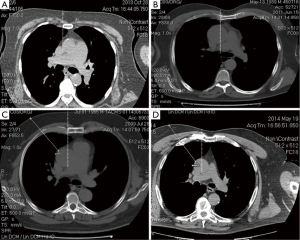
Computed tomography (CT) was used for surgical planning in 98% of patients. A 64-slice chest CT scan (Toshiba Aquilion ONE; Toshiba Medical System, Tokyo, Japan) without contrast enhancement was obtained to evaluate the anatomic relationship between the ICSs, sternum, ascending aorta, and aortic valve. Two CT-criteria of fundamental importance have been elaborated to choose between RAMT and MS: (I) completely retrosternal (Figure 1A) or relatively right lateral (Figure 1B) position of the ascending aorta, at the level of the pulmonary artery bifurcation; (II) a deeper chest (distance between the ascending aorta and the sternum 10 cm or more) (Figure 1C,D). The retrosternal position of the ascending aorta and the deep thorax were considered unfavourable anatomic conditions for the RAMT approach.
Upper MS through the 2nd (V-shaped), 3rd (J or inverted T) or 4th (J type) ICS was performed in the MS group, and the RAMT was done through the 2nd or the 3rd ICS, without rib resection. In the majority of patients, central aortic cannulation and standard (direct) clamping were achieved through the main surgical site, and venous cannulation was performed percutaneously through the groin. Standard implantation techniques for both sutured and sutureless prostheses were implemented. Intraoperative transoesophageal echocardiography was used routinely for the assessment of cardiac function, proper positioning of the percutaneous venous cannula, early surgical results and adequacy of air-removal. At the end of surgery, patients were transferred to the intensive care unit (ICU) and managed according to the unit protocol.
Data collection
The clinical audit committee of the G. Pasquinucci Heart Hospital institutional board approved the study to meet ethical and legal requirements, and written informed consent was waived. The completed data collection forms were entered in local databases and included several sections completed by the anaesthesiologists, cardiac surgeons, ICU personnel, and perfusionists involved in the care of the patients.
Statistical analysis
Patients’ demographic and operative data are expressed as mean ± standard deviation, medians (interquartile range, IQR, 25th-75th percentiles) or as prevalence percentages, as appropriate. Survival was evaluated using the Kaplan-Meier method. The Cox multivariable proportional hazards regression model, based on 89 pre- and postoperative variables, was developed to identify independent predictors of follow-up mortality in the studied population and to assess the weight of surgical approach in the late survival rate. Hazard ratios (HRs) with 95% CIs were calculated for each of the significant risk factors.
All reported probability values are two-tailed, and probability values of less than 0.05 were considered statistically significant. All statistical analysis was performed with SPSS software, version 19.0 (SPSS Inc, Chicago, IL, USA).
Results
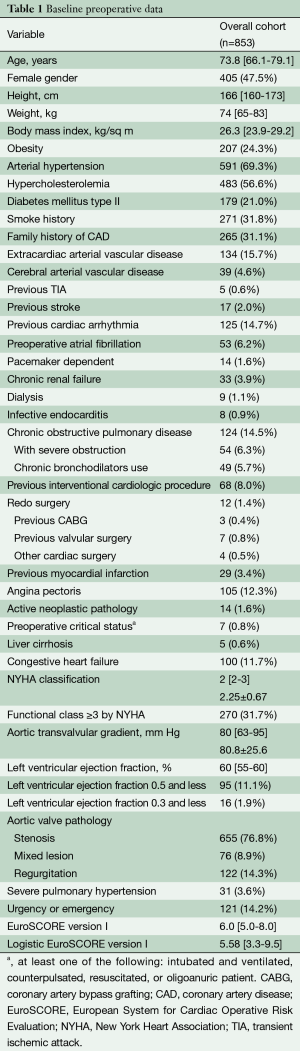
Demographic and baseline data
Patients’ preoperative variables, demographics, risk factors, and comorbidities are summarized in Table 1. The study cohort included 592 (309 males; median age 73.8) procedures performed through RAMT and 261 (139 males; median age 73.7) through MS. The median follow-up period was 29.1 months (interquartile range, 16.8-55.0 months; cumulated follow-up 2,676.0 patient-years), and the follow-up data were 98.2% complete. Redo surgery was performed in 12 (1.4%) patients.
