External aortic cross-clamping and endoaortic balloon occlusion in minimally invasive mitral valve surgery
Introduction
Minimally invasive cardiac surgery through the right mini-thoracotomy approach has established itself as standard of care for the treatment of pathologies affecting the atrio-ventricular valves (1). Experienced and specifically trained surgeons can achieve excellent operative results via the standard sternotomy approach, with many studies reporting better pain control, a faster recovery and a shorter hospital stay as compared to conventional surgery (2). Rather than a single approach, minimally invasive surgery refers to a collection of different techniques involving specific technologies, modified vascular access for cardiopulmonary bypass (CPB) perfusion and visualization. Two techniques of aortic occlusion and cardiac protection have been used: the transthoracic aortic clamp (TTC) and the endoaortic balloon occlusion (EAO). Both approaches present peculiar advantages and potential technical pitfalls. Few papers underlined the safety and reproducibility of these two techniques with personal experience and institutional preferences that probably played a major role in results. Two recent meta-analyses (3,4) revealed similar risk of mortality for the two approaches and no difference in the occurrence of perioperative stroke. However, a higher risk of aortic dissection was reported in patients who had the endoaortic conclusion compared to cross-clamping populations. We have reviewed our experience in mini-thoracotomy cardiac surgery in patients who received an external aortic clamp and patients who underwent operation with EAO.
Methods
Patients
We analyzed prospectively collected data of patients who received minimally invasive mitral surgery during the period January 2013 and July 2018. All patients who underwent cardiac operations for mitral valve dysfunction and other associated pathologies were included in the study. Reoperations and combined procedures were included as well. Ultimately, we retrieved information from 258 patients.
All patients underwent preoperative coronary angiography, chest X-ray and full transthoracic echocardiography. Trans-esophageal echo (TEE) study was performed before the operation in case of difficult interpretation of transthoracic images and always soon after intubation in theatre. In the cases with a documented history or clinical suspicion of peripheral vascular disease or thoraco-abdominal aortic disease, we performed a preoperative CT scan of the whole aorta. Severe vessels pathology, right chest disease or previous right lung/pleura surgery led us to a sternotomy approach. These cases account for about 4% of atrio-ventricular valves surgical activity.
Preoperative patient characteristics align with the definition of the EuroSCORE II model. Atrial fibrillation includes patients with history of paroxysmal, persistent and permanent arrhythmia. Cardiac enzymes were routinely evaluated after 12–18 hours since the end of the operation in postoperative day 1 (the results from this sample were included in the analysis) and every day until postoperative day 3. Complications were recorded within 30 days since the operation.
Interventions
A double-lumen endobronchial tube was used to allow single lung ventilation. A 19-Fr venous cannula was placed in the superior caval vein through the right jugular vein under TOE guidance for CPB venous return. Femoral vessels were exposed over the groin skin line with a 3-cm incision. The femoral arteries (19–21 Fr cannula) and femoral veins (23/25 Fr two-staged cannula) were cannulated using the Seldinger technique under TOE guidance. When an endoaortic balloon was used, a specific cannula with a side arm was inserted in the femoral artery (21–23 Fr). Afterwards, a guidewire was introduced and advanced into the ascending aorta under TOE guidance. The endoaortic balloon was finally placed over this guidewire before initiation of cardiopulmonary bypass (CPB). A 5–6 cm incision was then made at the inframammary fold in female patients and over the nipple in male patients; more recently, a periareolar incision was performed in male patients and women with small breasts. The mini-thoracotomy was performed at the level of the 4th intercostal space. A rib spreader was used in some cases to allow a better visualization of the aorta in patients receiving external aortic cross-clamping. Two ports were placed in the 4th and 6th intercostal space for intracardiac suction line and carbon dioxide delivery. The pericardium was opened 2 cm above the phrenic nerve and in most of the cases, two retraction stitches were passed. The field was flooded by carbon dioxide delivered at 3–4 L/min. CPB was started and the patient cooled down 30–32 °C. Vacuum-assisted venous drainage was utilized (maximum negative pressure −40 mmHg). In case of external cross-clamping, a flexible clamp was inserted through the mini-thoracotomy. Cold blood cardioplegia was used in 199 patients and the dose repeated every 20 minutes; in 59 cases, intracellular crystalloid cardioplegic solution ensured the cardiac arrest. Most of these cases were endoaortic balloon aortic occlusions. EAO was carefully monitored with TOE during positioning of the balloon in the ascending aorta, during inflation and during cardioplegia delivery. The left atrium was opened at the level of the interatrial groove; an atrial retractor with a side arm was placed laterally to the mammary artery in the same intercostal space as the mini-thoracotomy. Several techniques were used for mitral valve repair, usually a combination of annuloplasty, leaflet resection and sliding, placement of neochordae and repair of the commissures. In cases of tricuspid valve surgery, we did not snare/clamp the cavae. Before performing the right atriotomy, the inferior venous cannula was pulled back to avoid a full blood drainage and, consequently, air suction. De-airing was performed with a ventricular vent and through the cardioplegia needle in case of external clamping or through the endoaortic balloon lumen.
