Durability of mitral valve repair for mitral regurgitation due to degenerative mitral valve disease
Introduction
Degenerative diseases of the mitral valve (MV) are the most common cause of MV dysfunction in developed countries. Luckily, the anatomic abnormalities that cause valve dysfunction in patients with degenerative diseases of the MV are almost always amenable to valve repair. Myxomatous degeneration of the MV, fibroelastic deficiency and dystrophic calcification of the mitral annulus comprise the entities grouped under ‘degenerative diseases of the mitral valve’.
Carpentier (1) introduced the term ‘fibroelastic deficiency’ to describe valves with thin and transparent leaflets and attenuated chordae tendineae that may rupture causing leaflet prolapse and mitral regurgitation. The leaflets are often small, thin and inelastic.
Myxomatous degeneration is the most common type of degenerative MV disease. The degree of myxomatous change varies widely from mild changes in the central portion of the posterior leaflet to generalized involvement of the entire MV apparatus. In the latter case, this results in voluminous and thickened leaflets and chordae tendineae as well as variable calcification of the annulus, myocardium and papillary muscles (2,3). Myxomatous changes tend to be more severe in the medial half than in the lateral half of the MV.
Although fibroelastic deficiency, myxomatous disease and dystrophic calcification of the mitral annulus are distinct pathological entities, they may coexist or overlap. Thus, MV with fibroelastic deficiency may have myxomatous changes in the prolapsing segment or a valve with myxomatous disease in the leaflets may have attenuated chordae tendineae indistinguishable from those with fibroelastic deficiency. Dystrophic calcification of the mitral annulus may occur in isolation or combined with myxomatous disease or fibroelastic deficiency.
This manuscript summarizes the results of MV repair for mitral regurgitation due to degenerative diseases from several studies with long-term data on 15 years and beyond.
Late outcomes of mitral valve repair for mitral regurgitation due to degenerative disease (4)
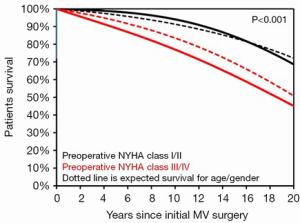
A consecutive series of 840 patients were followed prospectively and underwent echocardiographic assessment of valve function at a median 10.3 (range, 0-26) years. Patients’ mean age was 60 (range, 18-88) years and 71% were men. Approximately 48% of the patients were in New York Heart Association (NYHA) functional classes III and IV and 40% had a left ventricular ejection fraction <60%. At the time of surgery 181 patients were in atrial fibrillation or flutter, 81 (9.5%) had healed infective endocarditis and 6 had active disease. Coronary artery disease was documented in 121 (14.3%) and moderate or severe tricuspid regurgitation was present in 31 (3.7%). There were four early (<31 days) and 179 late deaths (81 cardiac or valve-related, 95 due to other causes and 3 unknown). Age by 5-year increments, NYHA functional class and left ventricular ejection fraction were independent predictors of cardiac death after MV repair. Figure 1 shows the patients’ long-term survival. Patients’ survival stratified by functional class (classes I and II vs. III and IV) was compared to that of a matched general population of Ontario for age and gender and is shown in Figure 2. MV repair failed to restore life span to normal in patients with more advanced functional classes.
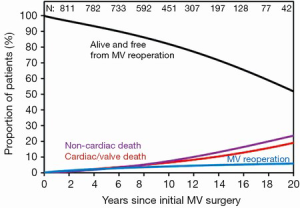
Thirty-eight patients underwent repeat MV surgery. The indication for reoperation was recurrent severe mitral regurgitation (MR) in 24 patients, mitral stenosis due to pannus on the annuloplasty ring and leaflets in 5, endocarditis in 4 and hemolytic anemia with mild or moderate MR in 5. The MV was re-repaired in 8 patients and replaced in 20. As shown in Figure 2, the probability of reoperation on the MV at 10, 15 and 20 years was 4.1% (95% CI, 3.0-5.6%), 5.1% (95% CI, 3.8-7.0%), and 5.9% (95% CI, 4.3-8.0%) respectively. Independent predictors of reoperation were isolated anterior leaflet prolapse, degree of myxomatous degeneration, Duran ring annuloplasty and duration of cardiopulmonary bypass.
