Importance of the third arterial graft in multiple arterial grafting strategies
Coronary artery bypass grafting (CABG) using the bilateral internal thoracic arteries (ITAs) has been demonstrated to improve survival and reduce the recurrence of angina in comparison with a single ITA revascularisation.
When bilateral ITAs are anastomosed to the left coronary artery system, several grafts can be used for the right coronary system revascularization. Conduits considered acceptable to revascularize the right coronary artery (RCA) system include the saphenous vein graft (SVG), the free radial artery (RA) implanted into the aorta or into the left internal thoracic artery, the right internal thoracic artery (RITA) in situ or used in a Y graft configuration, and the right gastroepiploic artery (RGEA). The influence of the type of conduit implanted to the RCA system on clinical results remains unclear, and the complementary conduit of choice for this system has yet to be determined. No superior patency rate for any of these grafts to the RCA has been clearly established. The patency results of the RITA on the RCA have been reported lower than those obtained when used for the left coronary system. The patency rates of RA and RGEA are highly dependent on the degree of stenosis of the native vessel, and their use remains limited because of its association with a high risk of graft failure related to competitive flow.
Moreover, left and right coronary systems exhibit distinct physiological flow patterns and different patterns of atheromatous disease, which, for example, may account for poorer patency of an in situ RITA grafted to the RCA compared with a left-sided target. Therefore, selection of the optimal conduit for the RCA or its branches cannot simply be extrapolated from data arising from left-sided or mixed targets.
In view of these recent studies debating the potential benefit of an third arterial graft, we compared the very long term results of RGEA grafting with SVG grafting in the patients with bilateral ITA grafting to the left coronary system.
Methods
Between July 1985 and November 1995, 2,940 patients underwent a surgical revascularization in our department. We compared the outcomes of patients undergoing bilateral ITA (BITA) revascularisation with either a RGEA (group I) or a SVG (group II).
Preoperative patient characteristics are shown in Table 1. Overall survival constituted the primary end point studied. The secondary end point was freedom from cardiac death.
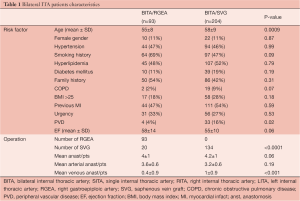
Full table
Statistical analysis
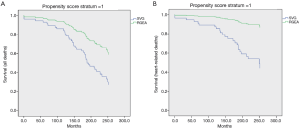
To deal with non-comparability of groups of patients receiving either surgery in this observational study, we used a 3-step analytical strategy. Univariate and multivariate Cox proportional hazard regression analyses were performed for the analysis of late mortality and cardiac events. Survival and event-free survival curves were estimated using the Kaplan-Meier method and differences between groups were compared using the log-rank test. A propensity score was calculated for GEA or SVG grafting to obtain relatively homogeneous subgroups i.e. with similar clinical characteristics. The Kaplan-Meier method was used to display the survival curves for each stratum (Figure 1).
Results
Eighty-six percent of the cohort was male and had an average of 59±9 years. Mean follow-up was 16.1±5.4 years. Mean postoperative follow-up in the group I and group II was 16±5.4 and 16.4±6.2 years respectively. One hundred and sixty patients were followed for more than 20 years after operation.
First step analysis: multivariate Cox proportional hazard regression analysis
The addition of a RGEA to BITA grafting influenced significantly the overall survival (HR, 0.46, 95% CI: 0.25-0.86, P=0.015) compared to a SVG. Other significant predictors included ejection fraction (HR, 0.97, 95% CI: 0.96-0.99, P=0.007), age (HR, 1.05, 95% CI: 1.03-1.08, P<0.0001) and peripheral vascular disease status (HR, 2.2, 95% CI: 1.3-3.6, P=0.001). Cardiac death was also significantly influenced by the presence of a RGEA compared with a SVG (HR, 0.2, 95% CI: 0.06- 0.6, P=0.009), as well as HTA (HR, 2.1, 95% CI: 1.08-4.1, P=0.02), polyvascular disease (HR, 2.7, 95% CI: 1.3-5.27, P=0.003) and ejection fraction (HR, 0.97, 95% CI: 0.94-1, P=0.04).
Second step analysis: Cox proportional hazard regression analysis using propensity score strata (Table 2)
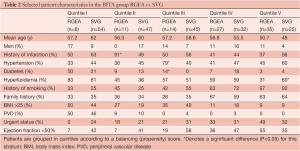
Full table
RGEA did significantly influence the overall survival (HR, 0.41, 95% CI: 0.22-0.74, P=0.0032). In complementary analyses for unbalanced risk factors, only history of myocardial infarction was significant, with little change in HR for RGEA vs. SVG. Cardiac deaths were significantly lower in RGEA compared to SVG grafting (HR, 0.18, 95% CI: 0.05-0.58, P=0.004). In complementary analyses for unbalanced risk factors, only history of arterial hypertension was significant, with little change in hazard ratio for RGEA vs. SVG.
Discussion
We found that the addition of a third arterial graft to the 2 ITA as a clear benefit over the classical saphenous vein in terms overall survival and cardiac survival. The suitable arterial grafts to target the RCA are the RA, the RGEA, and the RITA.
