Long-term results after robotically assisted coronary bypass surgery
Introduction
Robotically-assisted endoscopic coronary bypass surgery offers potential advantages over conventional coronary artery bypass grafting (CABG), specifically reduced surgical trauma and shortened recovery time. Long-term performance of the procedure is still not clear. It is important to understand whether robotically-assisted procedures provide the same clinical quality as the established open coronary bypass surgery through sternotomy. The aim of this review was to investigate and analyze the currently available long-term outcome data following robotically-assisted endoscopic coronary bypass surgery.
Methods
A PubMed search was carried out using “robotic”, “robotically”, “assisted”, “coronary”, and “bypass” as the primary key words. “Long-term” outcome was defined as outcome reported for the time-frame after one year post intervention. Eleven studies were eligible for review.
Both robotically-assisted totally endoscopic versions of the procedure and robotically assisted operations with an adjunctive mini-thoracotomy were included. The completely endoscopic version of the procedure is commonly referred to as TECAB (totally endoscopic coronary artery bypass), while the mini-thoracotomy version is called robotically assisted MIDCAB (minimally invasive direct coronary artery bypass). Six out of the 11 studies included combinations of robotic coronary artery bypass grafting and percutaneous coronary interventions, comprising the so-called “hybrid” coronary revascularization.
We specifically evaluated long-term survival, freedom from angina, patency of bypass grafts, freedom from re-intervention, and freedom from major adverse cardiac and cerebrovascular events (MACCE). These outcome measures were tabulated in a chronological fashion listing the first author, year of publication, surgical method applied, timeframe of patient observation, and cumulative freedom from the above events.
Reported freedom from event rates were also plotted against a postoperative 5-year time scale.
Results
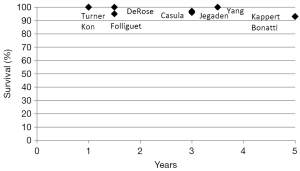
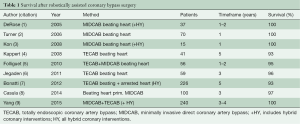
Table 1 shows the intermediate and long-term survival rates in several current series on robotically-enhanced CABG. For the timeframe of one to 5 years postoperatively, survival rates are reported to be over 90% in all studies. One study even reports 100% survival at 41 months (9). In another paper showing 93% survival at 5 years, all deaths on follow-up were non-cardiac in nature (4). Figure 1 depicts the collective survival curve derived from the literature data.
Full table
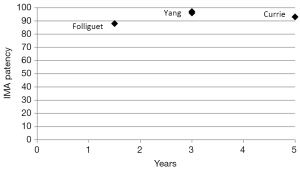
Four out of the eleven studies reported on graft patency. Table 2 highlights patency rates of the grafts placed with robotic assistance. The patency rates were above 90% in the studies reporting them. One very long-term study stated 93% patency of the internal mammary artery (IMA) at 5 years (10). Figure 2 shows the collective IMA patency rate.

Full table
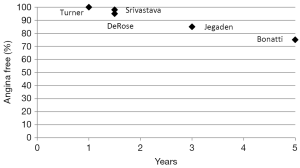
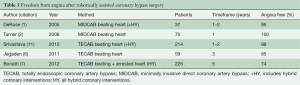
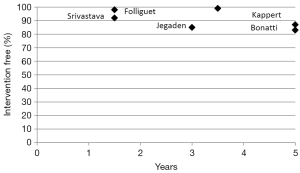
Freedom from angina approached 85% in one study at 3 years, and 74% in another study at 5 years (Table 3). The yearly trend of angina re-occurrence is seen in Figure 3.
Full table
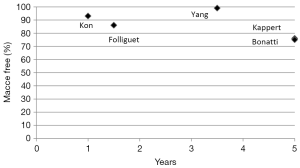
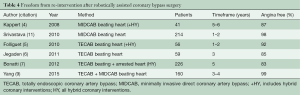
As shown in Table 4 and Figure 4, freedom from re-intervention remained in the middle 80% range at 5 years.
Full table
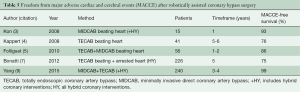
Studies reporting 5-year freedom from MACCE are listed in Table 5. The collective freedom from MACCE plot is shown in Figure 5, with a trend towards 75% freedom from any adverse event at the end of the observation period.
Full table
Discussion
Robotically-assisted coronary bypass surgery remains a controversial and an extensively debated procedure. The present review summarizes the currently available long-term data for endoscopic coronary bypass surgery. The long-term studies which were reviewed consistently showed that endoscopic coronary bypass surgery has excellent long-term results with outcomes comparable to conventional CABG with sternotomy.