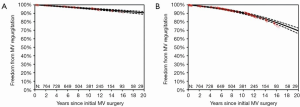
Periodical echocardiographic assessments revealed that 37 patients developed severe MR and 61 developed moderate MR. Among 37 patients with severe MR, 18 underwent reoperation, 5 were alive at the time of the report (four patients were asymptomatic with normal ventricular function and one patient was in class III and had poor ventricular function) and 14 died (eight valvular or cardiac-related deaths and six non-cardiac deaths). Among 61 patients with moderate MR, 11 underwent reoperation because of symptoms of MR or hemolysis, 28 were alive and 22 died (10 valvular or cardiac-related deaths and 12 non-cardiac deaths). Figure 3 shows the freedom from recurrent severe and severe or moderate MR.
Other valve-related events such as endocarditis, thromboembolism and anticoagulation-related hemorrhage were also examined. Nine patients developed an episode of infective endocarditis, of which five were treated with antibiotics alone and four required surgery. All patients survived reoperation. Freedom from endocarditis at 20 years was 98.5% (95% CI, 97.8-99.0%). Fifty-one patients suffered a stroke and 11 died. A total of 30 patients suffered cerebral transient ischemic attacks. The freedom from thromboembolism including transient ischemic attacks at 20 years was 85.7% (95% CI, 84.1-87.3%). The only independent predictor of thromboembolism was age by 5-year increments. A total of 174 patients were on long-term warfarin sodium therapy because of atrial fibrillation and/or a previous thromboembolic event. Thirty-eight of these patients suffered at least one serious hemorrhagic complication, of which there were eight deaths.
Very long-term durability of the edge-to-edge repair for isolated anterior mitral leaflet prolapse: Up to 21 years of clinical and echocardiographic results (5)
Alfieri’s group from Milan reported the results of MV repair on 139 patients with isolated prolapse of the anterior leaflet who were treated with the edge-to-edge repair first described by Alfieri and Maisano (6). This cohort had a mean age 54±14 years, 31% were in NYHA functional classes III and IV and 20% had atrial fibrillation The central portion of the anterior leaflet (A2) was prolapsing in 75.5% of the patients and the lateral sides of the anterior leaflet (A1 or A3) in 24.4%. In addition to the edge-to-edge repair, all patients also had an annuloplasty. Postoperative echocardiography revealed absent or mild MR in 93.5% and moderate MR in 6.4% early after surgery. After a median time interval of 11.5±3.7 years and 97% completeness of follow-up, the freedom from reoperation on the MV at 17 years (with less than 16 patients at risk) was 89.6±2.7 and the freedom from moderate and severe MR was 80.2±5.8%. Independent predictors of recurrent moderate or severe MR were residual MR at early echocardiography and posterior pericardial annuloplasty rather than prosthetic ring annuloplasty.
Very long-term results (more than 20 years) of valve repair with Carpentier’s techniques in nonrheumatic mitral valve insufficiency (7)
This report describes Professor Carpentier’s experience with MV repair in 162 patients with mitral regurgitation due to leaflet prolapse operated on from 1970 to 1984. Patients’ mean age was 56±10 years, 58% were in NYHA functional classes III and IV and 45% were in atrial fibrillation. Most patients (n=152) had type II Carpentier’s functional classification. The prolapse involved the posterior leaflet in 93 patients, the anterior leaflet in 28 patients and both leaflets in 31 patients. Repair of prolapse was accomplished by partial leaflet resection and chordal shortening or chordal transfer when necessary, in addition to a rigid remodeling annuloplasty. The median follow-up was 17 years. Ten patients required reoperation on the MV, three early and seven late. Seven had replacement and three re-repair. Freedom from reoperation at 20 years was 96.9% for posterior leaflet prolapse, 86.2% for anterior and 82.6% for bileaflet prolapse (the differences were significant by log-rank analysis with P=0.03).
