Outcomes of surgical and transcatheter aortic valve replacement in the octogenarians—surgery still the gold standard?
Abstract
Background: Contemporary options for aortic valve replacement (AVR) include transcatheter and surgical approaches (TAVR and SAVR). As evidence accrues for TAVR in high and intermediate risk patients, some clinicians advocate that all patients aged over 80 years should only receive TAVR. Our aim was to investigate the utility of SAVR and minimally invasive AVR (mAVR) among octogenarians in the current era of TAVR.
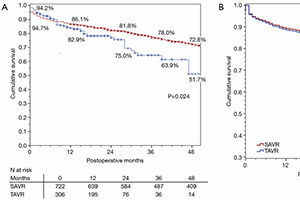
Methods: From 2002 to 2015, 1,028 octogenarians underwent isolated AVR; 306 TAVR and 722 SAVR, of which 378 patients underwent mAVR. Logistic regression and Cox modeling were used to evaluate overall operative mortality and mid-term survival, respectively. Patients were stratified based on procedural approaches (mAVR or full sternotomy for SAVR, and transfemoral or alternate access for TAVR). Median follow-up was 35 [interquartile range (IQR) 14–65] months.
Results: Compared to SAVR patients, TAVR patients were relatively older (86.2 versus 84.2 years) with co morbidities such as chronic kidney disease (CKD), diabetes mellitus (DM), cerebrovascular disease (CVD), and prior myocardial infarction (MI), all P<0.05. The mean STS-PROM for the TAVR group was statistically higher, 6.81 versus 5.58 for the SAVR group (P<0.001). The median in-hospital LOS was statistically higher for the SAVR group (P<0.05). Cox proportional hazard modeling, adjusted for temporal differences in procedure and patient selection, identified age, New York Heart Association (NYHA) class III/IV, preoperative creatinine, severe chronic lung disease, prior cardiac surgery as significant predictors of decreased survival (all P<0.05), while type of intervention (approach) was non-contributory. Adjusted operative mortality stratified by procedure approaches was similar between full sternotomy SAVR and mAVR, and between alternative access and transfemoral TAVR.
Conclusions: After adjusting for confounders, TAVR (regardless of approach), SAVR, and mAVR had comparable operative mortality and mid-term survival. Treatment decisions should be individualized with consensus from a multi-disciplinary heart team, taking into account patient co morbidities, frailty, and quality of life. We believe certain patient groups will still benefit from SAVR even in this elderly population.
Cover