Early surgical intervention or watchful waiting for the management of asymptomatic mitral regurgitation: a systematic review and meta-analysis
Introduction
The second most frequently encountered valve disease in Western countries, degenerative mitral regurgitation (MR), is often incidentally discovered in asymptomatic patients (1,2). MR due to degenerative mitral valve disease is surgically repairable in most patients (3,4), and correction routinely improves symptoms and restores life expectancy to that of the general population (5,6). Although most clinicians acknowledge the importance of surgical intervention in symptomatic patients with severe MR, there is continued disagreement regarding routine surgical referral earlier in the disease process, prior to the development of American College of Cardiology/American Heart Association (ACC/AHA) class I triggers (symptoms or left ventricular dysfunction) (7-9). Advocates of a “watchful waiting” approach maintain that untreated asymptomatic severe MR confers no incremental morbidity or mortality if surgery is delayed until the development of specific defined clinical endpoints (6), while proponents of early surgical referral assert that earlier surgery prevents deaths that would otherwise be avoidable (10-12). Discordant views also manifest in the most recent iterations of cardiovascular society practice guidelines; the ACC/AHA task force assigns early mitral valve surgery a class IIa recommendation (“should be considered”) (13), while the European society task force takes a more conservative stance, assigning a class IIb recommendation (“may be considered”) to surgery in asymptomatic individuals (14). Similarly, disagreement persists over referring patients for surgical intervention even earlier in the disease process, prior to the development of ACC/AHA class II triggers (atrial fibrillation or pulmonary hypertension) (13,14).
Initial investigation into the “watchful waiting” strategy demonstrated both safety and efficacy (6). However, in an era of mounting evidence that more centers can achieve less than 1% mortality rates and near 100% repair rates (3,4,15), as well as evidence that in the setting of severe MR, occult myocardial dysfunction is often masked by a “normal” preoperative ejection fraction (16), the “watchful waiting” strategy has recently been re-interrogated (10-12). Despite continued controversy, only a handful of centers have investigated the impact of early surgery for asymptomatic severe MR. The aim of the present study was to compare the effectiveness of a strategy of early surgery to watchful waiting by conducting a systematic review and meta-analysis of management plans for asymptomatic severe MR.
Methods
Search strategy
A systematic review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (17). PubMed, Web of Science, Google Scholar, and The Cochrane Library were queried on October 23, 2014 with no constraint for date, language, or type of publication. The search strategy emphasized sensitivity for asymptomatic mitral valve insufficiency and utilized a series of truth functions to increase specificity for study populations meeting the inclusion criteria (Appendix). For each database, searches included the words “mitral valve insufficiency” and “asympt*”. The electronic search was supplemented with an examination of the reference lists of relevant articles as well as discussion with experts.
Study selection
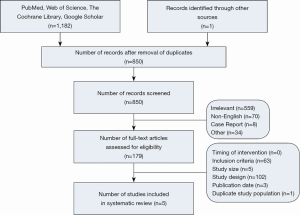
We included any cohort study published in a peer-reviewed journal after 1998 with greater than 100 adult patients with asymptomatic MR who either underwent surgery within 6 months of diagnosis or were subject to watchful waiting. Single-arm studies in which only a watchful waiting strategy was employed were also included in the systematic review. The year 1998 was chosen because it coincides with the introduction of the ACC/AHA practice guidelines suggesting the efficacy of an early surgery approach. Non-English studies were eliminated due to the lack of resources necessary for translation. One investigator (WLP) screened the titles and abstracts of all search results for gross adherence to the study criteria and two authors (ABG and WLP) independently reviewed the full texts of the screened results to confirm the eligibility of each included study (Figure 1).
Data extraction
Data were extracted for the rate of all-cause mortality, cardiac mortality, cardiac events, operative mortality, mitral valve repair, atrial fibrillation, repeat mitral valve surgery, and development of class I or II triggers from all five included studies using a standardized form. Data for actuarial freedom from all-cause mortality in subgroup analyses of patients without atrial fibrillation or pulmonary hypertension were also extracted. Non-perioperative data (all-cause mortality, cardiac mortality, cardiac events, atrial fibrillation, repeat mitral valve surgery, development of class I or II triggers) were extracted at the timepoint closest to 10 years (range, 8-12 years) from study inclusion.