Full table
Intraoperative data
The distribution of the received prosthesis type, operative times and other intraoperative data are shown in Table 2. A total of 443 (51.9%) and 368 (43.1%) patients received biological and sutureless prostheses, respectively. Median size of implanted prostheses was 23 (interquartile range, 23-25) mm. Median cardiopulmonary bypass (CPB) time and aortic cross-clamping time were 108 and 75 min, respectively. In 50 (8.4%) patients in the RAMT group, vs. 3 (1.1%) patients in the MS group, femoral arterial cannulation was used to establish CPB (P<0.0001). Associated procedures [mainly mitral valve surgery and atrial fibrillation (AF) ablation] (P=0.001) and sutureless or fast deployment prostheses (P<0.001) were more frequent in the RAMT. Six (2.3%) conversions to median sternotomy were necessary in the MS group vs. thirteen (2.2%) (P=0.93) in the RAMT group (Table 2).

Full table
Perioperative outcomes
The main clinical outcomes of the two cohorts are presented in Table 3. Overall 30-day mortality was 1.9% (nine patients in the RAMT and seven patients in the MS group, P=0.28). Median ICU stay was one day, median mechanical ventilation time was 6 h, and median hospital stay was six days. Thirty-seven (4.3%) patients required re-exploration for bleeding. No blood products were used in 671 (78.7%) patients. Perioperative stroke was reported in 15 (1.8%) patients, while transient ischemic attack occurred postoperatively in 11 (1.3%) patients. In 243 (28.5%) patients, new onset AF was reported.

Full table
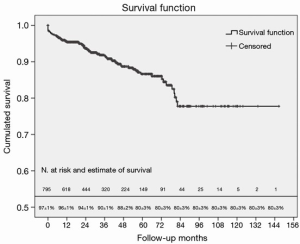
Survival outcomes
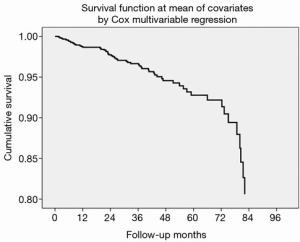
During the median follow-up period of 29.1 months (interquartile range, 16.8-55.0 months; cumulated follow-up 2,676.0 patient-years), 66 deaths were registered, with 33 occurring in the RAMT group. In the general cohort, leading causes were cardiac (32 patients, including 5 valve-related deaths), followed by pulmonary (14 patients), oncological (8 patients), neurological (6 patients), and infection-related (4 patients). Survival in the overall cohort was 96%±1% at 1 year, and 80%±3% at 5 years (Figure 2). Actuarial freedom from reoperation at 5 years was 97.5%±2%.
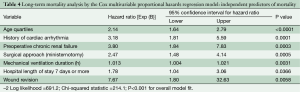
Univariate and multivariate analysis
Forty-three factors have been associated with follow-up mortality by univariate analysis (P≤0.10 criterion), and subsequently have been included in multivariable regression model. Using the Cox multivariable proportional hazards regression model, which demonstrated good overall fit (–2 Log likelihood =691.2; Chi-squared statistic =214.1; P<0.001 for overall model fit), seven factors have been independently associated with the long-term survival: advanced age, history of cardiac arrhythmia, preoperative chronic renal failure, MS approach, prolonged mechanical ventilation and hospital stay, and wound revision (Table 4). A Cox multivariate-adjusted survival curve is demonstrated in Figure 3.
Full table
Learning curve
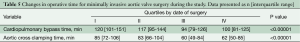
To better assess the effect of growing experience, we compared the perfusion times in the patients operated on before or after February 2012 (median of the study time-frame). For both CPB [119 (98-147) vs. 98 (80-125) min, P<0.0001] and aortic cross clamping [84 (69-105) vs. 61 (50-85) min, P<0.0001], there was a significant time reduction in the second half of the study. This effect remained statistically significant when comparing the quartiles of patients by date of surgery (Table 5).
Full table
Discussion
Different minimally invasive approaches have been developed for AVR over the years, including partial upper sternotomy, right parasternal thoracotomy or transverse sternotomy, with common goals of reducing invasiveness and surgical trauma. With developments in perfusion technology that accommodate CPB through smaller incisions, and the institution of carbon dioxide insufflation and intraoperative transesophageal echocardiography, minimally invasive aortic valve surgery has evolved into a routinely performed operation with excellent results (9,10,18,24).
