Video-assisted thoracoscopic thymectomy using 5-mm ports and carbon dioxide insufflation
Introduction
The preferred approach for thymectomy has traditionally been a sternotomy. Since the introduction of video assisted thoracoscopic surgery (VATS) thymectomy in the beginning of the 1990s (1), a minimally invasive approach to thymectomy for myasthenia gravis and early stage thymomas has gained widespread popularity. Several minimally invasive approaches to thymectomy have been described; VATS thymectomy from the right side, VATS thymectomy from the left side, bilateral VATS thymectomy (2), cervical thymectomy, subxiphoidal thymectomy (3), uniportal thymectomy (4) and robotic thymectomy (5). The potential benefits of a minimally invasive approach includes better cosmetic results, less postoperative pain, shorter length of stay, earlier return to daily activities, less bleeding and fewer complications overall with similar outcomes for survival, recurrence rate of thymoma and complete remission (CR) for myasthenia gravis (6-8).
Indication
This approach is applicable for patients with myasthenia gravis and/or thymomas up to 5 cm in diameter in clinical Masoaka Koga stage 1 (9). Either the left or right side can be used with this approach. The right side is preferred since there is a wider intrapleural space than on the left side, where the heart occupies space. Localizing the innominate vein is also easier on the right side, where it fuses with the superior vena cava. The phrenic nerve is localized more posteriorly on the left side, however, and it can be challenging to localize it from the right side. If the thymoma is located on the left-side close to the left phrenic nerve or the aorta-pulmonary window, a left sided approach is therefore preferred. Evidence of unilateral adhesions due to previous thoracic surgery may also influence the choice of side. If a bilateral approach is needed, an additional 5 mm port on the contralateral side can be added. If the thymoma is located high in the neck, the addition of a cervical incision may be necessary.
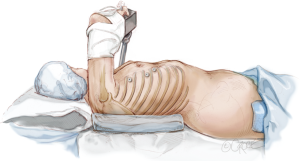
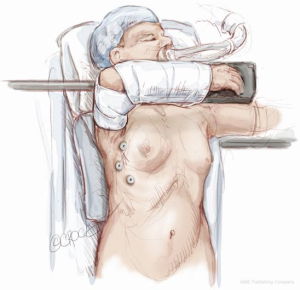
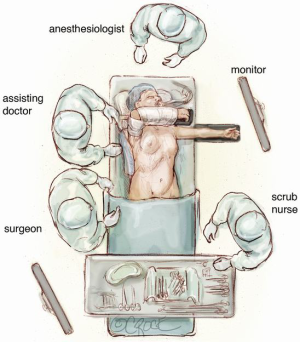
Positioning
The procedure is performed under general anesthesia with the patient monitored through an arterial line, and using double-lumen endotracheal intubation and contralateral one-lung ventilation. The patient is placed in the supine position with a 30-degree retroversion (Figure 1). The ipsilateral arm is placed over the head of the patient in a holder. Care should be taken to not overextend the shoulder, and thus avoid injury to the brachial plexus (Figure 2). The surgeon and the assistant stand on the ipsilateral side of the patient while the scrub nurse stands on the opposite site, using a separate monitor (Figure 3). A sternotomy tray is always ready in the operating theatre for a potential conversion.
Port placement
Three 5-mm ports (Versaport, Covidien) along the lateral border of the breast gland are used. The first port is created with a 5-mm skin incision. A dissector is introduced using blunt dissection along the upper edge of the sixth intercostal space in the mid-axillary line in order to create a pneumothorax. A 5-mm port with a trocar is then introduced into the same incision and a 5-mm, 30-degree thoracoscope (Endoye, Olympus) is used for inspecting the thoracic cavity for potential adhesions and pathology. Carbon dioxide (CO2) insufflation is installed using a pressure limit of 6–8 mmHg. Under thoracoscopic guidance, a second 5-mm port is bluntly introduced using a trocar into the anterior axillary line in the third intercostal space and a third 5-mm port placed in the midclavicular line into the sixth or seventh intercostal space. This latter incision is expanded at the end of procedure to 1–3 cm according to the size of the specimen to be resected.