Study design
Retrospective evaluation of prospectively collected data of a series of 258 consecutive patients who had minimally invasive cardiac surgery.
Statistical analysis
Continuous variables were presented as mean ± SD and analyzed using Student’s t-test. Categorical variables were expressed as absolute numbers and percentages and analyzed using chi-square test or, when appropriate, Fisher’s exact test. EAO group and external cross-clamping group were compared by means of preoperative patients’ characteristics, operative data and postoperative outcomes. Univariate analysis included 17 perioperative risk factors to determine whether any single variable influenced the occurrence of a new postoperative neurologic deficit, new postoperative cerebral stroke and hospital mortality. These variables were age, gender, redo operation, left ventricular ejection fraction (LVEF) <50%, hypertension, diabetes mellitus, hypercholesterolemia, renal dysfunction [estimated glomerular filtration rate (eGFR) <85 mL/min], hemodialysis, atrial fibrillation history, pulmonary hypertension [pulmonary artery pressure (PAPs) >30 mmHg), EAO technique, mitral valve replacement (against mitral valve repair), conversion to sternotomy, CPB time, cardioplegic arrest time, first procedures for each technique of cardioplegic arrest (first 50 cases considered as initial learning curve). Each variable with a value of P<0.05 was entered in a multiple logistic regression analysis model to study its independent predictability.
Results
Demographic data
Two-hundred fifty-eight patients were included in the study. Since the beginning of our experience, there was a liberal use of EAO and TTC according to surgeon’s preference. More recently, patients were operated predominantly on aortic cross-clamping; endoaortic balloon was reserved to redo operations. TTC was used in 165 patients (group TTC; mean age 62.8±13.1 years, male 53%); EAO was used in ninety-three patients (group EAO; mean age 56.1±14.5 years, male 50%). Apart from age, TTC patients were significantly older compared to EAO patients and the only difference between the two groups was the prevalence of redo procedures that were mostly accomplished by EAO (TTC =2% vs. EAO =12%, P=0.0018). All the patients but two (1 = redo case with refractory pulmonary edema due to mitral valve prosthesis dysfunction, 2 = acute massive mitral regurgitation with refractory pulmonary edema) were operated in an elective setting, including patients transferred by cardiology units after a recent episode of heart failure. Table 1 includes details about preoperative patient characteristics of the overall population of 258 patients and the two groups.

Full table
Operations performed
Mitral valve operations were associated with other procedures in 26% of the patients (n=68), particularly in 50 cases where tricuspid annuloplasty was also performed (19%). No difference between the two groups was found according to the types of operation. There was a significantly higher rate of mitral valve repair in TTC (TTC 70% vs. EAO 58%, P=0.04). However, when redo operations were excluded from analysis, this data retained no significance (TTC 68% vs. EAO 60%, P=0.19). CPB time and cardioplegic arrest time were similar in both groups. Table 2 summarizes all the operative data of the global population and the two groups.
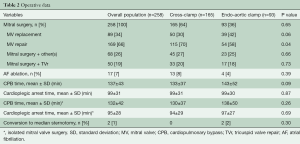
Full table
Perioperative outcomes
We found no difference in cardiac enzyme release with similar troponin I and CK-Mb at postoperative day 1. There were no cases of aortic dissection and femoral vessel complications. Patients who underwent EAO experienced a significantly higher rate of new postoperative cerebral stroke (TTC 0% vs. EAO 4.3%; P=0.03). Overall mortality was 1.9% (n=5) and mortality for primary operations was 1.2% (n=3). There was no difference in 30-day mortality between the two groups. Table 3 reports details of all perioperative outcomes.