Currently, the upper partial sternotomy with unilateral J-shaped extension to the right through the fourth ICS seems the most popular minimal access approach (10,19-26). Despite widespread adoption of limited sternotomy approaches for MIAVR and its outstanding achievements in terms of life quality and duration, several studies reported only marginal benefits (10,32) or did not find at all significant difference between mini-access and conventional AVR (19,21,33-36).
Our present study shows that both RAMT and MS are technically feasible and safe approaches, with low perioperative mortality and complications, and result in acceptable surgical results. In the majority of prior reports, MIAVR was associated with longer operative times compared with conventional sternotomy (10,19), but shorter duration of surgery with minimal access was also reported (20). Physically limited exposure and little space to operate are intrinsic drawbacks of minimally invasive approaches. With less room to manipulate, the use of HeartPort instruments is frequently required. However, operative duration can be reduced over time with growing experience as surgeons traverse the learning curve. This may at least in part explain the dynamics of CPB and aortic cross clamping times, which have shortened over time. Similar trends have been demonstrated in other, large centers experienced in MIAVR (9). Another important factor was the introduction of sutureless or rapid deployment prostheses in our clinical practice in 2011. Sutureless prostheses drastically reduce the implantation time, and contribute to the reduction of CPB, cross clamping, and overall operation time. As much as 43.1% of subjects enrolled in the present study received sutureless or rapid deployment prostheses.
Shorter ventilation times (16,35,37) and ICU/hospital stays (11-13,15,20,28) have been reported for MIAVR by high volume centers, but were less evident in pooled studies (10,19,24).
Numerous studies have addressed the incidence of new onset AF—the most frequent arrhythmia in cardiac surgery—after mini-access and conventional AVR. Notable controversy exists in available literature on the matter: while new onset AF reduction (12,16) has been reported in several studies, no difference between minimally invasive and full sternotomy approaches was found by other authors (10,19,20,28,33,35,38,39).
MS and RAMT approaches allow a smaller pericardial incision and exposed area, as well as anatomical and electrical integrity of the percutaneously cannulated right atrium, which reduces the inflammatory response. In addition, an intact sternum (for RAMT) would result in less postoperative pain, reducing the likelihood of AF. RAMT is known to be most often performed using peripheral CPB (40). The relatively higher rate of femoral arterial cannulation in the RAMT cohort in the current study may result from a learning curve effect (six attending surgeons have been in training since 2005); nowadays femoral perfusion is quite unusual in our practice, being reserved only for particular cases. The retrograde perfusion is not a physiological one, and may increase the incidence of perioperative cerebrovascular accident and groin vascular complications.
Although there is still a role for conventional sternotomy for AVR, minimally invasive techniques will continue to increase in popularity and may benefit the patient with shorter postoperative course, less morbidity, and decreased overall cost. Furthermore, minimally invasive approaches may be further facilitated by the development of sutureless or rapid deployment prostheses (41), which may reduce the CPB and cross-clamp durations. The results of the current study should be considered when commencing a minimally invasive AVR program by a single surgeon or entire department. New emerging technologies in the field of AVR should also be compared with the excellent results of minimally invasive approaches, before being widely adopted as a benchmark procedure.
Limitations
The present study is constrained by several limitations. It is based on a retrospective analysis of our large, institutional, observational, prospectively collected database, and thus it reflects a single center experience only and carries all the limits that a retrospective analysis design implies. Our internal institutional electronic database contains EuroSCORE I based records, instead of the newly introduced and more efficient EuroSCORE II. This study also reflects our initial experience with the two minimally invasive approaches and encompasses the ‘learning curve’.
There may be biases that could confound our findings, which were not adjusted for (e.g., personal performance of each surgeon). We might have been unable to account for the influence of any residual unmeasured factors that could affect the adverse outcomes. We fully recognize that our case series is widely variegated and comprises different clinical scenarios. The extremely heterogeneous study population may account for the skewedness of continuous data and abnormal distribution of dichotomous data.
We have utilized all-cause mortality data, though reliably obtained from our database, rather than the more specific cardiac-related mortalities and we did not address the relative incidence of nonfatal cardiac-related events. At the same time however, comprehensive analysis was performed on the whole study population, without any selection. Thus, to the best of our knowledge, this study comprises the largest contemporary single center experience with right minithoracotomy and ministernotomy AVR.
Conclusions
MIAVR via both approaches is safe and feasible with excellent outcomes, and is associated with low conversion rates and low perioperative morbidity. Long term survival is at least comparable to that reported for conventional sternotomy AVR.
