Minimally invasive versus open thymectomy: a systematic review of surgical techniques, patient demographics, and perioperative outcomes
Abstract
Background: Thymectomy is the mainstay of treatment for thymoma and other anterior mediastinal tumors, and is often utilized in the management of patients with myasthenia gravis (MG). While traditionally approached through a median sternotomy, minimally invasive approaches to thymectomy have increasingly emerged. The present systematic review was conducted to compare perioperative and clinical outcomes following minimally invasive thymectomy (MIT) and open thymectomy (OT).
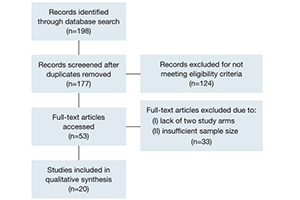
Methods: Articles were obtained through a PubMed literature search. Comparative studies reporting clinical outcomes following MIT and OT were eligible for inclusion. We selected studies with full text availability, written in the English language, published after 2005 and with at least 15 patients in each arm. A descriptive analysis was performed.
Results: Twenty studies were included, involving a total of 2,068 patients undergoing either MIT (n=838) or OT (n=1,230). Within individual studies, MIT and OT cohorts were well matched with regards to patient age and gender, but there was considerable variation across studies. Resected thymomas were consistently larger in OT groups, with mean diameter significantly larger in five studies (MIT, 29–52 mm; OT, 31–77 mm). MIT was consistently associated with a lower estimated blood loss (MIT, 20–200 mL; OT, 86–466 mL), chest tube duration (MIT, 1.3–4.1 days; OT, 2.4–5.3 days), and hospital length of stay (MIT, 1–10.6 days; OT, 4–14.6 days). There were no consistent differences in rates of perioperative complications, thymoma recurrence, MG complete stable remission, or 5-year survival.
Conclusions: In appropriately selected patients, MIT may reduce blood loss, chest tube duration, and hospital length of stay, with comparable clinical outcomes compared to OT via median sternotomy.
Cover