Robotic thymectomy for myasthenia gravis
Introduction
The outcomes of thymectomy and their association with surgical technique remain debatable. The outcomes depend not only on the molecular basis of the disease, such as the level of various antibodies, but also on the pathology of the gland. For instance, thymic follicular hyperplasia patients tend to benefit more from thymectomy (1). Moreover, thymectomy may alter the disease severity or induce remission (1). The best outcomes are typically observed in severe thymic hyperplasia patients who undergo thymectomy soon after the disease onset (2,3).
The therapeutic effect of thymectomy may be attributable to the elimination of main production sites of anti-acetylcholine receptor (AChR) autoantibody. Several minimally invasive methods have been used to perform thymectomy in myasthenia gravis (MG) patients. We prefer right-sided video-assisted thoracoscopic surgery (VATS) or robot-assisted thoracoscopic surgery (RATS) for thymectomy. Here, we describe RATS thymectomy along with a video presentation (Video 1).
Clinical vignette
The patient is a 45-year-old male with MG. His clinical findings are supported by electromyography findings and AChR-ab levels, which are higher than the upper limit of the reference range. Chest computed tomography did not reveal thymoma but minimal hyperplasia. His clinical condition corresponded to Myasthenia Gravis Foundation of America (MGFA) Grade IIIB (Table 1). The patient was prescribed pyridostigmine bromide (60 mg thrice a day) and corticosteroids. He was referred to the department of thoracic surgery for minimally invasive thymectomy. He was scheduled for a right-sided RATS procedure. On the morning of the surgery, he took 60 mg pyridostigmine bromide and 40 mg corticosteroid.
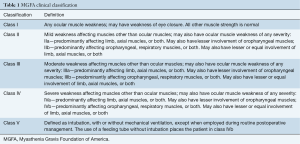
Full table
Surgical technique
Preparation
We prefer a right-sided approach for robotic thymectomy because of the larger space and easy access to the superior vena cava and both innominate veins. The patient is positioned 30° semi-supine and supported with a roll placed under the right shoulder. The right arm is draped and positioned inferior to the chest.
Exposition
Three ports are used in our technique. We do not open an access port if the operation is not performed for thymoma. For thymoma resections, the left port, which is located inside the pectoralis muscles, is enlarged and an Alexis retractor (Applied Medical, Rancho Santa Margarita, CA, USA) is placed. The incisions are placed around the breast without violating the mammary tissue. The first port is always the camera port, and the 30° up camera is used while placing other ports. During the operation, the 30° cameras, either up or down, could be used. While working under the sternum, the 30° up camera is a good choice, whereas while working at the left thymus side and inside the left pleural cavity near the left phrenic nerve, the 30° down camera is a good choice. The left port is opened in the pectoralis major muscle anterior to the axillary fossa. The right port is opened in the fifth or sixth intercostal space under the breast fold. After placement of the ports, side docking of the robot is performed (da Vinci SI Systems Intuitive Surgical, Sunnyvale, CA, USA).
Operation
We use CO2 insufflation with 8 mmHg pressure until the contralateral pleura is opened. We use a prograsper (Intuitive Inc., Sunnyvale, CA, USA) for the left arm and Maryland bipolar forceps (Intuitive Inc., Sunnyvale, CA, USA) for the right arm. After careful exploration of the right thoracic cavity, we begin dissection and perform resection of right-sided pericardiophrenic fatty tissue. It is separated from the diaphragm, pericardium, and sternum by dividing the vessels originating from the distal internal mammary vessels.
Thymus resection begins by dissecting the thymus from the pericardium, anterior to the right phrenic nerve. This dissection may either be blunt or performed with the Maryland forceps. The dissection of the thymus from the sternum may or may not require opening of the contralateral mediastinal pleura. The dissection of the superior vena cava around the phrenic nerve enables visualization of the superior vena cava and the junction of both innominate veins. The dissection of the angle between the phrenic nerve, superior vena cava, and sternum deserves the highest attention in this operation. This location is a trap for vascular or neural injury (particularly phrenic nerve) even in simple thymectomy.