Acknowledgements
Disclosure: Dr. Glauber M and Dr. Solinas M have to disclose a commercial/financial relationship with Sorin Group. The other authors declare no conflict of interest.
References
- Nkomo VT, Gardin JM, Skelton TN, et al. Burden of valvular heart diseases: a population-based study. Lancet 2006;368:1005-11. [PubMed]
- Iung B, Baron G, Butchart EG, et al. A prospective survey of patients with valvular heart disease in Europe: The Euro Heart Survey on Valvular Heart Disease. Eur Heart J 2003;24:1231-43. [PubMed]
- Schmitto JD, Mokashi SA, Cohn LH. Minimally-invasive valve surgery. J Am Coll Cardiol 2010;56:455-62. [PubMed]
- Johnston WF, Ailawadi G. Surgical management of minimally invasive aortic valve operations. Semin Cardiothorac Vasc Anesth 2012;16:41-51. [PubMed]
- Rao PN, Kumar AS. Aortic valve replacement through right thoracotomy. Tex Heart Inst J 1993;20:307-8. [PubMed]
- von Segesser LK, Westaby S, Pomar J, et al. Less invasive aortic valve surgery: rationale and technique. Eur J Cardiothorac Surg 1999;15:781-5. [PubMed]
- Ruttmann E, Gilhofer TS, Ulmer H, et al. Propensity score-matched analysis of aortic valve replacement by mini-thoracotomy. J Heart Valve Dis 2010;19:606-14. [PubMed]
- Ito T, Maekawa A, Hoshino S, et al. Right infraaxillary thoracotomy for minimally invasive aortic valve replacement. Ann Thorac Surg 2013;96:715-7. [PubMed]
- Tabata M, Umakanthan R, Cohn LH, et al. Early and late outcomes of 1000 minimally invasive aortic valve operations. Eur J Cardiothorac Surg 2008;33:537-41. [PubMed]
- Brown ML, McKellar SH, Sundt TM, et al. Ministernotomy versus conventional sternotomy for aortic valve replacement: a systematic review and meta-analysis. J Thorac Cardiovasc Surg 2009;137:670-679.e5.
- Korach A, Shemin RJ, Hunter CT, et al. Minimally invasive versus conventional aortic valve replacement: a 10-year experience. J Cardiovasc Surg (Torino) 2010;51:417-21. [PubMed]
- Glower DD, Desai BS, Hughes GC, et al. Aortic valve replacement via right minithoracotomy versus median sternotomy: a propensity score analysis. Innovations (Phila) 2014;9:75-81; discussion 81.
- Khoshbin E, Prayaga S, Kinsella J, et al. Mini-sternotomy for aortic valve replacement reduces the length of stay in the cardiac intensive care unit: meta-analysis of randomised controlled trials. BMJ Open 2011;1:e000266. [PubMed]
- Sharony R, Grossi EA, Saunders PC, et al. Minimally invasive aortic valve surgery in the elderly: a case-control study. Circulation 2003;108 Suppl 1:II43-7. [PubMed]
- Sharony R, Grossi EA, Saunders PC, et al. Propensity score analysis of a six-year experience with minimally invasive isolated aortic valve replacement. J Heart Valve Dis 2004;13:887-93. [PubMed]
- Glauber M, Miceli A, Gilmanov D, et al. Right anterior minithoracotomy versus conventional aortic valve replacement: a propensity score matched study. J Thorac Cardiovasc Surg 2013;145:1222-6. [PubMed]
- Rodriguez E, Malaisrie SC, Mehall JR, et al. Right anterior thoracotomy aortic valve replacement is associated with less cost than sternotomy-based approaches: a multi-institution analysis of ‘real world’ data. J Med Econ 2014;17:846-52. [PubMed]
- Merk DR, Lehmann S, Holzhey DM, et al. Minimal invasive aortic valve replacement surgery is associated with improved survival: a propensity-matched comparison. Eur J Cardiothorac Surg 2015;47:11-7. [PubMed]
- Murtuza B, Pepper JR, Stanbridge RD, et al. Minimal access aortic valve replacement: is it worth it? Ann Thorac Surg 2008;85:1121-31. [PubMed]
- Bakir I, Casselman FP, Wellens F, et al. Minimally invasive versus standard approach aortic valve replacement: a study in 506 patients. Ann Thorac Surg 2006;81:1599-604. [PubMed]
- Furukawa N, Kuss O, Aboud A, et al. Ministernotomy versus conventional sternotomy for aortic valve replacement: matched propensity score analysis of 808 patients. Eur J Cardiothorac Surg 2014;46:221-6; discussion 226-7. [PubMed]
- Gosev I, Kaneko T, McGurk S, et al. A 16-year experience in minimally invasive aortic valve replacement: context for the changing management of aortic valve disease. Innovations (Phila) 2014;9:104-10; discussion 110.
