A novel approach to ischemic mitral regurgitation (IMR)
Introduction
Ischemic mitral regurgitation (IMR) is a complicated medical condition with varying degrees of coronary artery disease (CAD) and mitral regurgitation (MR). At its essence, the MR results from ventricular changes induced by myocardial ischemia and/or infarcts. Ventricular remodeling with posterior displacement of the medial papillary muscle generally causes regurgitation. That displacement then leads to restriction of the posterior leaflet and an anteriorly directed regurgitant jet. In some cases, annular dilation from ventricular enlargement can result in MR with a resultant central jet.
Under current guidelines, coronary revascularization is a the mainstay of treatment for this disease; but many questions still surround the best approach to the mitral valve (1). Due to the significance of this problem both for individuals and for society, concerted efforts have been directed to gather evidence on the outcomes of different surgical approaches to better direct treatment. Although most agree that severe IMR requires surgical intervention, the issues of repair versus replacement, as well as necessity of mitral surgery for lesser levels of regurgitation, remain controversial.
In January 2014, a study funded by the National Institute of Health and published in the New England Journal of Medicine found no difference in clinical outcomes between mitral valve repair and mitral valve replacement (MVR) for severe IMR, although a more lasting correction of MR was noted in the replacement group (2). In December 2014, a study investigating the addition of MVR to coronary artery bypass grafting (CABG) in patients with moderate IMR failed to show a meaningful clinical improvement in the patients who underwent mitral repair (3). Thus, many questions remain regarding the optimal treatment for this significant disease process.
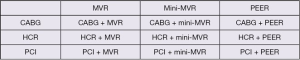
Additionally, more techniques have been developed for approaching the mitral valve and coronary revascularization. This allows for unique combinatorial procedures to address IMR (Figure 1). While most of these treatment options have not been studied in detail, they may present novel solutions to a widely variable and complex IMR patient population. Thus, a comparative analysis including an examination of potential benefits and risks will be helpful and potentially allow for more patient-specific treatment strategies.
Revascularization approaches
Coronary revascularization is fundamental to treating IMR. Three distinct approaches exist that can be distinguished based on level of invasiveness. The first is traditional CABG via a median sternotomy. The second is minimally invasive coronary artery bypass grafting (MIDCAB) with or without the use of robot assistance via the left anterior chest. While a small number of surgeons and institutions are capable of multi-vessel non-sternotomy revascularization, this is not commonplace. A more feasible practice would consist of a minimally invasive left internal mammary artery (LIMA) to left anterior descending (LAD) coronary artery anastomosis combined with percutaneous coronary intervention to the non-LAD territories requiring revascularization, Hybrid Coronary Revascularization (HCR). The third option is multi-vessel PCI alone.
PCI is the least invasive method of coronary revascularization; and while it has short-term morbidity advantages over traditional bypass surgery, it has not been able to meet the long-term benefits in mortality and freedom from revascularization that CABG provides in patients with multi-vessel disease. In fact, the FAME II trial was the first randomized control trial to demonstrate increased survival of PCI over medical therapy for stable coronary artery disease, and this was only after eliminating peri-procedural morbidity and mortality. Fortunately, in-stent restenosis, one of the major limitations of percutaneous revascularization, has decreased with each new generation of coronary stent (4). PCI, however, has yet to match CABG with regard to long-term benefits (5). Multiple studies have consistently demonstrated that for patients with multi-vessel disease and/or left main disease, regardless of the presence of diabetes, CABG yields better outcomes than PCI in terms of mortality, myocardial infarction and need for repeat coronary revascularization (6-9). Even when comparing CABG versus PCI for patients with proximal LAD disease, Hannan et al., showed that CABG patients had lower rates of repeat revascularization (10).
The benefit of CABG over PCI involves the long-term effects of IMA to LAD anastomosis, the potential ability of bypass grafts to ‘treat’ lesions that subsequently develop and resultant downstream effects of cytokines on arterial disease (11,12). On the other hand, PCI offers significantly lower rates of morbidity, including stroke, renal failure and shorter hospital stay.
