International E-vita open registry
Introduction
Following the introduction of the hybrid stent-graft “E-vita open” by our group in January 2005, and its successful implementation for routine one-stage repairs of complex thoracic aortic diseases, such as acute type I dissections, the International E-vita open registry (IEOR) was initiated in 2008 to study the principles of this treatment algorithm. The IEOR represents the first database to evaluate aortic disease after hybrid stent-grafts, and permits long-term follow-up of up to 8 years (1).
The hybrid stent-graft enables the surgical treatment of the ascending aorta, the arch, and the descending aorta within a single stage via a median sternotomy. As the descending aorta beyond the origin of the left subclavian artery is usually not accessible through a standard median sternotomy, a two-stage approach has been the norm for the past 30 years, although this has been associated with high perioperative and postoperative mortality (2-4).
Based on the evolutionary concept from Borst’s early elephant trunk technique, the stented distal portion of this hybrid graft sufficiently induces false lumen thrombosis to allow subsequent aortic remodelling in aortic dissections. Similarly, resolution of the non-perfused segment occurs after full exclusion of aneurysms. The graft should be slightly larger than the true lumen or distal neck diameter in dissection or aneurysmal disease.
The indications for applying this concept are (5):
- Acute type I dissection with an entry or re-entry tear at the distal arch and/or proximal descending aorta, or a full circumferential dissection at the distal arch level;
- Chronic type I dissection of distal ascending aorta, arch and descending aorta with fast growing aneurysmal configuration (>1 cm/year) and/or a diameter >6 cm, or true lumen collapse downstream with malperfusion symptoms;
- Retrograde type III dissection involving the arch with or without ascending aorta;
- Complex aneurysmal disease involving ascending aorta, arch and descending aorta.
The hybrid stent-graft is introduced during open aortic arch surgery, utilising hypothermic circulatory arrest and selective antegrade cerebral perfusion as neuroprotective mechanisms. The precise landing of the stented portion of the graft within the downstream aorta is facilitated by over-the-wire technique. Diseased sections can be avoided by direct angioscopic visualisation (6). After releasing the stented portion, a hemostatic suture-line between the intussuscepted arch prosthesis and the transected aortic arch is fashioned, followed by reimplantation of the head vessels into the arch graft through island or separate anastomotic techniques. Surgery is completed by anastomosing the arch prosthesis and the ascending aortic graft placed earlier (7,8).
To evaluate the efficacy of this treatment concept with regards to the durability of the repair, the need for subsequent secondary surgery or endovascular graft extension, the fate of the false lumen exclusion and remodelling of the aorta, as well as exclusion of aneurysms, the IEOR was established.
International E-vita open registry
Between January 2005 and October 2012, 416 patient datasets from 10 European centers were included in the IEOR database (Table 1).

Full table
Participation in the registry was voluntary, and was limited to high volume centres with experience in arch surgery. No specific guidelines were followed with regard to the operative protocols. While surgical strategies varied between institutions, bilateral selective cerebral perfusion during the hypothermic circulatory arrest was performed by all participating centres.
Acute dissection
138 patients in the registry presented with aortic dissection (121 acute type I and 17 acute type III dissection). The patients had a median age of 61 years and 81% underwent emergency surgery within 24 hours after onset of symptoms. According to the Penn classification, 48% of cases were class a, 24% class b, 8% class c and 20% class b+c. Additional surgical procedures included aortic valve replacement/repair, root replacement, and CABG in 40%. Operative times (mean ± SD) reflect the complexity of the treatment: the duration of cardiopulmonary bypass was 241±75 mins, cardioplegic cardiac arrest was 140±54 mins, and isolated bilateral selective cerebral perfusion was 68±30 mins. In-hospital mortality (beyond 30 days mortality) was 16%. The incidence of neurological events consisted of stroke in 7% and spinal cord injury (paraplegia or paraparesis) in 4%. Complete thrombosis of the false lumen along the stent-grafted descending aorta was achieved in 86% of patients postoperatively and documented in 92% at last follow-up. Within the discharged patient population, the survival rate after 5 years was 79%. Freedom from secondary aortic surgery or endovascular intervention in the downstream aorta after 5 years was 96% and 90%, respectively (Figure 1).
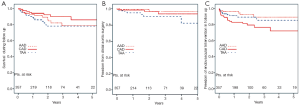
Chronic dissection
142 patients (median age 60 years) were operated on for chronic aortic dissection (100 chronic type I and 42 chronic type III). 67% underwent redo-surgery after proximal aortic repair. In-hospital mortality was 14%, with the incidence of stroke and spinal cord injury at 5% and 9%, respectively. Postoperatively, complete false lumen thrombosis to the end of the descending stent graft was achieved in 72% of patients and in 89% according to the last aortic imaging. Five-year survival rate for discharged patients was 86% and freedom from secondary thoracoabdominal surgery or endovascular intervention was 94% and 72%, respectively. In a previous study, Pacini et al. demonstrated preoperative renal insufficiency, uncontrolled placement of the E-vita open without a previously placed guide wire, prolonged ventilation, and permanent dialysis postoperatively as risk factors for mortality (8). Small true lumen (<0.25) in relation to the aortic diameter was identified as a risk factor for paraplegia.
