The transition to uniportal robotic surgery in the second decade of uniportal surgery
Introduction
In the last decade, uniportal video-assisted thoracoscopic surgery (VATS) has become the primary method of performing minimally invasive thoracic surgery in large parts of the world (1). This has enabled access to minimally invasive surgery for surgeons from a large number of countries without the use of complex equipment. Patients worldwide now have available to them less invasive surgery with the benefits of reduced pain, quicker recovery, and for those patients with higher comorbidities, the opportunity to undergo surgery.
However, in high resource countries, many surgeons prefer to use robotic surgery to perform thoracic surgery, as they have access to robotic platforms and patients find the concept attractive. Although the operations are similar to VATS in terms of quality of surgery, lymph node harvest and recovery times, advocates of robotic surgery point to the benefits of additional dexterity available for complex cases, ease of use, and ability to train others with dual console training and advanced simulation.
Diego Gonzalez-Rivas, the creator of uniportal VATS, by necessity after COVID had to spend more time in Spain but used this time to investigate the possibilities of robotic surgery (2). He paired up with a cardiac robotic surgeon to watch and understand the benefits of robotic surgery, but the fact remained that these advantages had to be counterbalanced by the fact that five incisions were required compared to a single incision in uniportal VATS (3).
Thus, he sought to apply robotic surgery to the uniportal incision which evolved into the first cases of uniportal robotic surgery in September 2021 and a rapid evolution and learning curve of this technique that is the subject of this edition of the Annals of Cardiothoracic Surgery.
In this article, we will discuss some of the technical elements of adopting uniportal robotic surgery in order to guide surgeons interested in adopting this technique into their practice.
However, unlike other robotic techniques, uniportal robotic surgery is currently off-label and therefore support will not be available from Intuitive, the current market leader in robotic surgery. This will no doubt change with time as the technique establishes itself and other manufacturers come onto the market. In this article, I will also explain the rationale behind the reason that it is off label and then we will give some advice as to how to work around this fact.
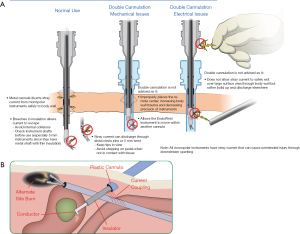
Capacitive coupling
Many surgeons are not aware of capacitive coupling which is not unique or specific to da Vinci Robotic Surgery. It has been a significant engineering problem since the beginning of laparoscopic surgery with the combined use of monopolar energy through plastic trocars or any type of insulating material at the body wall such as wound retractors.
This was highlighted by Tucker et al. in 1992 (1) who demonstrated currents as high as 25 watts being discharged into tissue outside of the view of the endoscope.
The problem of capacitive coupling occurs whenever a surgeon places a metal cannula through a plastic trocar or a plastic access port, such as an Alexis port, or through an open incision or an area such as the mouth in ear, nose and throat (ENT) surgery, where the cannulae do not touch soft tissue. The plastic trocar or air acts as an insulator and capacitive charge is then allowed to build up on the cannula when monopolar current passes down any instrument that is in that trocar.
Let’s take a quick step back to remind ourselves of what a capacitor is. A capacitor is in fact one of the simplest electrical devices that exists. They were discovered in 1740 when they were used to store static electricity simply by placing two metals close to each other but separated by an insulator. Flow of electrons in one metal induced a build-up of charge in the other metal that could be stored as it was unable to be discharged due to its insulation. This allowed a powerful spark to be discharged on demand. Allesandro Volta then used capacitors in 1782 to create the first batteries.
When we have a monopolar instrument, such as a hook diathermy, it is surrounded by a plastic insulator, but if you put it in a metal trocar, then you have unintentionally created a capacitor with charge passing down the hook diathermy. This induces a charge to build up on the metal on the other side, and in this case, it is the trocar. This is not an issue if the metal trocar is touching soft tissue, as this charge easily dissipates and thus does not build up. But if the trocar is then insulated from the soft tissue, then charge can build up on the trocar just like the early capacitors used to create sparks. The charge held in the trocar then remains even if the diathermy energy is stopped and is held in the metal of the trocar like a battery. If that trocar then touches something it can then discharge this energy. The danger arises when we consider what tissue can touch the trocar. If we touch a metal forceps that is holding lung out of view, then the lung could suffer a diathermy burn. In abdominal surgery, manufacturers are very concerned with a loop of small bowel touching the trocar and causing a burn to the small bowel that would not be noticed until postoperatively when the patient could suffer a small bowel perforation or peritonitis, as a direct consequence of capacitive coupling.
So what do the companies do to mitigate this complication? Hubert Stein, Senior Director of Surgical Applications Engineering at Intuitive who explained capacitive coupling to me, tells me that Intuitive surgical have designed the TORS (transoral robotic surgery) Trocars for ENT surgery to have an attachment at the side to dissipate any energy built up in the trocar by earthing it. And in the Single Port (SP) Intuitive system, the electrosurgical unit has been designed to monitor the trocars for electrical build-up, and to look for energy leakage and address it if this occurs.
