Minimally invasive thymectomy: the Mayo Clinic experience
Abstract
Background: The prevalence of minimally invasive thymectomy (MIT) is increasing and may have significant benefit to patients in terms of morbidity and post-operative recovery. Our aim was to review the Mayo Clinic experience of MIT.
Methods: We reviewed data from all MIT cases collected in a prospectively maintained database from January 1995 to February 2015. Data were collected regarding patient demographics, perioperative management and patient outcomes.
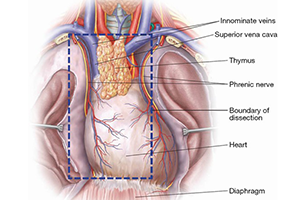
Results: A total of 510 thymectomies were performed in 20 years. Fifty-six patients underwent MIT (45 video-assisted thoracoscopy, 11 robotic-assisted). The median age was 55 years (range, 23-87 years) with male to female ratio of 25:31. Thymoma was the main pathologic diagnosis in 27/56 patients (48%), with 11/27 (41%) associated with myasthenia gravis (MG), and 16/27 (59%) non-MG. Other pathologies included 1/56 (2%) of each teratoma, lymphoma, lymphangioma, carcinoma and thymolipoma. There were 3/56 (5%) atrophic glands, 4/56 (7%) cysts, 6/56 (11%) benign glands and 11/56 (20%) hyperplastic. Mean blood loss (mL) and operative time (min) were significantly lower in the video-assisted thoracoscopic surgery (VATS) group compared to robotic (65±41 vs. 160±205 mL, P=0.04 and 102±39 vs. 178±53 min, P=0.001, respectively). There was no 30-day mortality. Post-operative morbidity occurred in 7/45 (16%) VATS patients (phrenic nerve palsy 7%, pericarditis 4%, atrial fibrillation 2%, pleural effusion 2%) and 1/11 (9%) robotic (urinary retention requiring self-catheterization). Reoperation was required in 1/3 of VATS patients with phrenic nerve palsy. There was no significant difference in length of hospital stay [VATS 1.5 days (range, 1-4 days) and robotic 2 days (range, 1-5 days) VATS; P=0.05]. Mean follow-up was 18.4 months (range, 1-50.4 months) with no tumor recurrences.
Conclusions: MIT can be performed with low morbidity and mortality. VATS is associated with reduced blood loss, operative times and earlier hospital discharge compared to robotic MIT.
Cover