Surgical steps
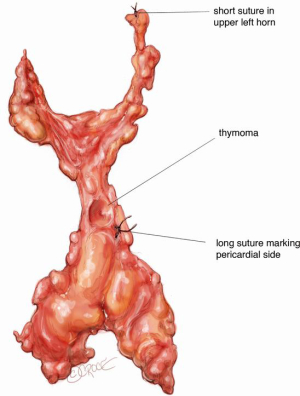
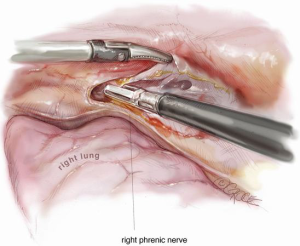
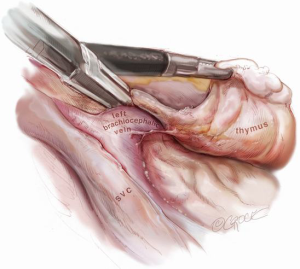
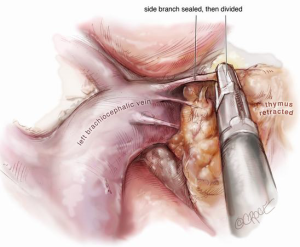
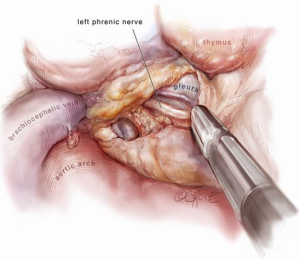
The entire thymic gland, including the two upper and two lower horns and all the fatty tissue in the anterior mediastinum, is excised in an “en bloc” fashion without touching the thymoma according to the recommendations from the International Thymic Malignancy Interest Group (ITMIG) (10). Dissection is performed using a bipolar energy device (LigaSure 5 mm, 35 cm, Covidien) in a clockwise direction on the right side and an anticlockwise direction on the left side. A roticulating crasper (Endo Crasp, Covidien) and 5 mm endopeanuts (Endopeanut, Covidien) are used for retraction. On the right side, the right lower horn is dissected along the right phrenic nerve, the pericardium and sternum (Figure 4). The dissection is then continued along the right phrenic nerve until the right mammary vein is reached. Continuing the dissection along the superior vena cava until its point of fusion with the innominate vein makes the localization of the latter structure easier on the right side easier than on the left (Figure 5). The right upper cervical horn is isolated, and while retracting the thymic gland inferiorly, the thyrothymic ligament is divided with LigaSure. The dissection is then continued along and above the innominate vein including all thymic and fatty tissue. Side branches to the innominate vein are divided with LigaSure, using a “double sealing technique”. In this sealing technique, the proximal end near the innominate vein is sealed with LigaSure, but not cut. Sealing and cutting is then performed distal to this point. A hemoclip can be applied, but is rarely needed. The left upper horn is dissected in the same way as the right upper horn and the thymic vein is divided with LigaSure (Figure 6). The pleura on the left side is localized and by continuing the dissection posteriorly, the left phrenic nerve can be visualized (Figure 7). The dissection is continued inferiorly along the left phrenic nerve while the gland is retracted to the right, and extended along the pleura and pericardium in order to remove the remaining part of the gland and fatty tissue, including the left inferior horn. The pleura on the left side are kept intact for as long as possible to prevent the left lung from occupying operating space. After completing the dissection, the orientation of the specimen is noted. CO2 insufflation is stopped and the lower 5 mm port is expanded to 1–3 cm according to the size of the specimen. An endobag (LaproSurge) is then introduced into the right thoracic cavity, where there is space and the specimen is grasped and placed into the bag. While extracting a thymoma of the thoracic cavity in an endobag, care should be taken not to squeeze the capsule. The specimen is marked with sutures and a drawing is made according to the recommendations from ITMIG (11) (Figure 8). Then the specimen is sent for pathology. The two 5 mm incisions are closed using only one suture in the skin. A CH18 chest drain is introduced in lower port and this incision is sutured in three layers using Vicryl 2-0.
Pain management and postoperative care
For pain management, an opioid-sparing multimodal analgesic regimen is used as previously described for VATS lobectomies (12), and consists of paracetamol (1 g + 1 g + 1 g + 1 g), slow-release ibuprofen (800 mg + 800 mg) and gabapentin (300 mg + 600 mg). At the beginning of the procedure, an intercostal block is applied for every port, using a total of 20 mL of bupivacaine (0.5%). An intercostal catheter is introduced sub-pleural into the posterior intercostal space of the lower port, using the Seldinger technique. The catheter is connected to an epidural pump with continuous infusion of 6 mL of bupivacaine/hour (0.25%). Removal of the catheter is usually performed together with chest drain removal. After extubation, the patient is transferred to a recovery room and observed for two hours, and then moved to the ward and mobilized according to enhanced recovery criteria. Usually, the chest drain can be removed the following morning, and if X-ray is acceptable and pain management is sufficient, the patient is sent home. Patients are seen in the outpatient clinic two weeks after surgery.