Very long-term survival and durability of mitral valve repair for mitral valve prolapse (8)
This retrospective study examined the results of MV surgery for MV prolapse in patients operated on at the Mayo Clinic from 1980 to 1995. A total of 917 patients were operated on: 679 had MV repair and 238 had MV replacement. The patients’ mean age was 65±13 years, 49% were in NYHA functional classes III and IV and 42% had atrial fibrillation. In addition, 27% had coronary artery disease, likely due to a more advanced age than in most other series of MV repair for degenerative disease. There were 58 reoperations in the repair group and the probability of reoperation at 15 and 20 years was 16% and 20% respectively. Reoperations after MV repair for prolapse of the anterior leaflet (28% at 15 years) were more common than after repair of prolapse of the posterior leaflet (11% at 15 years).
Discussion
MV repair is believed to provide better long-term survival and clinical outcomes than MV replacement in patients with degenerative disease of the MV, even in patients with concomitant coronary artery disease (8,9). Although MV repair is feasible in the vast majority of patients with MR due to degenerative diseases, the value of MV repair in elderly patients with complex pathology has been challenged (10). Using a large sample size of patients with degenerative diseases of the MV that underwent MV repair or replacement, Gillinov and colleagues (10) found worse outcomes after MV replacement, but the patients were older, had more advanced functional class, more complex MV pathology and worse ventricular function. By using propensity score analysis they were able to match a subgroup of MV repair to MV replacement and found no difference in long-term survival (10). Thus, some valves with advanced myxomatous degeneration or patients with dystrophic calcification of the mitral annulus may not benefit from MV repair more than they would with MV replacement. These considerations are important when recommending surgery in asymptomatic patients with MR.
MV repair restores valve function to near normal in patients with degenerative MR but it does not arrest the degenerative process and recurrent MR is a potential complication of surgery. We have identified the pathology of the MV as an important predictor of recurrent MR (4). Isolated prolapse of the anterior leaflet and advanced myxomatous degeneration were independent predictors of recurrent MR (4). Other factors that also predicted the development of late MR in our series were advancing age, lack of an annuloplasty ring and duration of cardiopulmonary bypass (4). Our results compared favorably with other studies that used echocardiography to assess MV function after repair. The reported freedom from recurrent moderate or severe MR has varied from 77% at 5 years (11), 71% at 7 years (12) and 81% at 10 years (13). These differences are likely related to patient selection and experience of the surgeon (14). Since the introduction of chordal replacement with Gore-Tex sutures into our practice in 1986, not only have a higher proportion of patients had MV repair instead of replacement but we have also increased the number of chords replaced per case (15). We believe that a large number of neo-chords is particularly important in cases of anterior leaflet prolapse, which is associated with higher rates of recurrent MR than isolated posterior leaflet prolapse (4-8,16). We frequently use 20 to 30 neo-chords of Gore-Tex in cases of bileaflet prolapse (16).
In our series of MV repairs, 78 patients did not have a mitral annuloplasty ring or band because we deemed the mitral annulus and leaflet to be relatively small (e.g., cases of fibroelastic deficiency) and an annuloplasty could have caused stenosis (4). By multivariable analysis, those patients had a higher risk of recurrent moderate MR but not for reoperation. It seems that mitral annuloplasty is necessary in all patients with MR due to degenerative disease (17). The type of mitral annuloplasty ring (rigid ring such as Carpentier’s, flexible such as Duran’s or simply a posterior band such as Cosgrove’s) had no effect on late recurrent MR in our experience (4). However, we found that the Duran ring was a risk factor for reoperation on the MV largely because of 5 patients who developed mitral stenosis due to excessive pannus on the annuloplasty ring with invasion into the leaflets (18). We did not encounter this problem with the Carpentier ring or Cosgrove band in our patients (4).
Freedom from reoperation on the MV underscores freedom from recurrent MR (4,11-13). This is likely due to the fact that reoperation is not usually offered to patients with recurrent moderate MR and asymptomatic severe MR. Thus, freedom from reoperation on the MV is not an accurate measurement of durability of MV repair. At 20 years in our series, only 6% of our patients had reoperation on the MV whereas almost twice as many developed severe MR and approximately 5 times more developed recurrent moderate MR (4).