Statistical analysis
Meta-analysis was conducted with Comprehensive Meta-Analysis version 2.2.064 (Biostat Inc., Englewood, New Jersey, USA). Because of heterogeneity in study populations, including differences in inclusion criteria and definitions of early surgery, a random-effects model was used in all analyses. Aggregate proportions, hazard ratios (HR), and relative risks (RR) were used to report pooled estimates. In cases of significant heterogeneity (I2>50%; Cochran Q statistic significance level <0.05), sensitivity analyses were performed to determine whether removal of each study would impact the pooled result. For the primary outcome, a fail-safe N test was performed to evaluate publication bias.
Results
The search strategy and removal of duplicates retrieved 850 title-abstracts for review. Of these, 179 full-text articles were eligible for assessment. Sixty-three articles did not meet the proposed inclusion criteria (most often due to heterogeneity of mitral valve disease or presence of symptoms in the study cohort) and 102 articles were reviews or editorials (Figure 1). Three retrospective observational cohort studies with propensity score adjustment analyses were included for data extraction and analysis (10-12). Two additional cohort studies that only investigated a watchful waiting strategy were included to better understand heterogeneity in results of the conservative approach (5,6). Two studies from Kang and colleagues were derived from the same database. Hence, the study encompassing the larger time frame and that which included an additional study center’s data was included.
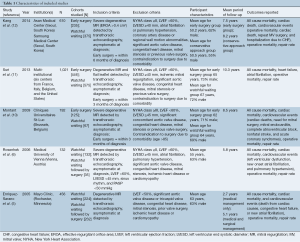
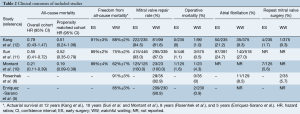
Table 1 summarizes the characteristics of the included studies and provides insight into potential biases in each study. The definition of early surgery varied between studies, and was performed within 3 to 6 months upon diagnosis of severe MR. Additionally, only the studies by Rosenhek and colleagues (6) and Kang and colleagues (12) specifically excluded patients with class II triggers (atrial fibrillation or pulmonary hypertension) on study entry. However, the remaining studies do report results of subgroup analyses performed in patients without class II triggers (10,11). Also of note, patients were younger in the studies by Rosenhek and colleagues (6), and Kang and colleagues (12).
Full table
Long-term all-cause mortality
Two of the three studies reported a significant difference in all-cause mortality between the early surgery and watchful waiting groups (Table 2) (10,11). In the three studies with a comparator arm, 10- to 12-year survival was 89% to 91% in the early surgery cohort and 62% to 88% in the conservative cohort (10-12). However, in an isolated analysis of the watchful waiting approach, Rosenhek and colleagues reported an 8-year survival rate (91%), equivalent to that of the survival of early surgery groups (6).
Full table
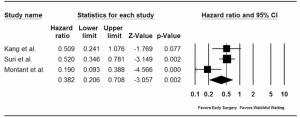
Pooled analysis of the overall study cohorts revealed a significant reduction in long-term mortality with an early surgery approach [HR =0.46; 95% confidence interval (CI): 0.24-0.88]. This survival benefit was even more pronounced in a pooled analysis of the propensity score matched cohorts (HR =0.38; 95% CI: 0.21-0.71) (Figure 2). Furthermore, the benefit of early surgery on survival persisted after a sensitivity analysis was performed to address the significant heterogeneity between studies (I2=67.13%, P=0.05 for Q statistic). Given the strong effect size of the three included studies, 21 unpublished null result studies would be required to bring the new pooled P value to a non-significant level (fail safe N test). To determine whether even earlier surgical intervention improved survival, a pooled analysis of the subgroup without atrial fibrillation or pulmonary hypertension was performed. The reduction in all-cause mortality persisted when those without class II triggers underwent early surgery compared with watchful waiting (RR =0.85; 95% CI: 0.75-0.98). However, significant heterogeneity was noted (I2=86.93%, P<0.001 for Q statistic).
