Management of malperfusion syndrome in acute type A aortic intramural hematoma
Abstract
Background: We report the outcomes of acute type A aortic intramural hematoma (ATAAIMH) with malperfusion treated with endovascular intervention and delayed open aortic repair.
Methods: Between April 1998 and April 2018, 644 patients were treated at our institution with an acute type A aortic dissection (ATAAD) or ATAAIMH, 82 (13%) had intramural hematomas (IMHs) including 12 (15%) with malperfusion syndrome (MPS) and 70 (85%) without MPS (no MPS). Data was obtained through medical record review, the Society of Thoracic Surgeons data elements, and the National Death Index database.
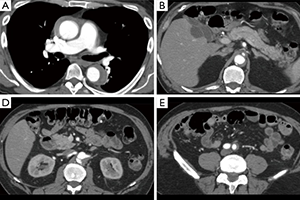
Results: Both MPS and No MPS groups had similar comorbidities including coronary artery disease, hypertension, diabetes, and peripheral vascular disease; however, those with MPS were sicker on admission with higher rates of acute renal failure (50% vs. 1%, P<0.0001) and acute paralysis (17% vs. 0%, P=0.02). Patients with MPS amenable to endovascular reperfusion (n=10) underwent endovascular fenestration/stenting and delayed aortic repair. Those with cerebral or coronary MPS (n=2) and those without MPS (n=70) underwent emergent open aortic repair. Of the ten patients undergoing fenestration/stenting, seven went on to aortic repair, one survived to discharge without aortic repair, one died from aortic rupture on hospital day 34, and one died from organ failure prior to aortic repair. Following endovascular fenestration/stenting or aortic repair, all patients with MPS had higher in-hospital mortality (17% vs. 0%), P=0.02. Following aortic repair, patients with MPS had more postoperative sepsis and longer postoperative length of stay (all P<0.05). However, both groups had a 0% operative mortality (including in-hospital and 30-day mortality following aortic repair). The 5-year survival of all ATAAIMH patients was 79%. The 2-year survival was significantly better in the No MPS group (94% vs. 62%, P=0.006).
Conclusions: ATAAIMH with MPS can be effectively managed with upfront endovascular fenestration/stenting followed by delayed aortic repair.
Cover