Suzuki and colleagues compared the revascularization with a SVG vs. the RGEA to the RCA (1). They found that at 7 year the freedom from death from all causes was 96% for the RGEA and 82% for the SVG and that the rate of freedom from cardiac events was 89% for the RGEA and 77% for the SVG. In a multivariate analysis they found that SVG use was an independent predictor’s of late cardiac event.
Di Mauro and colleagues (2), in a retrospective study found at 8 years freedom from cardiac death significantly higher when saphenous vein was used compared to RGEA grafting (94% with RGEA vs. 98% with SVG). They concluded that supplementary venous grafts seem to provide more stability than gastroepiploic artery, which may even impair long-term outcome.
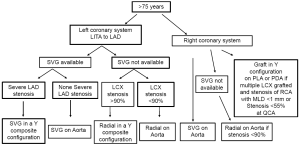
The absence of clear benefit of RGEA grafting is likely primarily due to the very high degree of flow competition with the RGEA artery leading to first graft dysfunction and finally to graft occlusion. We have focused our interest on the impact of the severity of the RCA lesion and its correlation to graft dysfunction (3). We found that a minimum lumen diameter measured by quantitative coronary angiography analysis above 1 mm predicts an unfavorable flow pattern and poor functionality in RGEA used in a composite fashion, but not in SVG. Several factors could contribute to the greater predictive value of RCA stenosis severity on the flow pattern of RGEA. Compared with a SVG which is directly anastomosed to the ascending aorta and can be considered as a first branch off of the aorta, the in situ RGEA is the fourth branch originating from a visceral system. This more distal origin from a complex branching arterial system combined with a lumen diameter that is usually smaller than that of venous grafts, may contribute to a lower flow capacity of RGEA compared to SVG.
An alternative strategy for arterial grafting to the RCA is use of a radial artery. Hirose and colleagues (4) have compared the use of a radial artery versus the RGEA in adjunction of the 2 ITA’s. They found after a follow-up of 2.3 years, that the event-free rates as well as the survival rates were not significantly different between the 2 groups. The RA can be used to bypass a variety of coronary arteries, whereas the GEA can be used only for revascularization of the RCA because of the limited length of the in situ graft. In situ GEA grafting or composite RA grafting should be chosen for patients with a calcified aorta.
Another attractive possibility is to use the right ITA in a composite Y graft configuration to revascularize the whole coronary system with the use of only 2 ITAs. However, the RITA used in a Y configuration has an increased risk of competitive flow compared with the in situ graft (5). The mechanism of competitive flow is more complex than that in the individual graft in which the interaction is only between the proximal inflow and the distal anastomosis outflow. In such sequential composite bypass, the interaction is also between all the anastomosed branches within the composite graft. This leads to a phasic delay between the pressure wave in the grafts, and in the coronary arteries, especially in the more distal ones such as the right coronary artery.
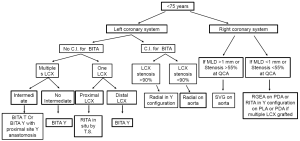
In a prospective randomized trial we have demonstrated that the functionality of the RITA graft targeted to the PDA is significantly affected by the RCA lesion characteristics (6). A minimum lumen diameter of the stenosis above 1.1 mm predict an unfavorable flow pattern and poor functionality in RITA used in a composite fashion, but not in SVG. We have recommended that in stenosis of intermediate severity [minimum lumen diameter (MLD) >1.1 mm] the SVG should be used preferentially to graft the RCA system. However, when the preoperative MLD is below a threshold of 1.1 mm a RITA could be used in a composite fashion with good result. Therefore we have modified our grafting strategy (Figures 2,3). The use of a third arterial conduit targeted to the RCA should be considered to improve long-term survival.
Acknowledgements
Disclosure: The author declares no conflict of interest.
References
- Suzuki T, Asai T, Matsubayashi K, et al. In off-pump surgery, skeletonized gastroepiploic artery is superior to saphenous vein in patients with bilateral internal thoracic arterial grafts. Ann Thorac Surg 2011;91:1159-64. [PubMed]
- Di Mauro M, Contini M, Iacò AL, et al. Bilateral internal thoracic artery on the left side: a propensity score-matched study of impact of the third conduit on the right side. J Thorac Cardiovasc Surg 2009;137:869-74. [PubMed]
- Glineur D, D’hoore W, El Khoury G, et al. Angiographic predictors of 6-month patency of bypass grafts implanted to the right coronary artery a prospective randomized comparison of gastroepiploic artery and saphenous vein grafts. J Am Coll Cardiol 2008;51:120-5. [PubMed]
- Hirose H, Amano A, Takahashi A. Triple arterial coronary revascularization using the radial artery and bilateral internal mammary arteries versus the gastroepiploic artery and bilateral internal mammary arteries. Circ J 2002;66:544-8. [PubMed]
- Glineur D, Hanet C, D’hoore W, et al. Causes of non-functioning right internal mammary used in a Y-graft configuration: insight from a 6-month systematic angiographic trial. Eur J Cardiothorac Surg 2009;36:129-35; discussion 135-6. [PubMed]
- Glineur D, D’hoore W, de Kerchove L, et al. Angiographic predictors of 3-year patency of bypass grafts implanted on the right coronary artery system: a prospective randomized comparison of gastroepiploic artery, saphenous vein, and right internal thoracic artery grafts. J Thorac Cardiovasc Surg 2011;142:980-8. [PubMed]