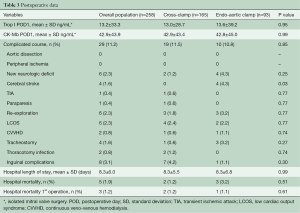
Full table
Univariate and multivariate analysis
Univariate analysis found significant risk factors for new neurologic deficit: mitral valve replacement (against mitral valve repair), P=0.0035; CPB times, P=0.00008; cardioplegic arrest time, P=0.004. None of these variables retained significance after multivariate analysis.
Use of EAO (P=0.03) and CPB times (P=0.02) were significantly associated with new postoperative cerebral stroke at univariate analysis. No significance was found at multivariate analysis.
Reoperation (P=0.01), pulmonary hypertension/PAPs >30 mmHg (P=0.02) and CPB time (P=0.02) were associated at univariate analysis with 30-day mortality. After multivariate analysis, no significance was found.
Discussion
Minimally invasive mitral valve surgery is gaining full credit after a couple of decades of skepticism received from the vast majority of cardiac surgeons. While reduction of surgical incision through a small thoracotomy is a common element for all minimally invasive approaches, perfusion, cardioplegia strategy and aortic occlusion techniques may vary according to surgeon preference and specific training. In this report, we describe our experience on aortic occlusion strategy comparing EAO with external trans-thoracic clamp. This comparison is relatively uncommon, as surgeons and centers usually adopt only one technique and do not master both aortic occlusion strategies. Although the proportion of external cross-clamping was higher in our cohort, the number of cases performed with endoaortic balloon is relatively high, documenting good and consistent experience.
We did not observe any difference in clinical outcomes with one technique over the other. Endoaortic balloon use was associated with increased risk of stroke, although after multivariable adjustment, endoaortic balloon was not predictive of stroke occurrence. There is, however, a rationale for increased stroke risk with the endoaortic technique because distal dislodgement of the balloon may lead to occlusion of the innominate artery; this complication is generally avoided by bilateral radial artery pressure monitoring and cerebral oximetry based on near-infrared spectroscopy (NIRS) evaluation. In contrast to other reports (3-5), endoaortic balloon utilization in our study was not associated with longer CPB and cross-clamp time, indicating that with adequate training this technique does not increase the complexity and the duration of the operations (6). While with the endoaortic balloon time is required to position the tip of the catheter in the ascending aorta under TOE guidance, with the external clamp, a cardioplegia cannula must be placed in the ascending aorta and sometimes repair of the needle-hole is cumbersome and time-consuming.
We did not observe any iatrogenic aortic dissection. This was a feared complication in the early era of minimally invasive mitral valve surgery, particularly with the endoaortic balloon (7). Two recent meta-analyses detected an increased incidence of acute iatrogenic aortic dissection when endoaortic balloon is used in minimally invasive cardiac surgery (3,4). In our cohort, both groups used retrograde perfusion through the femoral artery and perfusion pressure were constantly monitored throughout the operation, with particular emphasis at the beginning of CPB, before cross-clamping of the aorta. With the endoaortic balloon catheter occupying part of the cannula lumen, there is a substantial risk of having high jet pressures at the exit of the cannula. When perfusion pressure within the femoral artery line exceeded 200 mmHg, simple adjustments were initially made (i.e., repositioning of the arterial cannula, use of vasodilators); if adjustments did not produce a significant reduction of perfusion pressures, then the other femoral artery was isolated and cannulated splitting arterial perfusion in both arteries and thus obtaining a remarkable pressure reduction. Avoiding extremely high jet pressures from the femoral cannula is essential in preventing retrograde aortic dissection, particularly in patients with atherosclerotic disease and explains why this is not an observed complication nowadays.
Some concerns exist regarding satisfactory myocardial protection with the two settings of aortic occlusion and cardioplegia delivery (8,9). In our experience, myocardial damage expressed as cardiac enzymes release was not influenced by aortic occlusion technique. Monodose crystalloid cardioplegia was preferably utilized with the endoaortic technique because balloon positioning in the ascending aorta can only be visualized by TOE when the left atrium is closed, therefore subsequent doses of intermittent cardioplegia may lead to dislodgment of the endoaortic balloon and inadequate myocardial protection. In the external transthoracic clamp cases, intermittent cold blood cardioplegia has been preferred to avoid further hemodilution. We have previously demonstrated that both crystalloid and cold blood cardioplegia solutions provide adequate protection in minimally invasive cardiac surgery (10).