HCR is a revascularization strategy that attempts to combine the advantages of CABG and PCI. The LIMA to LAD anastomosis is done off-pump through a small left anterior thoracotomy, thereby eliminating aortic manipulation and the need for cardiopulmonary bypass, both of which increase the risk of procedural complications, including stroke, while providing the long-term benefit of IMA. PCI can be employed to resolve significant non-LAD coronary lesions. Recent studies on HCR have demonstrated that the results of this method are equivalent to the benefits of open CABG along with the morbidity advantages of PCI. Halkos et al. reviewed 300 patients who underwent HCR over a 9-year period. Their cohort had a 1.3% mortality rate, 1% stroke rate, 4.8% need for repeat revascularization and a 96% LIMA patency rate (13). These results are comparable to traditional CABG with a potentially decreased rate of stroke. In addition, Harskamp et al. compared HCR to CABG in a propensity-matched analysis in over 1,000 patients over 10 years. Their study demonstrated similar mortality between HCR and CABG but HCR was associated with a significantly lower rate of hospital morbidity, including re-operation, renal failure, prolonged ventilation, infection, transfusions and shorter hospital stays (14). Finally, Zhu et al. performed a meta-analysis comparing HCR to CABG and found that HCR was comparable to CABG in terms of mortality, myocardial infarction, stroke, atrial fibrillation and renal failure but had significantly lower rates of transfusions and shorter ICU and hospital stays (15). While these studies are limited in the length of follow-up and lack of randomization, they warrant further evaluation. The results are promising and establish HCR as a revascularization strategy combining the benefits of PCI and CABG.
Mitral regurgitation (MR) approaches
For patients with MR and an indication for intervention, treatment options can also be distinguished, based on level of invasiveness, into three categories. MVR has traditionally been performed through a median sternotomy with cardiopulmonary bypass and exposure of the mitral apparatus through Sondergaard’s groove, the inter-atrial septum or less commonly the dome of the left atrium. The minimally invasive mitral operation (mini-MVR), via the right chest, is a second option. Finally, a percutaneous edge-to-edge repair of the mitral valve (PEER), simulating an Alfieri stitch, is possible.
Minimally invasive techniques, initially developed in the 1990s, involve exposure through a right anterior thoracotomy with or without the use of a robot. Variations of this procedure with respect to cardiopulmonary bypass management range from cold fibrillatory arrest to cardioplegic arrest with either a transthoracic aortic cross clamp or a balloon endoclamp. A recent study from the University of Pennsylvania compared outcomes of MVR with mini-MVR in over 200 propensity-matched pairs, including a small group of patients with IMR (16). In this study, patients undergoing mini-MVR had longer ischemic and cardiopulmonary bypass times, yet they demonstrated equivalent outcomes for in-hospital hospital mortality, renal failure, atrial fibrillation, stroke and 9-year mortality. Furthermore, transfusion, 30-day readmission rates and post-repair MR were found to be lower in the mini-MVR group. Additionally, a meta-analysis from Cao et al. that analyzed seven studies (including one randomized controlled trial) that compared these two mitral approaches in patients with degenerative disease found no difference in outcomes (17). This data suggest that outcomes, including long-term survival of patients undergoing mini-MVR, are comparable to MVR.
Another option, PEER, specifically involving mal-coaptation of the anterior and posterior leaflets, now exists as a feasible treatment option for MR. PEER involves percutaneous venous access, puncture through the inter-atrial septum, and deployment of a clip to secure the edges of the mitral leaflets and decrease or eliminate the regurgitant jet. The clip limits retrograde systolic flow while still allowing sufficient diastolic left ventricular filling. In 2011, the initial EVEREST II data was published (18). This study randomized patients with 3-4+ MR into traditional MVR and PEER approaches and compared outcomes up to one year after intervention. While patients in the PEER cohort had significantly fewer major adverse events at 30 days, a significant portion ultimately required MVR, thus failing to meet equivalence with regard to efficacy. A four-year follow up study confirmed these results (19). Glower et al., however, recently reported one-year data for high-risk patients, defined by an STS risk greater than or equal to 12%, with 3-4+ MR who underwent PEER (20). They found that PEER significantly decreased the degree of MR and improved symptoms as reported by a decrease in NYHA status while imparting less mortality and morbidity than an open procedure. Interestingly, most of these patients had IMR (70%) and previous CABG (60%). Taken together, these sources suggest that while PEER may be a less attractive treatment option for most MR patients, it may yet find a niche within the previously described high-risk group and may provide another alternative for treating IMR.
