Comparison of SynCardia total artificial heart and HeartWare HVAD biventricular support for management of biventricular heart failure: a systematic review and meta-analysis
Abstract
Background: The aim of this study was to compare the outcomes of patients undergoing SynCardia total artificial heart (TAH) and biventricular HeartWare ventricular assist device (Bi-HVAD) support for biventricular heart failure (HF).
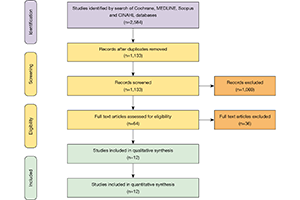
Methods: Electronic search was performed to identify all relevant studies detailing patients who underwent biventricular assist device implantation using Bi-HVAD devices and those who underwent TAH placement for biventricular HF. Twelve studies including 512 patients in the TAH group versus 38 patients in the Bi-HVAD group were pooled for meta-analysis.
Results: Ischemic cardiac etiology was present in 32% (95% CI, 24–47) of TAH vs. 15% (95% CI, 4–44) of Bi-HVAD patients (P=0.21). There was a comparable incidence of stroke [TAH 11% (95% CI, 7–16) vs. Bi-HVAD 13% (95% CI, 2–51), P=0.86] and acute kidney injury [TAH 28% (95% CI, 2–89) vs. Bi-HVAD 27% (95% CI, 9–59), P=0.98]. Overall infection rate was 67% (95% CI, 47–82) in TAH and 36% (95% CI, 10–74) in Bi-HVAD (P=0.16). Driveline infections were comparable between the two groups [TAH 11% (95% CI, 6–19) vs. Bi-HVAD 8% (95% CI, 1–39), P=0.73] and although a higher incidence of mediastinitis was found in the Bi-HVAD group [TAH 4% (95% CI, 2–7) vs. Bi-HVAD 15% (95% CI, 4–45), P=0.07] there was no statistically significant difference between the groups. Postoperative bleeding was present in 42% (95% CI, 28–58) of TAH vs. 23% (95% CI, 8–52) of Bi-HVAD (P=0.22). Patients in the TAH group had shorter duration of support [TAH 71 days (95% CI, 15–127) vs. Bi-HVAD 167 days (95% CI, 116–217), P=0.01]. At the mean follow-up time of 120 days, (95% CI, 83–157) patients in both groups had similar overall mortality [TAH 36% (95% CI, 22–49) vs. Bi-HVAD 26% (95% CI, 6–46), P=0.44] including mortality on device support [TAH 26% (95% CI, 17–36) vs. Bi-HVAD 21% (95% CI, 4–37), P=0.55]. Discharge home on support was achieved in 6% (95% CI, 4–17%) of TAH patients vs. 73% (95% CI, 48–89%) of Bi-HVAD (P<0.01), and 68% (95% CI, 52–84) of TAH patients were transplanted vs. 61% (95% CI, 47–75) in the Bi-HVAD group (P=0.14).
Conclusions: Patients on Bi-HVAD support were more likely to be able to be discharged home on support and had similar overall mortality to TAH, albeit with much longer duration of support.
Cover