- Goldstone AB, Joseph Woo Y. Minimally invasive surgical treatment of valvular heart disease. Semin Thorac Cardiovasc Surg 2014;26:36-43. [PubMed]
- Phan K, Xie A, Di Eusanio M, et al. A meta-analysis of minimally invasive versus conventional sternotomy for aortic valve replacement. Ann Thorac Surg 2014;98:1499-511. [PubMed]
- Woo YJ. Minimally invasive valve surgery. Surg Clin North Am 2009;89:923-49. [PubMed]
- Raja SG, Benedetto U, Amrani M. Aortic valve replacement through J-shaped partial upper sternotomy. J Thorac Dis 2013;5 Suppl 6:S662-8. [PubMed]
- Miceli A, Murzi M, Gilmanov D, et al. Minimally invasive aortic valve replacement using right minithoracotomy is associated with better outcomes than ministernotomy. J Thorac Cardiovasc Surg 2014;148:133-7. [PubMed]
- Brinkman WT, Hoffman W, Dewey TM, et al. Aortic valve replacement surgery: comparison of outcomes in matched sternotomy and PORT ACCESS groups. Ann Thorac Surg 2010;90:131-5. [PubMed]
- Hiraoka A, Totsugawa T, Kuinose M, et al. Propensity score-matched analysis of minimally invasive aortic valve replacement. Circ J 2014;78:2876-81. [PubMed]
- Glauber M, Farneti A, Solinas M, et al. Aortic valve replacement through a right minithoracotomy. Multimed Man Cardiothorac Surg 2006;2006:mmcts.2005.001826.
- Phan K, Xie A, Tsai YC, et al. Ministernotomy or minithoracotomy for minimally invasive aortic valve replacement: a Bayesian network meta-analysis. Ann Cardiothorac Surg 2015;4:3-14. [PubMed]
- Scarci M, Young C, Fallouh H. Is ministernotomy superior to conventional approach for aortic valve replacement? Interact Cardiovasc Thorac Surg 2009;9:314-7. [PubMed]
- Aris A, Cámara ML, Montiel J, et al. Ministernotomy versus median sternotomy for aortic valve replacement: a prospective, randomized study. Ann Thorac Surg 1999;67:1583-7; discussion 1587-8. [PubMed]
- Bonacchi M, Prifti E, Giunti G, et al. Does ministernotomy improve postoperative outcome in aortic valve operation? A prospective randomized study. Ann Thorac Surg 2002;73:460-5; discussion 465-6. [PubMed]
- Mächler HE, Bergmann P, Anelli-Monti M, et al. Minimally invasive versus conventional aortic valve operations: a prospective study in 120 patients. Ann Thorac Surg 1999;67:1001-5. [PubMed]
- Dogan S, Dzemali O, Wimmer-Greinecker G, et al. Minimally invasive versus conventional aortic valve replacement: a prospective randomized trial. J Heart Valve Dis 2003;12:76-80. [PubMed]
- Johnston DR, Atik FA, Rajeswaran J, et al. Outcomes of less invasive J-incision approach to aortic valve surgery. J Thorac Cardiovasc Surg 2012;144:852-858.e3.
- Farhat F, Lu Z, Lefevre M, et al. Prospective comparison between total sternotomy and ministernotomy for aortic valve replacement. J Card Surg 2003;18:396-401; discussion 402-3. [PubMed]
- Murtuza B, Pepper JR, Stanbridge RD, et al. Does minimal-access aortic valve replacement reduce the incidence of postoperative atrial fibrillation? Tex Heart Inst J 2008;35:428-38. [PubMed]
- Malaisrie SC, Barnhart GR, Farivar RS, et al. Current era minimally invasive aortic valve replacement: techniques and practice. J Thorac Cardiovasc Surg 2014;147:6-14. [PubMed]
- Phan K, Tsai YC, Niranjan N, et al. Sutureless aortic valve replacement: a systematic review and meta-analysis. Ann Cardiothorac Surg 2015;4:100-11.