Ischemic mitral regurgitation (IMR) approaches
IMR is an important disease process and therapy has focused on both revascularization and repair or replacement of the mitral valve for at least those with severe MR. Three separate treatment modalities exist for both revascularization and restoring competency of the mitral valve. Therefore, at least in theory, the treatment options for IMR include nine possible approaches: CABG + MVR, CABG + mini-MVR, CABG + PEER, HCR + MVR, HCR + mini-MVR, HCR + PEER, PCI + MVR, PCI + mini-MVR, and PCI +PEER (Figure 1).
Two of the options—HCR + MVR and CABG + mini-MVR—are not reasonable and do not warrant further discussion. Of the seven remaining, one—CABG + MVR—is the current standard of care. The remaining six have various attributes that could make them relevant to subsets of IMR patients for whom the current standard of care falls short or could be improved. These six options are discussed further below:
CABG + PEER
At face value, it would seem counterintuitive for a patient to undergo the most invasive treatment option for coronary revascularization and the least invasive approach to treating his or her MR. Several arguments for this approach can nonetheless be made. Cardiopulmonary bypass and aortic cross clamping could be eliminated if the CABG was performed off-pump. Furthermore, the PEER device could be placed directly through the left or right atrium, or potentially through the left ventricle—though this would require modification of the current device—simplifying the technical procedure. This could be beneficial in patients with significant renal disease or where significant concern exists for potential neurological impairment or blood loss.
HCR + PEER
During this procedure, revascularization would be provided by techniques for HCR described above. PEER could be performed during the same anesthetic via a femoral approach or possibly through direct left atrial or left ventricular access. Alternatively, the PEER portion of the procedure could be staged. As with CABG + PEER, an advantage is that the need for cardiopulmonary bypass is no longer absolute. Furthermore, with this approach coronary revascularization is achieved with both PCI and LIMA to LAD bypass, thereby resulting in a less significant incision while providing the long-term benefits of LIMA grafting. Whether this method provides an equivalent revascularization result as traditional CABG likely depends on the degree of non-LAD coronary disease; but this combination could still be useful in patients who are at high operative risk.
PCI + PEER
This combination of techniques is the least invasive and minimizes the significant risks of surgery. In addition, depending on patient risk factors, these procedures could easily be performed together or staged. Nonetheless, given the limited efficacy of both procedures in treating multi-vessel coronary disease and MR, relative to more invasive approaches, only a select subgroup of high-risk patients with the appropriate coronary lesions suitable for PCI and mitral pathology amenable to PEER could benefit from this approach.
HCR + mini-MVR
In this approach, a left anterior thoracotomy would allow LIMA-LAD bypass, under direct visualization or with thoracoscopic/robotic assistance for IMA procurement. PCI of the non-LAD lesions could be performed either at the same setting or staged before or after the MIDCAB. This could be followed by mini-MVR. This strategy ensures optimal myocardial protection during the mitral correction. Sternal integrity is also maintained. In addition, a recent group performed PCI and valve surgery during the same procedure indicating that a single staged HCR/mini-MVR is feasible (21).
Although no large studies have looked directly at HCR + mini-MVR, several groups have investigated hybrid approaches of PCI combined with valve operations. In 2014, Santana et al., published the results of over 200 patients who underwent PCI for coronary revascularization followed by a minimally invasive valve procedure. They found a mortality rate of 3.6% and an all-cause mortality rate of 12% at 4.5 years. They also demonstrated a decreased complication rate and length of stay for the hybrid group compared to those undergoing conventional sternotomy (22).
