Short-term mechanical circulatory support as bridge to heart transplantation: paracorporeal ventricular assist device as alternative to extracorporeal life support
Abstract
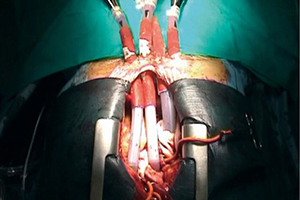
Extracorporeal life support (ECLS) is generally considered to be the treatment of choice for bridging to heart transplantation (HTx) patients with cardiogenic shock; however, alternative mechanical circulatory support (MCS) devices have been proposed with satisfactory results and, among those, paracorporeal systems have demonstrated to be safe and effective. This technology has been used for decades as bridge to transplant, especially in patients with advanced right ventricular dysfunction or evidence of multiorgan failure (MOF), which could be difficult to manage with an isolated left ventricular support. Paracorporeal systems are defined by having the pump located outside of the body, with inflow and outflow cannulas that traverse the skin connecting the pump with the heart and great vessels. They can be utilised in a uni- or bi-ventricular configuration and can provide pulsatile or continuous flow, depending on the device technology (pneumatic vs. centrifugal). In particular, pneumatic devices allow for patient mobilization and hospital discharge, improving rehabilitation and organ recovery while bridging to transplant. In our institution at the University Hospital of Udine, 34 pneumatic paracorporeal ventricular assist devices (VADs) have been implanted since 1998: in most cases (32 pts), as biventricular support for patients in INTERMACS class I–II. After a median support time of 34 (range, 0–385) days, with 19 patients (56%) supported for more than 1 month, 23 patients (68%) underwent HTx and 3 (9%) were successfully weaned to hospital discharge, resulting in an overall combined 76% survival to HTx or weaning. After transplant, the survival rate was similar to the one of the patients not bridged with MCS. In conclusion, pneumatic VADs can effectively assist patients with severe biventricular failure, especially those with contraindications to ECLS or expected long waiting times for HTx. Moreover, they can potentially result in hospital discharge, optimal organ and patient recovery and donor-recipient matching, resulting in a satisfactory transplant outcome.
Cover