Operative mortality
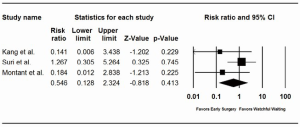
All studies (including the two without an early surgery group) reported operative mortality rates ≤1% (Table 2) (5,6,10-12). Aggregate mortality rates across all five studies revealed an operative mortality of 0.7% in the early surgery cohorts and 0.7% in the watchful waiting cohorts. Meta-analysis corroborated the absence of an incremental risk of operative mortality with a watchful waiting approach (RR =0.55; 95% CI: 0.13-2.32) (Figure 3).
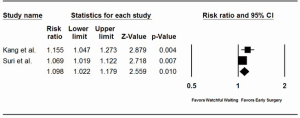
Repair rate
In two of the three comparative effectiveness studies, the rate of mitral valve repair compared with replacement was significantly higher in the early surgery cohorts (Table 2) (11,12). In the third study, Montant and colleagues achieved a 100% repair rate in both groups (10). However, exclusive of the study by Montant and colleagues, the mitral valve was surgically repaired in less than 95% of cases in all studies, regardless of treatment cohort.
Pooled analysis of the comparative effectiveness studies demonstrated that early surgery significantly increased the likelihood of mitral valve repair compared with watchful waiting (RR =1.10; 95% CI: 1.02-1.18) (Figure 4). Although excluded from the pooled analysis because they lack a comparator arm, the watchful waiting studies by Rosenhek and colleagues and Enriquez-Sarano and colleagues both reported repair rates (82.9% and 90.9%, respectively) less than that of the early surgery cohorts in the comparison studies (93% to 100%).
Repeat mitral valve surgery
Three studies included data on the incidence of repeat mitral valve surgery (6,10,12). Kang and colleagues reported similar rates of repeat mitral valve surgery in the early surgery and watchful waiting groups (1.7% vs. 1.0%, respectively, P=1.0) (12). Rates of reoperation in the other two studies were higher; 5.6% of patients required reoperation in the early surgery cohort of Montant and colleagues’ study (10), and mitral reoperations were performed in 5.7% of patients in the watchful waiting cohort of Rosenhek and colleagues’ study (6). Because only one study included data from both treatment arms, pooled analyses of the incidence of repeat mitral valve surgery were not performed.
Atrial fibrillation
Three studies analyzed the incidence of new atrial fibrillation (6,11,12). Although more patients in the early surgery cohort developed atrial fibrillation within the first 3 months of study entry, the overall incidence of atrial fibrillation did not significantly differ between treatment groups over long-term follow-up (24.7% early surgery vs. 27.0% watchful waiting, P=0.89) (11). The incidence of atrial fibrillation was lower in the watchful waiting cohort in the study by Kang and colleagues (21.2% early surgery vs. 9.3% watchful waiting, P<0.0001) (12). This lower rate of atrial fibrillation closely approximated that reported by Rosenhek and colleagues (8.5%) (6). Meta-analyses were not performed because only two studies contained data for both treatment arms.
Development of class I or II triggers
Only the Rosenhek series automatically referred patients for surgery when class I or II triggers developed. In their series, 55% of patients remained free of surgical triggers 8 years after study inclusion (6). In another prospective study of asymptomatic patients with degenerative MR, only 46% of patients remained free from surgical intervention at 5 years (5). However, it should be noted that physician or patient preference was the primary surgical indication in 47 of the 232 patients that underwent surgery.
Discussion
Improvement in the clinical outcomes of the surgical treatment of mitral valve disease has rejuvenated advocacy for earlier intervention in the disease process, prior to the development of symptoms or ventricular dysfunction. Yet, discordance between observational investigations of watchful waiting and early surgery management strategies drives the continued controversy surrounding this issue. This international disagreement resonates in disparate recommendations by American and European professional society practice guidelines. The overall survival benefit and increased likelihood of receiving a mitral valve repair afforded by early surgery in the present meta-analysis supports the more aggressive therapeutic strategy. However, several caveats warrant discussion.
In order to determine the optimal management of asymptomatic severe MR, one must weigh the risks of early surgery against that of watchful waiting. Specifically, is the development of symptoms or adverse sequelae of MR (left ventricular dysfunction, atrial fibrillation, or pulmonary hypertension) inevitable? Also, does waiting to intervene until such triggers develop negatively impact survival or operative outcome?