Survival
The collective data derived from the reviewed studies demonstrates a 1- to 2-year survival ranging between 95% and 100%, and a 5-year survival in the 93% range. The studies in our review contain patients with left anterior descending (LAD) artery disease, as well as patients with multi-vessel disease who were treated with hybrid revascularization. Data from the Society of Thoracic Surgeons (STS) database linked with the Social Security Death Master File (SSDMF) revealed a 1-year survival rate of 88.9% in 7,344 patients with all vein grafts, 95.2% in patients with single IMA grafts, 97.4% in patients with bilateral IMAs, and 95.4% of patients with all arterial grafts (range, 88.9–95.2%) (12). An early study from the Cleveland Clinic main campus demonstrated a 5-year survival rate of 97% in patients with conventional on-pump isolated single LIMA to LAD grafts (13). Five-year survival rates of patients with multi-vessel disease in the ARTS and SYNTAX trials were 92% and 89%, respectively (14,15). Survival at 5-year in the FREEDOM trial, which evaluated diabetics with multi-vessel disease, was 89.8% in the surgical arm of the study (16). A recent Cleveland Clinic study including 11922 CABG procedures in diabetics (17) revealed 5-year survival rates of 75%, 82%, and 91% after vein grafting, single IMA use, and double IMA use respectively, once again confirming the tremendous advantages of two internal mammary arteries and underscoring the survival disadvantage of diabetics overall. One benefit that robotic techniques offer is placement of these two arterial conduits without splitting the sternum. This is probably the most promising aspect of these procedures.
IMA patency
According to the reviewed literature, the 5-year patency rates of robotically placed IMA ranged between 88% and 97%, demonstrating that the quality of the bypass grafts meets current quality standards. A classic study on patency of coronary bypass grafts by Fitzgibbon and co-workers (18) reported a perfect IMA patency rate of 85% and general patency including low grade graft stenosis of 95% at one to two and a half years. Five-year perfect IMA patency rates and general patency rates were 83% and 91%, respectively. It needs to be kept in mind that only four out of the 11 studies reported on patency rates and firm conclusions cannot be drawn. Angiographic follow-up studies would be desirable to get a clearer view on the performance of robotically placed bypass conduits.
Freedom from angina
Twenty-six percent of patients in this review developed angina at 5-years postoperatively. Only one study, however, described this endpoint at 5-years and included complex hybrid interventions in patients with multi-vessel disease (7). Freedom from angina rates in the studies that reported on earlier time points ranged from 85% to 100% (1,2,6,11). Out of the larger CABG studies, the ARTS trial demonstrated a 5-year angina recurrence rate of 15.5% for CABG, and 21.2% for percutaneous coronary intervention (PCI) using bare metal stents (14). Freedom from angina is a soft endpoint and definitely more difficult to assess than freedom from death, stroke, and re-intervention.
Freedom from re-intervention
As expected, not all patients who developed symptoms after robotic coronary bypass grafting need re-intervention, and approximately 15% underwent another procedure during a 5-year timeframe. It is important to note that some of the studies that we investigated included hybrid procedures, and several re-interventions may have been caused by in-stent restenosis and/or occlusion. It was not possible to differentiate between re-operation and percutaneous re-intervention from the available data. Long-term results of the SYNTAX trial demonstrated a 5-year repeat revascularization rate of 13.7% after conventional CABG (15), while the corresponding overall re-intervention rate in the earlier ARTS trial (14) was 8.8% for CABG through sternotomy. For both studies, this re-intervention rate was significantly lower than in the percutaneous interventional arms of the trials.
Freedom from MACCE
The data in this review demonstrates a freedom from MACCE rate after robotic CABG comparable with MACCE-free rates in large series on conventional CABG. The 5-year rates of freedom from MACCE in the surgical arms of the SYNTAX trial and ARTS trial were 73.1% and 78% respectively (14,15), very similar to the findings in our study which showed a MACCE free survival between 75% and 76% at 5-years. In the multi-vessel PCI arm of the SYNTAX trial, freedom from major adverse cardiac and cerebrovascular events was 62.6%, roughly 10% lower than after surgery (15). Robotic CABG offers an opportunity to place single or double IMA bypass grafts without opening the chest. If this factor is included in future revascularization concepts, better long-term results can be achieved compared to multi-vessel stenting, and probably closer to multivessel CABG may be expected. Data on long-term event-free survival after conventional single LIMA to LAD grafting are not well-published. A study conducted in 2000 by Greenbaum and co-workers described a MACE-free rate of 80% after isolated IMA grafting (19). Freedom from death, myocardial infarction and stroke at 5-years in the FREEDOM trial was 81.3% for CABG (16), though re-interventions were not part of the composite endpoint in this trial. Five-year event-free survival for PCI was 73.4%.
Limitations of this review
Major limitations of the current literature review of long-term outcomes of robotically-assisted CABG include the fact that a variety of surgical techniques were utilized. Such procedures ranged from robotically assisted CABG with adjunctive mini-thoracotomies, to completely endoscopic versions performed using a port-only approach. In addition, beating heart as well as arrested heart methods formed part of the spectrum of surgical techniques. The variability of approaches furthermore encompassed single LIMA to LAD grafting, multivessel robotic CABG, and hybrid interventions. In addition, technology has progressed since the introduction of surgical robots in the late 1990s. Lastly, single surgeon and team learning curves may have also affected the results.