Exposure of the mitral valve is generally well accomplished with both aortic occlusion strategies. Mitral repair rate was significantly higher in the external cross-clamping group, but this was probably just a casual finding. The use of thoracoscopy and video assistance has become a fundamental part of the technique, particularly since the implementation of 3D endoscopy; it remarkably improves the mitral valve visualization and repair possibilities. The absence of transthoracic clamping and cardioplegia cannulation may facilitate thoracoscopy positioning and visualization.
Apart from the common contraindication for EAO, in case of an ascending aorta diameter greater than 40 mm, the choice between the two techniques of aortic occlusion was based mainly on operator preference and naturally affected patient selection. This is clearly underlined by the significant difference in age and in the rate of redo operations between the two groups. Elderly patients may exhibit atherosclerotic disease of the peripheral arteries and the thoraco-abdominal aorta, thus justifying the use of transthoracic cross-clamp. On the other hand, the use of EAO allows an even smaller surgical access, being more appealing in the young for aesthetic reasons and less traumatic in frail patients. Furthermore, the EAO system provides fundamental technical advantages in avoiding tissue dissection and is our first choice in redo operations.
Our results showed that EAO and aortic cross-clamping proved to be safe and effective. There was a higher rate of perioperative stroke in the EAO group, but it was statistically non-significant. Rather than looking for the superiority of one of these two techniques, we reported the advantage given by the possibility of handling both endoaortic occlusion and transthoracic clamping and the availability of tailoring the surgical strategy according to individual patient characteristics.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Casselman FP, Van Slycke S, Wellens F, et al. Mitral valve surgery can now routinely be performed endoscopically. Circulation 2003;108 Suppl 1:II48-54. [Crossref] [PubMed]
- Modi P, Hassan A, Chitwood WR Jr. Minimally invasive mitral valve surgery: a systematic review and meta-analysis. Eur J Cardiothorac Surg 2008;34:943-52. [Crossref] [PubMed]
- Kowalewski M, Malvindi PG, Suwalski P, et al. Clinical Safety and Effectiveness of Endoaortic as Compared to Transthoracic Clamp for Small Thoracotomy Mitral Valve Surgery: Meta-Analysis of Observational Studies. Ann Thorac Surg 2017;103:676-86. [Crossref] [PubMed]
- Khan H, Hadjittofi C, Uzzaman M, et al. External aortic clamping versus endoaortic balloon occlusion in minimally invasive cardiac surgery: a systematic review and meta-analysis. Interact Cardiovasc Thorac Surg 2018;27:208-14. [PubMed]
- Mazine A, Pellerin M, Lebon JS, et al. Minimally invasive mitral valve surgery: influence of aortic clamping technique on early outcomes. Ann Thorac Surg 2013;96:2116-22. [Crossref] [PubMed]
- Casselman F, Aramendi J, Bentala M, et al. Endoaortic Clamping Does Not Increase the Risk of Stroke in Minimal Access Mitral Valve Surgery: A Multicenter Experience. Ann Thorac Surg 2015;100:1334-9. [Crossref] [PubMed]
- Mohr FW, Falk V, Diegeler A, et al. Minimally invasive port-access mitral valve surgery. J Thorac Cardiovasc Surg 1998;115:567-74; discussion 574-6. [Crossref] [PubMed]
- Bentala M, Heuts S, Vos R, et al. Comparing the endo-aortic balloon and the external aortic clamp in minimally invasive mitral valve surgery. Interact Cardiovasc Thorac Surg 2015;21:359-65. [Crossref] [PubMed]
- Ius F, Mazzaro E, Tursi V, et al. Clinical results of minimally invasive mitral valve surgery: endoaortic clamp versus external aortic clamp techniques. Innovations (Phila) 2009;4:311-8. [Crossref] [PubMed]
- De Palo M, Guida P, Mastro F, et al. Myocardial protection during minimally invasive cardiac surgery through right mini-thoracotomy. Perfusion 2017;32:245-52. [Crossref] [PubMed]