Not every asymptomatic patient with severe MR rapidly develops symptoms or adverse sequelae of the disease. In the study by Rosenhek and colleagues, 55% of patients remained free of class I or II triggers 8 years after the diagnosis of severe MR, and trigger incidence did not significantly differ between patients with leaflet flail or leaflet prolapse (6). In contrast, in the study by Enriquez-Sarano and colleagues, asymptomatic individuals acquired class I or II triggers at a faster rate; more than half of the patients required surgery within 5 years (5). Because it may predict symptom onset or ventricular dysfunction, stress testing is emerging as a useful prognostic modality in evaluating asymptomatic patients with MR. In fact, twenty percent of “asymptomatic” patients may have significantly reduced exercise capacity and should actually be classified as symptomatic (18). Exacerbation of MR during exercise correlates with poorer symptom-free survival (19,20), and impaired contractile reserve during stress testing may predict significant left ventricular dysfunction in medically treated patients (21). Thus, stress testing may identify those that would most benefit from an early surgery approach if a watchful waiting strategy is employed (8).
Yet, the question remains whether waiting to intervene until class I or II triggers develop worsens survival. In a well-designed prospective study, Rosenhek and colleagues demonstrated excellent survival when patients were only referred for surgery at the onset of class I or II triggers (6). However, in the present study, pooled results from the three published comparison trials revealed a significant reduction in the hazard of death when an early surgical approach was used. It should be noted that over 20% of patients included in the studies by Suri and colleagues and Montant and colleagues had atrial fibrillation and/or pulmonary hypertension, and these class II triggers were more often present in the early surgery group (10,11). However, both investigator groups did conduct sub-group analyses in which patients with these class II triggers were excluded. Using this sub-group data, individual and pooled results again demonstrated a survival benefit in the early surgery cohort. Thus, early surgery even appears to improve survival compared with that of a watchful waiting strategy if employed prior to the development of atrial fibrillation or pulmonary hypertension. Whether that benefit stems only from those that are more likely to rapidly develop symptoms or ventricular dysfunction with medical management cannot be determined with the data currently available.
Apprehension surrounding watchful waiting also originates from concern that inferior surgical outcomes result from delaying surgery. Although operative mortality did not differ between treatment arms in individual or pooled analyses, significantly higher repair rates were achieved in the early surgery cohorts. Because of the inherent risks of prosthetic mitral valves (valve degeneration, thromboembolism, anticoagulant-associated hemorrhage, and endocarditis) and the survival advantage associated with mitral valve repair (22-24), it is critical that patients undergoing surgery for degenerative MR have a very high probability of durable repair, especially those with asymptomatic disease. Current ACC/AHA practice guidelines recommend intervention only if the probability of repair exceeds 95% and expected mortality is less than 1% (13). Although the pooled operative mortality for both groups was less than 1% (0.7% for early surgery vs. 0.7% for watchful waiting), examination of aggregate data across all five studies demonstrates that the 95% repair rate recommended by the ACC/AHA task force was only attained in the early surgery group (94.5% for early surgery vs. 87.7% for watchful waiting). Thus, there may be a disadvantage with respect to repairability with a watchful waiting approach that may potentially impact survival in the long-term. Because of the observational nature of each comparison study, the decision to operate early was at the discretion of physicians. Consequently, those with more complex valve disease may have been preferentially funneled into the watchful waiting cohort. However, examination of the characteristics of each study population reveals that such a bias is likely not the case; the proportions of patients with anterior or bileaflet prolapse were similar in each group (10-12). Also, it must be noted that the centers that conducted these studies were reference centers. At such centers, mitral valve repair rates approach 100% (4,25), compared with national repair rates ranging between 48% and 77% (26). Although repair of isolated single-segment posterior leaflet dysfunction is sufficiently standardized and reproducible, more complex valve dysfunction is significantly more difficult to durably repair. Given the association between surgical expertise, volume, and outcomes, it is advisable that asymptomatic patients with more complex valve pathology be referred to valve centers of excellence if a strategy of early surgery is employed (26).