Discussion
The potential advantages of this approach compared to sternotomy include better cosmesis, less postoperative pain, shorter length of stay, earlier return to daily activities, less bleeding and fewer complications (6-8). Whether there is any difference in outcome between the many different minimal invasive approaches to thymectomy is unclear and remains to be investigated. The use of 5 mm ports and a 5-mm camera may potentially include less pressure on the intercostal nerve and thus less postoperative pain and possibly less chronic pain. A CH18 chest drain is used for the same reason, accepting that this size may not adequately drain a potential hemothorax, and in this case, another chest drain may be needed. CO2 insufflation is used to compress the ipsilateral lung and mediastinum, providing great space over the innominate vein and making the dissection of the innominate vein and cervical horns safer. Patients with a comprised cardiac output may not tolerate CO2 insufflation. In such cases, the pressure can be reduced or CO2 can be used intermittently for the crucial dissection in the neck. Bipolar electrocoagulation with LigaSure has less lateral thermal spread than monopolar electrocoagulation, allowing for safer dissection along the phrenic nerve and greater vessels. Ultrasonic devices can also be used for dissection, but one should be aware about the heat spread from the active plate.
A potential aspect for further development of the technique could involve introducing a subxiphoidal incision for thymomas that are over 5 cm in diameter, thus avoiding compression of the intercostal nerve when extracting these larger tumors from the thoracic cavity.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author is a Speaker for Medtronic, Ethicon, Medela and Takeda.
References
- Landreneau RJ, Dowling RD, Castillo WM, et al. Thoracoscopic resection of an anterior mediastinal tumor. Ann Thorac Surg 1992;54:142-4. [PubMed]
- Liu Z, Yang J, Lin L, et al. Unilateral video-assisted thoracoscopic extended thymectomy offers long-term outcomes equivalent to that of the bilateral approach in the treatment of non-thymomatous myasthenia gravis. Interact Cardiovasc Thorac Surg 2015;21:610-5. [PubMed]
- Zielinski M, Czajkowski W, Gwozdz P, et al. Resection of thymomas with use of the new minimally-invasive technique of extended thymectomy performed through the subxiphoid-right video-thoracoscopic approach with double elevation of the sternum. Eur J Cardiothorac Surg 2013;44:e113-9; discussion e119.
- Wu CF, Gonzalez-Rivas D, Wen CT, et al. Single-port video-assisted thoracoscopic mediastinal tumour resection. Interact Cardiovasc Thorac Surg 2015;21:644-9. [PubMed]
- Rueckert J, Swierzy M, Badakhshi H, et al. Robotic-assisted thymectomy: surgical procedure and results. Thorac Cardiovasc Surg 2015;63:194-200. [PubMed]
- Yuan ZY, Cheng GY, Sun KL, et al. Comparative study of video-assisted thoracic surgery versus open thymectomy for thymoma in one single center. J Thorac Dis 2014;6:726-33. [PubMed]
- Ye B, Tantai JC, Ge XX, et al. Surgical techniques for early-stage thymoma: video-assisted thoracoscopic thymectomy versus transsternal thymectomy. J Thorac Cardiovasc Surg 2014;147:1599-603. [PubMed]
- Jurado J, Javidfar J, Newmark A, et al. Minimally invasive thymectomy and open thymectomy: outcome analysis of 263 patients. Ann Thorac Surg 2012;94:974-81; discussion 981-2. [PubMed]
- Koga K, Matsuno Y, Noguchi M, et al. A review of 79 thymomas: modification of staging system and reappraisal of conventional division into invasive and non-invasive thymoma. Pathol Int 1994;44:359-67. [PubMed]
- Toker A, Sonett J, Zielinski M, et al. Standard terms, definitions, and policies for minimally invasive resection of thymoma. J Thorac Oncol 2011;6:S1739-42. [PubMed]
- Detterbeck FC, Moran C, Huang J, et al. Which way is up? Policies and procedures for surgeons and pathologists regarding resection specimens of thymic malignancy. J Thorac Oncol 2011;6:S1730-8. [PubMed]
- Wildgaard K, Petersen RH, Hansen HJ, et al. Multimodal analgesic treatment in video-assisted thoracic surgery lobectomy using an intraoperative intercostal catheter. Eur J Cardiothorac Surg 2012;41:1072-7. [PubMed]