Transapical aortic valve implantation in the presence of a mitral prosthesis
Introduction
Transcatheter aortic valve implantation (TAVI), using the Edwards Sapien balloon expandable valve (Edwards Lifesciences, Irvine, California, USA) has expanded our ability to treat patients with symptomatic severe aortic stenosis, and become the treatment of the choice in high risk inoperable patients (1,2). Further inroads into its application in subgroup populations, such as patients with a functioning mitral valve prosthesis, has also been defined over recent years. With experience, these patients now need not be uniformly excluded (3). Our case series have demonstrated that the transapical TAVI of a balloon expandable valve is feasible and safe in patients with both mechanical and bioprosthetic mitral prostheses. Technical challenges however exist in patients with mitral bioprostheses (3). The understanding of the interaction between both prostheses at the anatomic aorto-mitral continuity is critical for patient selection, and procedural modification to ensure success.
Pitfalls
Different mechanical valves have rigid housing cages with varying height and variable degrees of pivot guard protrusion. The techniques of mitral valve implantation can also affect the degree of prosthetic protrusion into the left ventricular outflow tract (LVOT). An everting suture technique leaves the mitral prosthesis sited below the mitral annulus, with resultant prominence of the rigid housing cage and/or pivot guard within the LVOT. Echocardiography is useful in identifying ‘unfavorable’ characteristics that should raise alarm. Bioprostheses have more prominent commissural struts and invariably impinge on the LVOT. Therefore, the ‘high risk’ patient for TAVI has either a bioprosthetic mitral valve, or a mechanical valve with its rigid housing cage in close proximity to the aortic annulus within the LVOT.
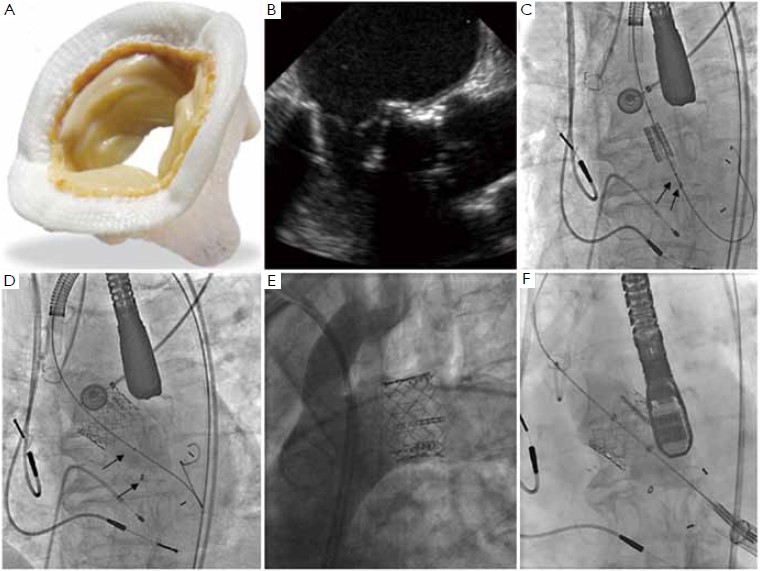
Valve maldeployment and embolization occurs principally when the inflating balloon impinges onto the adjacent mitral prosthesis: specifically, the prosthetic housing cage and pivot guard (mechanical valve), or the commissural struts (bioprosthesis). This impingement of the balloon propels it along with the mounted valve in the ‘aortic’ direction (Figure 1A, B, C, D, E). The “high risk” patients should not be treated using the transfemoral approach. The transapical approach is safe with good outcomes in patients with mitral prostheses (3) (Figure 1F). The shorter access site-balloon distance and the coaxial alignment allow the operator to firmly stabilize both the delivery sheath and catheter, and to promptly react to restrain the valve from ‘aortic’ displacement should this occur.
Operative technique
The standard transapical TAVI procedure is performed through a left anterolateral mini-thoracotomy (4-6). The radiolucent soft tissue retractor is preferable to avoid cluttering of the imaging field and to minimize postoperative pain. Transesophageal echocardiography reconfirms the aortic annular size, and the degree of mitral prosthetic impingement into the LVOT. Rapid epicardial ventricular pacing (~180 beats per minute) during balloon valvuloplasty and valve deployment are routine.
Balloon valvuloplasty (BAV) using the ASCENDRA kit balloon (3 cm balloon length) or equivalent, is a mandatory pre-implantation rehearsal because balloon shifts during valvuloplasty forewarn of potential valve maledeployment and embolization. Observations during BAV include: (I) the extent of balloon impingement onto the mechanical mitral prosthetic cage or bioprosthetic commissural strut, and (II) the degree of balloon displacement during inflation. Occasionally immobilization of a mechanical leaflet can be seen during BAV. This however is only transient and does not impact on subsequent mitral prosthetic function post-TAVI.
Our initial experience has defined the following procedural modifications for the Sapien valve implantation in patients with an existing mitral prosthesis, particularly a bioprosthesis.
I. The Sapien valve is positioned more ventricular (50- 60% of the stent in LVOT) in anticipation of a minimal ‘aortic’ shift, and even more ventricular (60% of stent in LVOT) when massive balloon shift is observed during BAV in patients with mitral bioprostheses.
II. The operator should firmly hold both the delivery sheath (right hand) and valved-balloon catheter (left hand), maintaining both the sheath position and direction at the apex of the heart. Active pulling of the valve back at the earliest sign of balloon shift may be required. However, beware that the inappropriate “pull-back” of the valve catheter can also cause valve maldeployment.
III. Slow balloon inflation during valve deployment minimizes displacement and allows an experienced operator to actively adjust the valve position.
IV. Aggressive valve oversizing may worsen deployment shifts. Redilatation for paravalvular leaks should be avoided because it may displace the valve, and overdilation of the outflow stent of the transcatheter valve aggravates transvalvular regurgitation.
Summary
Various degree of balloon displacement occur due to impingement on the housing cage and pivot guards of mechanical mitral valves, and on the bioprosthetic struts. The high-risk patients have either bioprosthetic mitral valves, or mechanical valve cages seated below the mitral annulus impinging onto the balloon during BAV. The transarterial approach should be avoided in these high-risk patients. The transapical approach with some technical modifications is safe, with good outcomes in patients with functioning mitral prostheses. TAVI in the presence of a mitral prosthesis, however, should be reserved for experienced centers.
Acknowledgements
Disclosure: Dr. J. Ye is consultant to Edwards Lifesciences, Irvine, USA.
References
- Kodali SK, Williams MR, Smith CR, et al. Two-year outcomes after transcatheter or surgical aortic-valve replacement. N Engl J Med 2012;366:1686-95.
- Makkar RR, Fontana GP, Jilaihawi H, et al. Transcatheter aortic-valve replacement for inoperable severe aortic stenosis. N Engl J Med 2012;366:1696-704.
- Soon JL, Ye J, Lichtenstein SV, et al. Transapical transcatheter aortic valve implantation in the presence of a mitral prosthesis. J Am Coll Cardiol 2011;58:715-21.
- Ye J, Cheung A, Lichtenstein SV, et al. Six-month outcome of transapical transcatheter aortic valve implantation in the initial seven patients. Eur J Cardiothorac Surg 2007;31:16-21.
- Ye J, Cheung A, Lichtenstein SV, et al. Transapical aortic valve implantation in humans. J Thorac Cardiovasc Surg 2006;131:1194-6.
- Wong DR, Ye J, Cheung A, et al. Technical considerations to avoid pitfalls during transapical aortic valve implantation. J Thorac Cardiovasc Surg 2010;140:196-202.