Considerable heterogeneity in the demographics of each study population may in part account for discordance between the study by Rosenhek and colleagues and the four other studies included in this systematic review. For example, the mean age of patients in the former study (55 years) is substantially lower than that of the studies by Suri and colleagues (65 years), Montant and colleagues (63 years), and Enriquez-Sarano and colleagues (63 years). The relatively young age of patients in the study by Rosenhek and colleagues may therefore limit external validity. In fact, the survival benefit afforded by early surgery is significantly more pronounced in individuals over 50 years of age (12). Additionally, variance in gender distribution amongst the different studies are noted and may further confound inter-study comparisons (8).
Limitations
The strength of any meta-analysis is limited by the strength of the included studies. No randomized trial exists that compares the two management strategies. Because of the observational design of each study, confounding by indication limits internal validity. However, all three comparison studies included in the pooled analyses employed propensity score matching to mitigate this bias. Although the number of patients in each study was relatively large, only three studies could be included in the meta-analysis and conclusions from the pooled analyses must be drawn with the understanding that they are limited by significant heterogeneity. Also, studies do not always report data on the same clinical endpoints. Consequently, important endpoints, such as the incidence of stroke and heart failure, could not be assessed.
Conclusions
Discordant results of observational studies yield disagreement regarding the preferred management of asymptomatic severe MR. The present study represents, to our knowledge, the first systematic review and meta-analysis on this topic, and demonstrates that a strategy of early surgery improves survival and may increase the likelihood of mitral valve repair. Because the studies were conducted in reference centers, one cannot predict whether a survival advantage would persist if a strategy of routine early surgical referral is employed nationally. A randomized comparative effectiveness trial is clearly needed. Until then, management decisions should be individualized to each patient, and asymptomatic patients with higher risk profiles or with more complex valve dysfunction should be referred to expert centers to maximize the probability of a durable repair and optimal outcome.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
Appendix
Detailed search strategy
PubMed was queried using the search term “Mitral Valve Insufficiency”[Mesh] AND asympt* AND (watch* OR wait* OR surg* OR interv* OR repair* OR replace* OR conven* OR treat*)”. This search returned 327 results. Web of Science was queried for the topic “Mitral valve insufficiency” and refined by the search terms “asymptomatic” and “wait* or watch* or interven* or repair* or replace* or conven* or treat*”. This search returned 389 results. Google Scholar was queried for all the words “mitral valve insuf* asymptom* repair*” including the exact phrase “watchful waiting”. This search returned 364 results. The Cochrane Library was querried for trials with the MeSH descriptor “[Mitral Valve Insufficiency] explode all trees and with qualifier(s): [Surgery - SU]” and the qualifier “asympt*”. This search returned 102 results.
In total, our query returned 1,182 results. All search results were imported into EndNote X7. Duplicate search results were identified by the software and 333 were eliminated after a manual review. The remaining 850 results were filtered and abstracts, letters, editorials, and case-reports were eliminated. Results which were published through a non peer-revieved platform or deemed irrelevant (typically on the basis of being in vitro or in non-human species) were eliminated. Non-English results were eliminated because we lack the necessary translation resources.