Mitigation of the risks of capacitive coupling
Firstly, bipolar diathermy use does not have this issue and therefore the easiest way to mitigate the risks of capacitative coupling is to simply use the Maryland bipolar forceps or the fenestrated bipolar forceps in uniportal robotic surgery. If you do want to use monopolar energy, such as the spatula or hook diathermy, then you should make your team aware of this issue. In thoracic surgery, the trocars are unlikely to be able to directly touch any organs other than the lungs. Furthermore, lung graspers or metal suckers that could contact the trocars are likely to be in view, so keep them in view as much as possible so the lung parenchyma can be observed for any issues. If further actions were desired to mitigate the risk, then the TORS trocars could be used and earthed as they are in ENT surgery. In reality, this issue does not seem to be causing any harm in thoracic surgery, but awareness is important as it on this basis that this use of the da Vinci Surgical system remains off-label when used uniportally, which is the reason that surgeons are unable to receive assistance in uniportal robotic training from the company or support for their cases (Figure 1A,1B).
Starting uniportal robotic surgery
For units that do not have an established multiportal robotic program in thoracic surgery, you must commence your robotic journey by first being fully proctored in multiportal robotic surgery with the full support of Intuitive. The Intuitive training program has been developed over 20 years and has trained over 55,000 surgeons worldwide. It begins with 30 hours of simulator training, then uses wet lab and dry lab training with thoracic surgical proctors, and then brings a proctor to come to perform your first operation with you in your hospital. Thereafter, there are a series of courses to increase your knowledge and skills and in thoracic surgery. These use the excellent KindHeart beating heart pig model to teach advanced thoracic skills such as segmentectomy and sleeve resection. This training will enable the surgeon to be fully conversant with the robotic platform, and understand the use of the arms, port placement, stapling and the flow of robotic lobectomy, and allow the full team to be skilled in robotic set up. Of note, robotic surgery is a team approach and it is key to have the full team trained in set up, instrument management, error handling and anesthesia. I would personally recommend that teams perform around 100 robotic thoracic operations before considering a uniportal robotic surgery as an option, although this will vary according to individual skills and hospital set up.
For established multiportal robotic programs, it is of some advantage if the surgeon and especially the assistant has some experience in uniportal VATS, even if this is just for more minor operations. Consider performing minor operations such as bullectomies, pleural biopsies and empyema surgery uniportally prior to embarking on a uniportal robotic program. But other than this recommendation, any established multiportal robotic program can easily consider doing some cases uniportally with their robotic platform. As a first step, it is advisable to engage with your whole team and review the proposal to perform uniportal robotic surgery with the team and gain consent of the hospital to perform uniportal surgery with an off-label indication for the Intuitive system.
Case selection
When learning new procedures, it is important to select appropriate cases for the first few patients and make sure that there are good conversion options available for the patient. The ideal case to begin in thoracic surgery is always wedge resections (most commonly for metastases) with an indication to perform a lymphadenectomy. The reason for this is that that most important part of the operation, which is the wedge resection, can be completed early in the procedure and then a full lymphadenectomy, which may easily be justified, can allow the surgeon to test the technique around the whole thoracic cavity, allowing the lung to be moved into all four quadrants and to work from the inferior pulmonary ligament, posteriorly with station seven, anteriorly with the upper lobe vein and anterior hilar lymph nodes, and superiorly with the superior mediastinal lymph nodes. Any limitations of movements or time pressures can then either allow conversion to multiportal robotics or cessation of the operation without detriment to the patient. It is important to do a handful of these cases to understand how to avoid clashing, the use of the stapler and the placement of the single incision.
Port placement
A key part of uniportal robotic surgery is the understanding of placement of this incision. It is usually at the sixth intercostal space for an upper lobectomy and the seventh space for a lower lobectomy. It is also a little more posterior than the usual uniportal VATS incision as the endoscope looks 30 degrees down on the hilum and thus needs to be around the anterior axillary line. It is important to get a feel for optimal port placement in some minor cases before proceeding to lobectomies, as a good port placement greatly facilitates the operation.
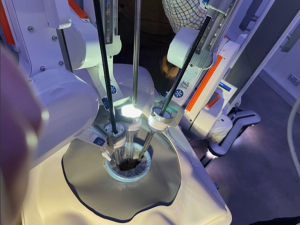
The ports
It may be tempting to start with three ×8 mm Intuitive ports, but this is a mistake as it will cause a surgeon inexperienced in uniportal robotic surgery significant problems with clashing/collision of the arms. It is far preferable to wait until you have access to two TORS ports as this will help you understand how to avoid this problem. You can then place one 8 mm Intuitive trocar between two TORS ports, without the CO2 seals attached, and a 12 mm port to exchange for stapling. This is the optimal set up and is in fact superior to three TORS ports with the ground modules attached. Diego has successfully removed the grounding modules off a set of ports, but again this is an off-label modification to the ports and therefore you would need to check with your hospital before making this modification. If this modification is made, then three TORS ports are optimal. The endoscope is always in the posterior port in a 30 degrees downward configuration, unless there are adhesions. The middle port is used for the instrument that will be most cranial, then the most anterior port is used for the most caudal instrument. Instruments will then need to be assigned manually on the surgeon’s console before starting the procedure.
