Hybrid three-stage repair of mega-aortic syndrome with the Lupiae technique: 10-year results
Abstract
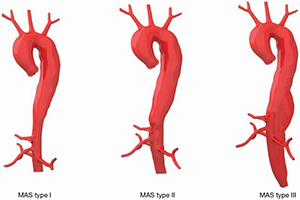
Background: Mega-aortic syndrome (MAS) is a rare disease carrying a poor prognosis if treated conservatively. Open repairs of these aneurysms are invasive, while totally endovascular repairs are associated with higher rates of late reintervention due to endoleaks, compromising long-term prognosis. We describe the 10-year results of a hybrid three-stage approach to MAS using the Lupiae technique.
Methods: Between 2006 and 2016, 27 patients with MAS extending from the ascending aorta to the iliac arteries (MAS type III) underwent: (I) a surgical aortic arch debranching, using the Vascutek Lupiae™ multibranched graft to create a proximal Dacron landing zone; (II) an abdominal aorta debranching to create a distal Dacron landing zone and (III) the implantation of multiple endovascular stents to exclude any residual aneurysm between the two landing zones.
Results: One patient died following the first stage, and another following the second stage of the repair (overall mortality 7.4%). The interval between the first and the second stage was 58.3±16.1 days. The interval between the second and the third stage was 47.7±13.1 days. Four-year survival was 88.6%±6.2% while 10-year survival was 51.7%±17.9%. One patient had a type III endoleak after the third stage that self-resolved within 6 months without intervention. No patient had type I or II endoleaks and none underwent redo procedures. Mean follow-up was 5.9±3.6 years and completeness was 100%.
Conclusions: Three-stage hybrid repairs using the Lupiae technique can be safely performed in MAS type III patients. Short intervals between the stages should mitigate the risk of rupture during the waiting periods and may enhance patient compliance, but to achieve this, the burden and the complexity of the first stage must be carefully weighted. Our strategy improves the long-term survival of these patients compared to their natural history and is less invasive than an open repair. The adoption of Dacron landing zones appears to be associated with very low rates of reintervention due to endoleaks.
Cover