The dissection of the upper thymic poles requires extra caution. The capsule of the thymus is separated from the peripheral fatty and connective tissue. The denuded superior poles are separated from their attachments to the thyrothymic ligament by gentle caudal traction. The artery and venous branches feeding the thymus are identified and divided during this maneuver. There is considerable variability with respect to the number and/or location of the major thymic veins. Extra caution is needed to divide them carefully without causing hemorrhage. After complete dissection of the upper poles, thymus is retracted caudally, which renders it completely free from the left innominate vein. Attachment of clips to the thymus capsule may cause unexpected incidental bleeding from the left innominate vein. If not opened until this part of the operation, the contralateral mediastinal pleura could be opened. We prefer to resect both mediastinal pleura and keep them on the specimen.
The left side of the thymus is dissected from the pericardium by pulling the thymic tissue toward the surgeon with the left arm. The left phrenic nerve is visualized with the help of the 30° down camera, and extreme caution is required to prevent thermal or mechanical injury.
Completion
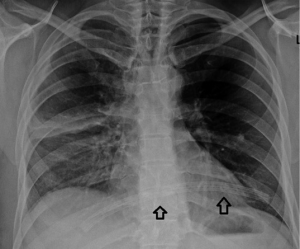
After completion of the dissection and resection of the left thymus, fatty tissue located at the left pericardiophrenic angle is completely resected. After completion of the operation, the left phrenic nerve is examined to ensure that there is no injury. A Jackson Pratt drain is placed transmediastinally to the left hemi thoracic cavity to drain both the pleural cavities (Figure 1).
Comment
Minimally invasive thymectomy is associated with less blood loss, shorter postoperative hospital stay, and decreased need for narcotic analgesics compared to open surgery. Moreover, the long-term outcomes, such as quality of life, are better or at least similar to those of open surgery (4).
Robotic thymectomy could be one of the most dangerous operations if performed by an unexperienced surgeon. Even surgeons who have extensive experience in minimally invasive thymic surgery may face catastrophic complications, such as cardiac arrest and rupture of the aorta or superior vena cava (5). Other common complications of thoracic surgery may also occur.
A potential problem for many surgeons using a right-sided approach is inadequate visualization of the left phrenic nerve. During thymectomy, the left phrenic nerve should be identified and dissected meticulously to prevent any injury. Especially, in obese patients (body mass index >35 kg/m2), the left phrenic nerve may not be easily identified and evaluated owing to excessive fatty tissue. Surgeons may consider a bilateral approach in such patients.
We have been performing VATS thymectomy for more than 16 years and total number of VATS thymectomy operations are over 500 patients in Istanbul University, Istanbul Medical School and Group Florence Nightingale Hospitals. When we are operating on a patient with severe MG and there is a risk for postoperative prolonged intubation, we prefer to perform VATS thymectomy, as the duration of a VATS thymectomy operation is generally shorter when compared to a robotic thymectomy operation. The other reason for selection of robotic thymectomy is suitability of insurance and economic conditions. As the robotic thymectomy costs higher than the VATS thymectomy, some patients prefer to have VATS thymectomy.
We have fewer left-sided approach experiences. These are limited to the patients who had a previous surgery from the right thoracic cavity and totally left sided located thymoma patients. When the patient is myasthenic, and has a left sided thymoma, we still prefer right sided thymectomy and generally perform bilateral approach if the thymoma is close to the left phrenic nerve.
Robotic thymectomy for the treatment of MG is a safe procedure. The potential dangerous operative and postoperative complications should be kept in mind, and appropriate management strategies adopted to prevent severe morbidity and mortality.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Spillane J, Hayward M, Hirsch NP, et al. Thymectomy: role in the treatment of myasthenia gravis. J Neurol 2013;260:1798e801.
- Budde JM, Morris CD, Gal AA, et al. Predictors of outcome in thymectomy for myasthenia gravis. Ann Thorac Surg 2001;72:197e202.
- Nieto IP, Robledo JP, Pajuelo MC, et al. Prognostic factors for myasthenia gravis treated by thymectomy: review of 61 cases. Ann Thorac Surg 1999;67:1568e71.
- Bachmann K, Burkhardt D, Schreiter I, et al. Long-term outcome and quality of life after open and thoracoscopic thymectomy for myasthenia gravis: analysis of 131 patients. Surg Endosc 2008;22:2470-7. [Crossref] [PubMed]
- Toker A, Tanju S, Ziyade S, et al. Early outcomes of video-assisted thoracoscopic resection of thymus in 181 patients with myasthenia gravis: who are the candidates for the next morning discharge? Interact Cardiovasc Thorac Surg 2009;9:995-8. [Crossref] [PubMed]