Instruments
For a variety of reasons, we would most strongly recommend a Maryland bipolar forceps in the dominant hand and a bipolar fenestrated forceps in the non-dominant hand. This allows bipolar energy safely from both hands, and is the most versatile configuration, also allowing grasping and the safe passage of instruments around vessels. The spatula or hook is another option, but the aforementioned risks of capacitive coupling exist and the whole case cannot be performed with either a hook or spatula and a bipolar forceps, thus attracting additional costs.
It may be tempting to recommend that the assistant perform stapling, but it is preferable to use the Intuitive stapler from the first case. Some experience is needed in the exchange of the 8 mm port for the 12 mm port and the set-up of this port to help the surgeon to perform consistent stapling. We recommend looking down the 12 mm port to line it up on the structure to be stapled, then make sure the remote center is 2–3 cm out of the incision so that the articulation of the stapler is not an issue.
The assistant
It cannot be emphasized enough that the assistant is key to the success of the operation. Ensuring that the ports are separated as much as possible in the uniportal incision and that the remote centers are at the appropriate depth is important. Ensuring that the Xi is orientated directly vertically with 20 cm between arms and that the clearance controls are optimized is also important. But more so is experience in knowing when to introduce the long metal curved sucker to retract for the surgeon or when to leave the surgeon to perform two handed surgery. Of note, obtaining a long metal curved sucker for the first operation is key, as this maximizes the success of the first few cases, and a shorter sucker or one without a curve will completely inhibit the assistant’s ability to assist. The assistant must be conversant with swapping the 8 mm trocar with the 12 mm stapling trocar (without the CO2 cap) and then positioning it for stapling. If the angle for the stapler is incorrect, then the trocar should be repositioned.
Alternative platforms
There are currently a small number of other companies that are in the market. Cambridge Medical Robotics (CMR) has over 100 Versius systems in operation internationally. Its key advantage is its small size and its 5 mm arms, and it is in use in around five centers in thoracic surgery. I am a proctor for CMR, and I have made some attempts to try uniportal robotic surgery with it, but due to the novel way in which the instruments are held at their distal end, it is not suitable for uniportal surgery.
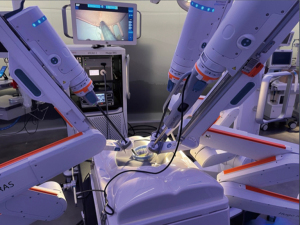
The Hugo System by Medtronic on the other hand, holds the instruments in a similar fashion to Intuitive (The Remote Centre of Motion or RCM method) and it has been tried in a dry lab situation and is thought to be suitable for uniportal robotic surgery (Figure 2). This will need to be confirmed in clinical trials. Other systems such as Avatera that use the remote center of motion method may also be suitable for uniportal Robotic surgery as they come on the market in thoracic surgery.
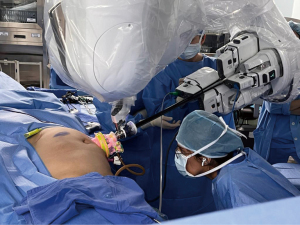
The SP Xi from Intuitive is a system designed for uniportal surgery. It is just undergoing Food and Drug Administration (FDA) approved clinical trials in uniportal thymectomy in the USA, and has been used in cadaveric laboratories and in limited clinical trials for lobectomy and does show some considerable promise. The limitation of a fixed 25 mm diameter single trocar with a need for the working zone to be more than 12 cm from the port has recently been overcome by the creation of a bespoke Alexis style Intuitive entry system that may well work very well in uniportal surgery, either from an intercostal incision or a subxiphoid incision (Figure 3). There is currently no Intuitive stapler to use with the system, and a bedside assistant still needs to perform the stapling. In addition, an SP system must be purchased in order to move to SP robotic surgery (Figure 4).
Conclusions
In the last decade, uniportal VATS grew from creation to the predominant method of surgery in thoracic surgery. Again, uniportal robotic surgery has been created at the commencement of this decade, and already only one year after its creation it has been used for advanced cases including segmentectomies and sleeve resections, thus it will be very interesting to see how it progresses over the coming years and as other robotic platforms become clinically available. We are at the dawn of the robotic era, and this is an exciting evolution of the technique of robotic surgery.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Tucker RD, Voyles CR, Silvis SE. Capacitive coupled stray currents during laparoscopic and endoscopic electrosurgical procedures. Biomed Instrum Technol 1992;26:303-11. [PubMed]
- Gonzalez D, Paradela M, Garcia J, et al. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5. [Crossref] [PubMed]
- Gonzalez-Rivas D, Bosinceanu M, Manolache V, et al. Uniportal fully robotic-assisted major pulmonary resections. Ann Cardiothorac Surg 2023;12:52-61. [Crossref] [PubMed]