Video-atlas of radical pleurectomy for malignant pleural mesothelioma
Introduction
Malignant pleural mesothelioma (MPM) is an aggressive malignancy arising from the mesothelial surfaces of the pleura. Macroscopic complete resection (MCR) seems to have the greatest impact on survival in surgery-based multimodality treatment protocols (1). Depending on the surgical preference and intraoperative findings, extrapleural pneumonectomy (EPP) or aggressive radical pleurectomy (RP) or pleurectomy/decortication (P/D) might achieve MCR even at advanced stages or in the presence of higher tumor burden (2).
There is a variable definition of RP and P/D in the literature. In our definition, RP is a surgical procedure with complete lung-sparing resection of the visceral and parietal pleura (3). Wedge resections are carried out in the event of deep infiltration of the lung parenchyma. Care is taken to preserve the phrenic nerve, pericardium and diaphragm whenever possible. If necessary, partial or total resection and reconstruction of the diaphragm and pericardium can be carried out. In contrast, the International Association for the Study of Lung Cancer International Staging Committee (IASLC) and the International Mesothelioma Interest Group (IMIG) define P/D as a surgical procedure to remove all macroscopic tumour involving the parietal and visceral pleura. The term “extended” P/D was proposed for additional diaphragmatic or pericardial resection (4).
Furthermore, it has been shown that patients undergoing P/D and having incomplete resection (R2) might have comparable survival to patients having MCR with EPP (5). Thus, it is very important to have the ability to perform RP in the management of MPM from a functional and/or oncological point of view. The accompanying video represents an effort to demonstrate the key steps in how to perform RP.
Case presentation
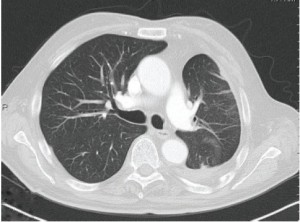
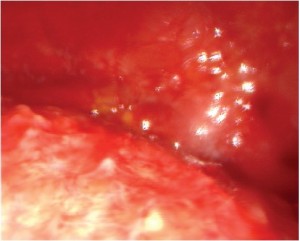
This is a 79-year old man with previous occupational asbestos exposure presenting with unilateral left-sided pleural effusion. Initial CT-scan showed a thickened pleura within the left chest (Figure 1). After video-assisted thoracoscopic exploration, MPM was provisionally diagnosed on the basis of macroscopic intraoperative view (Figure S1). Pleural biopsy confirmed the diagnosis of epitheloid MPM. The patient underwent RP with resection and reconstruction of the diaphragm due to local infiltration (Video 1). Adequate MCR was achieved at the end of surgery. The patient was extubated immediately after surgery and transferred to the intensive care unit. The postoperative X-ray of the chest showed a fully expanded lung on the left side. The final examination of the resected specimens confirmed the pathological IMIG stage III [pT3 N0 (0/23)].
Preoperative assessment
All patients undergo preoperative pulmonary and cardiac evaluation: pulmonary function test (PFT), quantitative perfusion scans, stress tests and transthoracic echocardiography. All patients have to meet standard cardiopulmonary criteria for the proposed resections according to the algorithm of Miller (6). However, lung-sparing RP is associated with significant improvement of PFTs and lung perfusion in patients with MPM. Thus, even patients with impaired preoperative lung function might be a candidate for RP [3]. Routine staging includes computed tomographic (CT) scan of the chest and abdomen. Magnetic resonance imaging (MRI) is considered as the standard reference if infiltration of the chest wall, mediastinal organs, heart or great vessels is suspected. Positron emission tomography (PET), mediastinoscopy or laparoscopy are not routinely performed (7).
Anesthetic considerations
Pulse oximetry, central venous and arterial cannulations are the current standard for our patients as a routine for all major thoracic resections. All patients receive general anesthesia and double lumen endobronchial intubation. Positive end-expiratory pressure (PEEP) during anesthesia is used and PEEP is adjusted, as needed, to facilitate the dissection of the visceral pleura. Intraoperative bronchoscopy performed by the anesthesiologist is helpful in suctioning blood and secretions. A close collaboration between the anesthesiologist and surgeon is of critical importance throughout the entire procedure.
Thoracotomy
The operation is performed in the straight lateral decubitus position. We prefer a large s-shaped skin incision. All chest tube tracts and thoracoscopy incisions have to be resected until the pleura is reached to avoid recurrence in these areas. A rib-sparing posterolateral thoracotomy is performed in the 6th or 7th intercostal space depending on the expected tumor burden and distribution. The serratus anterior muscle is preserved and mobilized anteriorly. A posterior costotomy of one rib is enough to get adequate access into the chest. In most of the cases, we perform a second basal thoracotomy to get better visualization and access to the diaphragm and the costophrenic angle.
Extrapleural dissection
The extrapleural dissection from the chest wall usually can be done bluntly and en-bloc until the mediastinum and diaphragm are reached. We pack each section with warm laparotomy pads for hemostasis. Attempts should be made to dissect the endothoracic fascia en-bloc with the parietal pleura. Otherwise the fascia is removed piecemeal. At this point, frozen sections of the endothoracic fascia might be useful for decision making. During the entire extrapleural dissection, care must be taken not to injure the subclavian vessels, phrenic and vagal nerves, superior vena cava, azygos vein and the internal mammary vessels. Esophageal injuries may be avoided by the use of a naso-gastric tube.