References
- Freed LA, Levy D, Levine RA, et al. Prevalence and clinical outcome of mitral-valve prolapse. N Engl J Med 1999;341:1-7. [PubMed]
- Devereux RB, Jones EC, Roman MJ, et al. Prevalence and correlates of mitral valve prolapse in a population-based sample of American Indians: the Strong Heart Study. Am J Med 2001;111:679-85. [PubMed]
- Goldstone AB, Atluri P, Szeto WY, et al. Minimally invasive approach provides at least equivalent results for surgical correction of mitral regurgitation: a propensity-matched comparison. J Thorac Cardiovasc Surg 2013;145:748-56. [PubMed]
- Castillo JG, Anyanwu AC, Fuster V, et al. A near 100% repair rate for mitral valve prolapse is achievable in a reference center: implications for future guidelines. J Thorac Cardiovasc Surg 2012;144:308-12. [PubMed]
- Enriquez-Sarano M, Avierinos JF, Messika-Zeitoun D, et al. Quantitative determinants of the outcome of asymptomatic mitral regurgitation. N Engl J Med 2005;352:875-83. [PubMed]
- Rosenhek R, Rader F, Klaar U, et al. Outcome of watchful waiting in asymptomatic severe mitral regurgitation. Circulation 2006;113:2238-44. [PubMed]
- Suri RM, Schaff HV, Enriquez-Sarano M. Mitral valve repair in asymptomatic patients with severe mitral regurgitation: pushing past the tipping point. Semin Thorac Cardiovasc Surg 2014;26:95-101. [PubMed]
- Gillam LD, Marcoff L, Shames S. Timing of surgery in valvular heart disease: prophylactic surgery vs watchful waiting in the asymptomatic patient. Can J Cardiol 2014;30:1035-45. [PubMed]
- Rosenhek R. Watchful waiting for severe mitral regurgitation. Semin Thorac Cardiovasc Surg 2011;23:203-8. [PubMed]
- Montant P, Chenot F, Robert A, et al. Long-term survival in asymptomatic patients with severe degenerative mitral regurgitation: a propensity score-based comparison between an early surgical strategy and a conservative treatment approach. J Thorac Cardiovasc Surg 2009;138:1339-48. [PubMed]
- Suri RM, Vanoverschelde JL, Grigioni F, et al. Association between early surgical intervention vs watchful waiting and outcomes for mitral regurgitation due to flail mitral valve leaflets. JAMA 2013;310:609-16. [PubMed]
- Kang DH, Park SJ, Sun BJ, et al. Early surgery versus conventional treatment for asymptomatic severe mitral regurgitation: a propensity analysis. J Am Coll Cardiol 2014;63:2398-407. [PubMed]
- Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;129:e521-643. [PubMed]
- Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC); European Association for Cardio-Thoracic Surgery (EACTS), Vahanian A, Alfieri O, et al. Guidelines on the management of valvular heart disease (version 2012). Eur Heart J 2012;33:2451-96. [PubMed]
- Svensson LG, Atik FA, Cosgrove DM, et al. Minimally invasive versus conventional mitral valve surgery: a propensity-matched comparison. J Thorac Cardiovasc Surg 2010;139:926-32. [PubMed]
- Quintana E, Suri RM, Thalji NM, et al. Left ventricular dysfunction after mitral valve repair--the fallacy of “normal” preoperative myocardial function. J Thorac Cardiovasc Surg 2014;148:2752-60. [PubMed]
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535. [PubMed]
- Lancellotti P, Magne J. Stress testing for the evaluation of patients with mitral regurgitation. Curr Opin Cardiol 2012;27:492-8. [PubMed]
- Magne J, Lancellotti P, Piérard LA. Exercise-induced changes in degenerative mitral regurgitation. J Am Coll Cardiol 2010;56:300-9. [PubMed]
- Magne J, Lancellotti P, Piérard LA. Exercise pulmonary hypertension in asymptomatic degenerative mitral regurgitation. Circulation 2010;122:33-41. [PubMed]
- Lee R, Haluska B, Leung DY, et al. Functional and prognostic implications of left ventricular contractile reserve in patients with asymptomatic severe mitral regurgitation. Heart 2005;91:1407-12. [PubMed]
- Gillinov AM, Blackstone EH, Nowicki ER, et al. Valve repair versus valve replacement for degenerative mitral valve disease. J Thorac Cardiovasc Surg 2008;135:885-93, 893.e1-2.
- Enriquez-Sarano M, Schaff HV, Orszulak TA, et al. Valve repair improves the outcome of surgery for mitral regurgitation. A multivariate analysis. Circulation 1995;91:1022-8. [PubMed]
- Chikwe J, Goldstone AB, Passage J, et al. A propensity score-adjusted retrospective comparison of early and mid-term results of mitral valve repair versus replacement in octogenarians. Eur Heart J 2011;32:618-26. [PubMed]
- Goldstone AB, Cohen JE, Howard JL, et al. A "repair-all" strategy for degenerative mitral valve disease safely minimizes unnecessary replacement. Ann Thorac Surg 2015. [Epub ahead of print]. [PubMed]
- Gammie JS, O'Brien SM, Griffith BP, et al. Influence of hospital procedural volume on care process and mortality for patients undergoing elective surgery for mitral regurgitation. Circulation 2007;115:881-7. [PubMed]