Complex thoracic aortic aneurysmal disease
In 136 patients (median age 69 years) operated for multisegmental thoracic aneurysmal disease, in-hospital mortality and 5-year survival rate was 13% and 78%, respectively. Incidence of stroke and spinal cord injury were 7% each. The first postoperative aortic imaging demonstrated complete exclusion and thrombosis of the aneurysmal formation by the graft in 77% of patients. It has been shown that full exclusion of the aneurysm depends on the extent of the aneurysmal disease below the mid-thoracic aorta (9). Freedom from secondary open surgery and endovascular intervention was 82% and 86%, respectively.
Discussion
The favourable results from Essen using the E-vita open principle has been reproduced by a multinational community of specialized cardiovascular centres throughout Europe (1,7-9). In acute type I dissections, in-hospital mortality is comparable to surgeries without the more aggressive approach of fully resecting the aortic arch and simultaneous descending aorta stent-grafting. As freedom from distal re-interventions during 5-year follow-up reaches approximately 90%, it can be concluded that simultaneous true lumen stabilization and induction of false lumen thrombosis can result in full aortic remodeling down to the end of the stent-graft at the mid-thoracic level.
Surprisingly, the same results can be achieved by applying this treatment principle to chronic aortic disease. Freedom from secondary open surgery demonstrates that definitive treatment could be achieved in more than two-thirds of the patients. An additional endovascular procedure for extension of aortic coverage can easily be undertaken with low peri-interventional morbidity and mortality. However, the high percentage of spinal chord damage has to be taken seriously. This has led to the recommendations for simultaneous perfusion of the left subclavian artery during hypothermic circulatory arrest, the mandatory use of spinal cord fluid drainage for at least 72 hours postoperatively at high systemic arterial pressures and low central venous pressure, and landing the E-vita open stent-graft above thoracic-level 9. Small true lumen was identified as a risk factor for postoperative paraplegia in chronic dissections, which may aid in better patient selection. We are convinced that the presence of this international registry is an important tool for developing guidelines and frameworks for future algorithms and treatments of this complex patient population.
Acknowledgements
Disclosure: Heinz Jakob is consultant to Jotec GmbH, Hechingen, Germany.
References
- Jakob H, Tsagakis K, Pacini D, et al. The International E-vita Open Registry: data sets of 274 patients. J Cardiovasc Surg (Torino) 2011;52:717-23. [PubMed]
- Borst HG, Walterbusch G, Schaps D. Extensive aortic replacement using “elephant trunk” prosthesis. Thorac Cardiovasc Surg 1983;31:37-40. [PubMed]
- Safi HJ, Miller CC 3rd, Estrera AL, et al. Optimization of aortic arch replacement: two-stage approach. Ann Thorac Surg 2007;83:S815-8; discussion S824-31.
- Etz CD, Plestis KA, Kari FA, et al. Staged repair of thoracic and thoracoabdominal aortic aneurysms using the elephant trunk technique: a consecutive series of 215 first stage and 120 complete repairs. Eur J Cardiothorac Surg 2008;34:605-14; discussion 614-5. [PubMed]
- Jakob H, Dohle DS, Piotrowski J, et al. Six-year experience with a hybrid stent graft prosthesis for extensive thoracic aortic disease: an interim balance. Eur J Cardiothorac Surg 2012;42:1018-25. [PubMed]
- Tsagakis K, Kamler M, Benedik J, et al. Angioscopy--a valuable tool in guiding hybrid stent grafting and decision making during type A aortic dissection surgery. Eur J Cardiothorac Surg 2010;38:507-9. [PubMed]
- Tsagakis K, Pacini D, Di Bartolomeo R, et al. Multicenter early experience with extended aortic repair in acute aortic dissection: is simultaneous descending stent grafting justified? J Thorac Cardiovasc Surg 2010;140:S116-20; discussion S142-S146.
- Pacini D, Tsagakis K, Jakob H, et al. The frozen elephant trunk for the treatment of chronic dissection of the thoracic aorta: a multicenter experience. Ann Thorac Surg 2011;92:1663-70; discussion 1670.
- Mestres C, Tsagakis K, Pacini D, et al. One-stage repair in complex multisegmental thoracic aneurysmal disease. Results of a multicenter study. Interact CardioVasc Thorac Surg 2012;15:105.