PCI + MVR & PCI + mini-MVR
Another option for the treatment of IMR consists of multi-vessel PCI for revascularization followed by mitral repair or replacement either through a sternotomy or right anterior thoracotomy. While these approaches do not provide the benefits of IMA grafting, they would provide an alternative for patients with an unusable LIMA or unsuitable LAD target. Additionally, the minimally invasive approach for the mitral valve could provide a significant reduction in morbidity. Furthermore, this approach can be performed without aortic cross-clamping, allowing patients with significant aortic disease to undergo the operation.
George et al. recently described a series of 26 patients who underwent a single-stage hybrid procedure involving PCI of a non-LAD vessel followed by a valve operation (21). Recalculating the STS risk after the PCI was performed, they found a 35% risk reduction in the re-operative group and a 17% risk reduction in the non re-operative group. In addition, they had no in-hospital mortalities and very few complications. No coronary-stent thromboses were noted during a follow-up period of two years.
Although there is less morbidity and mortality associated with a hybrid approach, several groups have observed an increased incidence of acute kidney injury when both PCI and a valve procedure are performed on the same day. This prompted the recommendation of establishing a period of three weeks between the PCI and valve operation (23,24). Additionally, there is a potential for increased bleeding if PCI is done prior to surgery due to the administration of clopidogrel (25), although there is evidence suggesting this risk may not be significant (21,26).
Conclusions
More treatment options exist for IMR than traditional CABG ± MVR. The potential benefits of employing these techniques include reducing in-hospital morbidity and mortality, especially for high-risk patients. In many instances, mid- and long-term results for minimally invasive surgical approaches for the treatment of coronary disease and MR compare favorably to those of more conventional surgical procedures. Percutaneous approaches to the treatment of multi-vessel CAD and MR offer advantages in certain subsets of patients that are unable or unwilling to undergo more traditional surgical procedures. Tailoring the approach to individual patient pathology and comorbidities is feasible and offers potentially better treatment paradigms for IMR.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Bonow RO, Carabello BA, Chatterjee K, et al. 2008 focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1998 guidelines for the management of patients with valvular heart disease). Endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol 2008;52:e1-142. [PubMed]
- Acker MA, Parides MK, Perrault LP, et al. Mitral-valve repair versus replacement for severe ischemic mitral regurgitation. N Engl J Med 2014;370:23-32. [PubMed]
- Smith PK, Puskas JD, Ascheim DD, et al. Surgical treatment of moderate ischemic mitral regurgitation. N Engl J Med 2014;371:2178-88. [PubMed]
- Smit Y, Vlayen J, Koppenaal H, et al. Percutaneous coronary invervention versus coronary artery bypass grafting: a meta-analysis. J Thorac Cardiovasc Surg 2015;149:831-8.e1-13.
- Park SJ, Ahn JM, Kim YH, et al. Trial of everolimus-eluting stents or bypass surgery for coronary disease. N Engl J Med 2015;372:1204-12. [PubMed]
- Marui A, Kimura T, Nishiwaki N, et al. Five-year outcomes of percutaneous versus surgical coronary revascularization in patients with diabetes mellitus (from the CREDO-Kyoto PCI/CABG Registry Cohort-2). Am J Cardiol 2015;115:1063-72. [PubMed]
- Kurlansky P, Herbert M, Prince S, et al. Improved long-term survival for diabetic patients with surgical versus interventional revascularization. Ann Thorac Surg 2015;99:1298-305. [PubMed]
- Farkouh ME, Domanski M, Sleeper LA, et al. Strategies for multivessel revascularization in patients with diabetes. N Engl J Med 2012;367:2375-84. [PubMed]
- Sipahi I, Akay MH, Dagdelen S, et al. Coronary artery bypass grafting vs percutaneous coronary intervention and long-term mortality and morbidity in multivessel disease: Meta-analysis of randomized clinical trials of the arterial grafting and stenting era. JAMA Intern Med 2014;174:223-30. [PubMed]
- Hannan EL, Zhong Y, Walford G, et al. Coronary artery bypass graft surgery versus drug-eluting stents for patients with isolated proximal left anterior descending disease. J Am Coll Cardiol 2014;64:2717-26. [PubMed]
- Tatoulis J, Buxton BF, Fuller JA. Patencies of 2127 arterial to coronary conduits over 15 years. Ann Thorac Surg 2004;77:93-101. [PubMed]
- Hayward PA, Buxton BF. Contemporary coronary graft patency: 5-year observational data from a randomized trial of conduits. Ann Thorac Surg 2007;84:795-9. [PubMed]
- Halkos ME, Walker PF, Vassiliades TA, et al. Clinical and angiographic results after hybrid coronary revascularization. Ann Thorac Surg 2014;97:484-90. [PubMed]
- Harskamp RE, Vassiliades TA, Mehta RH, et al. Comparative Effectiveness of Hybrid Coronary Revascularization vs Coronary Artery Bypass Grafting. J Am Coll Surg 2015;221:326-334.e1.