Conclusions
The current literature review revealed that from a very general perspective, long-term results after robotically-assisted CABG are consistent and comparable with results published for open CABG through sternotomy.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Derose JJ Jr, Balaram SK, Ro C, et al. Mid-term results and patient perceptions of robotically-assisted coronary artery bypass grafting. Interact Cardiovasc Thorac Surg 2005;4:406-11. [Crossref] [PubMed]
- Turner WF Jr, Sloan JH. Robotic-assisted coronary artery bypass on a beating heart: initial experience and implications for the future. Ann Thorac Surg 2006;82:790-4; discussion 794. [Crossref] [PubMed]
- Kon ZN, Brown EN, Tran R, et al. Simultaneous hybrid coronary revascularization reduces postoperative morbidity compared with results from conventional off-pump coronary artery bypass. J Thorac Cardiovasc Surg 2008;135:367-75. [Crossref] [PubMed]
- Kappert U, Tugtekin SM, Cichon R, et al. Robotic totally endoscopic coronary artery bypass: a word of caution implicated by a five-year follow-up. J Thorac Cardiovasc Surg 2008;135:857-62. [Crossref] [PubMed]
- Folliguet TA, Dibie A, Philippe F, et al. Robotically-assisted coronary artery bypass grafting. Cardiol Res Pract 2010;2010:175450.
- Jegaden O, Wautot F, Sassard T, et al. Is there an optimal minimally invasive technique for left anterior descending coronary artery bypass? J Cardiothorac Surg 2011;6:37. [Crossref] [PubMed]
- Bonatti JO, Zimrin D, Lehr EJ, et al. Hybrid coronary revascularization using robotic totally endoscopic surgery: perioperative outcomes and 5-year results. Ann Thorac Surg 2012;94:1920-6; discussion 1926.
- Casula R, Khoshbin E, Athanasiou T. The midterm outcome and MACE of robotically enhanced grafting of left anterior descending artery with left internal mammary artery. J Cardiothorac Surg 2014;9:19. [Crossref] [PubMed]
- Yang M, Wu Y, Wang G, et al. Robotic Total Arterial Off-Pump Coronary Artery Bypass Grafting: Seven-Year Single-Center Experience and Long-Term Follow-Up of Graft Patency. Ann Thorac Surg 2015;100:1367-73. [Crossref] [PubMed]
- Currie ME, Romsa J, Fox SA, et al. Long-term angiographic follow-up of robotic-assisted coronary artery revascularization. Ann Thorac Surg 2012;93:1426-31. [Crossref] [PubMed]
- Srivastava S, Gadasalli S, Agusala M, et al. Beating heart totally endoscopic coronary artery bypass. Ann Thorac Surg 2010;89:1873-9; discussion 1879-80.
- Jacobs JP, Edwards FH, Shahian DM, et al. Successful linking of the Society of Thoracic Surgeons database to social security data to examine survival after cardiac operations. Ann Thorac Surg 2011;92:32-7; discussion 38-9. [Crossref] [PubMed]
- Boylan MJ, Lytle BW, Loop FD, et al. Surgical treatment of isolated left anterior descending coronary stenosis. Comparison of left internal mammary artery and venous autograft at 18 to 20 years of follow-up. J Thorac Cardiovasc Surg 1994;107:657-62. [PubMed]
- Serruys PW, Ong AT, van Herwerden LA, et al. Five-year outcomes after coronary stenting versus bypass surgery for the treatment of multivessel disease: the final analysis of the Arterial Revascularization Therapies Study (ARTS) randomized trial. J Am Coll Cardiol 2005;46:575-81. [Crossref] [PubMed]
- Mohr FW, Morice MC, Kappetein AP, et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet 2013;381:629-38. [Crossref] [PubMed]
- Farkouh ME, Domanski M, Sleeper LA, et al. Strategies for multivessel revascularization in patients with diabetes. N Engl J Med 2012;367:2375-84. [Crossref] [PubMed]
- Raza S, Sabik JF 3rd, Masabni K, et al. Surgical revascularization techniques that minimize surgical risk and maximize late survival after coronary artery bypass grafting in patients with diabetes mellitus. J Thorac Cardiovasc Surg 2014;148:1257-64; discussion 1264-6. [Crossref] [PubMed]
- Fitzgibbon GM, Kafka HP, Leach AJ, et al. Coronary bypass graft fate and patient outcome: angiographic follow-up of 5,065 grafts related to survival and reoperation in 1,388 patients during 25 years. J Am Coll Cardiol 1996;28:616-26. [Crossref] [PubMed]
- Greenbaum AB, Califf RM, Jones RH, et al. Comparison of medicine alone, coronary angioplasty, and left internal mammary artery-coronary artery bypass for one-vessel proximal left anterior descending coronary artery disease. Am J Cardiol 2000;86:1322-6. [Crossref] [PubMed]