In conclusion, MV repair is feasible in most patients with degenerative MR and the freedom from reoperation is very high, particularly in patients with posterior leaflet prolapse. However, patients with more advanced degenerative diseases also benefit from MV repair.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Carpentier A. Cardiac valve surgery--the "French correction". J Thorac Cardiovasc Surg 1983;86:323-37. [PubMed]
- Adams DH, Anyanwu AC. Seeking a higher standard for degenerative mitral valve repair: begin with etiology. J Thorac Cardiovasc Surg 2008;136:551-6. [PubMed]
- Carpentier AF, Pellerin M, Fuzellier JF, et al. Extensive calcification of the mitral valve anulus: pathology and surgical management. J Thorac Cardiovasc Surg 1996;111:718-29; discussion 729-30. [PubMed]
- David TE, Armstrong S, McCrindle BW, et al. Late outcomes of mitral valve repair for mitral regurgitation due to degenerative disease. Circulation 2013;127:1485-92. [PubMed]
- De Bonis M, Lapenna E, Taramasso M, et al. Very long-term durability of the edge-to-edge repair for isolated anterior mitral leaflet prolapse: up to 21 years of clinical and echocardiographic results. J Thorac Cardiovasc Surg 2014;148:2027-32. [PubMed]
- Alfieri O, Maisano F. An effective technique to correct anterior mitral leaflet prolapse. J Card Surg 1999;14:468-70. [PubMed]
- Braunberger E, Deloche A, Berrebi A, et al. Very long-term results (more than 20 years) of valve repair with carpentier's techniques in nonrheumatic mitral valve insufficiency. Circulation 2001;104:I8-11. [PubMed]
- Mohty D, Orszulak TA, Schaff HV, et al. Very long-term survival and durability of mitral valve repair for mitral valve prolapse. Circulation 2001;104:I1-I7. [PubMed]
- Gillinov AM, Blackstone EH, Nowicki ER, et al. Valve repair versus valve replacement for degenerative mitral valve disease. J Thorac Cardiovasc Surg 2008;135:885-93, 893.e1-2.
- Gillinov AM, Faber C, Houghtaling PL, et al. Repair versus replacement for degenerative mitral valve disease with coexisting ischemic heart disease. J Thorac Cardiovasc Surg 2003;125:1350-62. [PubMed]
- Stevens LM, Basmadjian AJ, Bouchard D, et al. Late echocardiographic and clinical outcomes after mitral valve repair for degenerative disease. J Card Surg 2010;25:9-15. [PubMed]
- Flameng W, Herijgers P, Bogaerts K. Recurrence of mitral valve regurgitation after mitral valve repair in degenerative valve disease. Circulation 2003;107:1609-13. [PubMed]
- Shimokawa T, Kasegawa H, Katayama Y, et al. Mechanisms of recurrent regurgitation after valve repair for prolapsed mitral valve disease. Ann Thorac Surg 2011;91:1433-8; discussion 1438-9. [PubMed]
- Kilic A, Shah AS, Conte JV, et al. Operative outcomes in mitral valve surgery: combined effect of surgeon and hospital volume in a population-based analysis. J Thorac Cardiovasc Surg 2013;146:638-46. [PubMed]
- David TE, Armstrong S, Ivanov J. Chordal replacement with polytetrafluoroethylene sutures for mitral valve repair: a 25-year experience. J Thorac Cardiovasc Surg 2013;145:1563-9. [PubMed]
- Gillinov AM, Blackstone EH, Alaulaqi A, et al. Outcomes after repair of the anterior mitral leaflet for degenerative disease. Ann Thorac Surg 2008;86:708-17; discussion 708-17. [PubMed]
- Gillinov AM, Tantiwongkosri K, Blackstone EH, et al. Is prosthetic anuloplasty necessary for durable mitral valve repair? Ann Thorac Surg 2009;88:76-82. [PubMed]
- Ibrahim MF, David TE. Mitral stenosis after mitral valve repair for non-rheumatic mitral regurgitation. Ann Thorac Surg 2002;73:34-6. [PubMed]