- Zhu P, Zhou P, Sun Y, et al. Hybrid coronary revascularization versus coronary artery bypass grafting for multivessel coronary artery disease: systematic review and meta-analysis. J Cardiothorac Surg 2015;10:63. [PubMed]
- Goldstone AB, Atluri P, Szeto WY, et al. Minimally invasive approach provides at least equivalent results for surgical correction of mitral regurgitation: a propensity-matched comparison. J Thorac Cardiovasc Surg 2013;145:748-56. [PubMed]
- Cao C, Gupta S, Chandrakumar D, et al. A meta-analysis of minimally invasive versus conventional mitral valve repair for patients with degenerative mitral disease. Ann Cardiothorac Surg 2013;2:693-703. [PubMed]
- Feldman T, Foster E, Glower DD, et al. Percutaneous repair or surgery for mitral regurgitation. N Engl J Med 2011;364:1395-406. [PubMed]
- Mauri L, Foster E, Glower DD, et al. 4-year results of a randomized controlled trial of percutaneous repair versus surgery for mitral regurgitation. J Am Coll Cardiol 2013;62:317-28. [PubMed]
- Glower DD, Kar S, Trento A, et al. Percutaneous mitral valve repair for mitral regurgitation in high-risk patients: results of the EVEREST II study. J Am Coll Cardiol 2014;64:172-81. [PubMed]
- George I, Nazif TM, Kalesan B, et al. Feasibility and early safety of single-stage hybrid coronary intervention and valvular cardiac surgery. Ann Thorac Surg 2015;99:2032-7. [PubMed]
- Santana O, Funk M, Zamora C, et al. Staged percutaneous coronary intervention and minimally invasive valve surgery: results of a hybrid approach to concomitant coronary and valvular disease. J Thorac Cardiovasc Surg 2012;144:634-9. [PubMed]
- Ranucci M, Ballotta A, Agnelli B, Frigiola A, Menicanti L, Castelvecchio S. Acute kidney injury in patients undergoing cardiac surgery and coronary angiography on the same day. Ann Thorac Surg 2013;95:513-9. [PubMed]
- Kramer RS, Quinn RD, Groom RC, et al. Same admission cardiac catheterization and cardiac surgery: Is there an increased incidence of acute kidney injury? Ann Thorac Surg 2010;90:1418-23; discussion 1423-4. [PubMed]
- Berger JS, Frye CB, Harshaw Q, et al. Impact of clopidogrel in patients with acute coronary syndromes requiring coronary artery bypass surgery: a multicenter analysis. J Am Coll Cardiol 2008;52:1693-701. [PubMed]
- Fox KA, Mehta SR, Peters R, et al. Benefits and risks of the combination of clopidogrel and aspirin in patients undergoing surgical revascularization for non-ST-elevation acute coronary syndrome: the Clopidogrel in Unstable angina to prevent Recurrent ischemic Events (CURE) Trial. Circulation 2004;110:1202-8. [PubMed]