Dissection of the diaphragm and pericardium
The RP technique usually allows the isolated resection of the diaphragmatic pleura, leaving the bare muscles of the diaphragm behind without impairment of diaphragmatic function. If the tumor extension involves the diaphragmatic muscle, diaphragm resection and reconstruction with Goretex (2 mm) in the standard fashion might be necessary. All attempts should be made not to open the peritoneum to avoid tumor seeding into the abdomen. However, preservation of diaphragm function is associated with greater increase in FVC and FEV1, respectively (3). Thus, the preservation of the diaphragm should be attempted whenever technically and oncologically feasible. The fibrous part is resected while the serous part of the pericardium is left. However, resection and reconstruction with Goretex is carried out in case of macroscopic tumour involving the pericardium. Similarly, the phrenic nerve may also have to be sacrificed, in case of inseparable macroscopic tumor. In our opinion, it is very important to keep the pericardial sac closed, whenever possible, until the resection is completed and the hemithorax is irrigated to avoid possible tumour spread into the pericardium.
Visceral pleurectomy
PEEP is adjusted as needed to facilitate the distinction between lung and pleura during the operation. The dissection of the visceral pleura can be very challenging. The correct dissection plane is created after a sharp incision with a blade of the attached parietal and visceral pleura. The visceral pleurectomy or decortication proceeds with blunt (using fingers, small sponge stick, or other grasping instruments) and sharp dissection (scalpel or scissors). The fissures are dissected in the same fashion. However, dissecting the tumor burden from the underlying interlobar vessels can be very dangerous. This surgical step is performed without PEEP. Vessel loops or tourniquets around the main pulmonary artery might be useful before the dissection in the fissures to restrain the blood flow in case of severe bleeding. Wedge resections can be performed in the event of lung parenchymal invasion. The final resection steps including the en-bloc specimen with visceral and parietal pleura with attached diaphragm and mediastinal fat tissue (Video 1).
Lymph node dissection
Systematic interlobar, hilar and mediastinal lymphadenectomy is done routinely after RP, according to IASLC lung cancer surgery guidelines (8). We do not routinely dissect the lymph nodes along the internal mammary artery, but do so only in the event of macroscopic lymph node metastases. Lymph nodes are labeled to facilitate correct postoperative staging.
Post-resectional steps
The thoracic cavity is irrigated. We prefer irrigation with peroxide (17.5%) followed by warm saline. Two large chest tubes (28 Charriere) are placed anteriorly and posteriorly. The anterior chest tube is placed at the apex of the hemithorax while the second chest tube extends from the diaphragm to the posterior site of the decorticated lung. The chest tubes are maintained under suction.
Postoperative management
All attempts should be made to extubate the patients immediately after the surgical procedure. Whenever postoperative mechanical ventilation is indicated, the double-lumen tube should be replaced by standard endotracheal single-lumen tube. Careful fluid management is important after RP in the same manner as after any major lung resection. The tubes are converted to water seal depending on the amount of air leakage. Postoperative air leakage is common even after the 10th postoperative day.
Acknowledgements
We thank the nursing staff for their valuable assistance in making this surgical movie.
Disclosure: The author declares no conflict of interest.
References
- Sugarbaker DJ. Macroscopic complete resection: the goal of primary surgery in multimodality therapy for pleural mesothelioma. J Thorac Oncol 2006;1:175-6.
- Flores RM. Surgical options in malignant pleural mesothelioma: extrapleural pneumonectomy or pleurectomy/decortication. Semin Thorac Cardiovasc Surg 2009;21:149-53.
- Bölükbas S, Eberlein M, Schirren J. Prospective study on functional results after lung-sparing radical pleurectomy in the management of malignant pleural mesothelioma. J Thorac Oncol 2012;7:900-5.
- Rice D, Rusch V, Pass H, et al. Recommendations for uniform definitions of surgical techniques for malignant pleural mesothelioma: a consensus report of the International Association for the Study of Lung Cancer International Staging Committee and the International Mesothelioma Interest Group. J Thorac Oncol 2011;6:1304-12.
- Lang-Lazdunski L, Bille A, Lal R, et al. Pleurectomy/decortication is superior to extrapleural pneumonectomy in the multimodality management of patients with malignant pleural mesothelioma. J Thorac Oncol 2012;7:737-43.
- Miller JI Jr. Complications of pulmonary surgery: preoperative evaluation. Chest Surg Clin N Am 1992;2:701-11.
- Bölükbas S, Manegold C, Eberlein M, et al. Survival after trimodality therapy for malignant pleural mesothelioma: Radical Pleurectomy, chemotherapy with Cisplatin/Pemetrexed and radiotherapy. Lung Cancer 2011;71:75-81.
- Rusch VW, Asamura H, Watanabe H, et al. The IASLC lung cancer staging project: a proposal for a new international lymph node map in the forthcoming seventh edition of the TNM classification for lung cancer. J Thorac Oncol 2009;4:568-77.