Long-term outcomes of the frozen elephant trunk procedure: a systematic review
Introduction
Combining the advantages of the classical elephant trunk with modern stent technology, the frozen elephant trunk (FET) procedure has been instrumental in treating complex multi-segmental aortic pathologies in a single operation. The secured expansile stent-graft is able to facilitate downstream aortic remodelling by inducing false lumen thrombosis and depressurization of the false lumen, stabilize the dissecting membrane, and limit stent-graft migration and proximal type Ia endoleaks (1,2). While multiple meta-analyses have reaffirmed the relatively safe short-term profiles of these devices, much less is known regarding long-term outcomes, particularly in terms of overall survival and freedom from reintervention (3-7). The present meta-analysis aimed to determine long-term outcomes following the FET procedure.
Methods
Literature search strategy
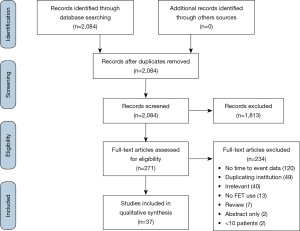
Electronic searches were performed using Ovid Medline, Embase, Scopus, and PubMed, from their date of inception to October 2019. To achieve maximum sensitivity of the search strategy, the terms ‘elephant trunk’, ‘Thoraflex’, ‘E-vita’, ‘Gianturco Z’, ‘Chavan-Haverich’, or ‘Cronus’ were used as either keywords or MeSH terms. Determination of whether the descending endoprosthesis was stented (i.e., ‘frozen’) or not (i.e., conventional elephant trunk) was made upon full article review. The reference lists of all included studies were reviewed for further identification of other potentially relevant studies. All identified articles were systematically assessed using the inclusion and exclusion criteria.
Selection criteria
Eligible studies for the present systematic review included those which (I) examined the use of FETs, (II) had clinical follow-up data of at least 12 months, and (III) had at least 10 patients. The FET is required to be deployed via open surgery in an antegrade fashion into the proximal descending aorta, and secured at the proximal aspect by sutures. No distinction was made regarding the management of head and neck vessels. All publications were limited to those involving human subjects and in the English language. Abstracts, case reports, conference presentations, editorials, and expert opinions were excluded. Review articles were omitted because of potential publication bias and duplication of results. Primary endpoint was overall survival. Secondary outcomes included freedom from reintervention, freedom from aortic events, 30 day/in-hospital mortality, stroke/permanent neurological damage, spinal cord damage, temporary neurological deficit, acute kidney injury, and hospital and intensive care unit (ICU) length of stay.
Data extraction and critical appraisal
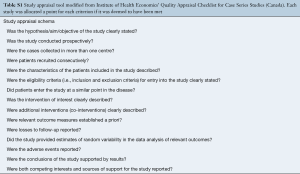
All data were extracted from article texts, tables and figures. Two investigators (Y.J., H.H.) independently reviewed each retrieved article. Discrepancies between the two reviewers were resolved by the senior investigator (D.H.T.). Quality assessment was assessed using a modified schema used for assessing case series, developed by the Institute of Health Economics (Alberta, Canada) (8) (Table S1). This schema examines the suitability of study objective, design, population, intervention, outcome measure, statistical analysis, appropriateness of results and conclusions, and competing interests (Table S1). Each study was scored out of 15 points, with 13–15 representing high-quality, 10–12 as medium-quality, and less than 10 as low-quality.
Full table
Statistical analysis
Descriptive statistics were calculated for all collected variables. Categorical or continuous variables were aggregated using meta-analysis of proportions or means, as appropriate. Data is presented as N (%) or mean ± standard deviation (SD). Where continuous values are presented in median with range or interquartile ranges they were converted to mean and SD using methods published by Wan and colleagues (9). Guyot’s iterative algorithm was applied to digitized Kaplan-Meier curves to reconstruct individual patient data (10,11). This approach assumed a constant, non-informative censoring mechanism. The reconstructed patient data were then aggregated to form the combined survival curve. The estimated survival for a 57-year-old male in 2010, representing the median age, sex, and study period of all studies, is also plotted to represent general population survival curve. The American life tables were selected arbitrarily (Center for Disease Control, United States). All p-values were two-sided, and p-values less than 0.05 were considered statistically significant. All statistics were performed with R (version 3.3.5, R Core Team, Vienna, Austria).
Results
Literature search
Overall 2,084 records were identified from the literature search (Figure S1). Following review (1,2,12-29), 37 were included in the quantitative analysis with a total of 4,178 patients (Table S2) (30-46). No further studies were identified from review of references. Three studies were multi-center studies (12,14,42), including an international registry (14). The median size of included studies was 58 patients (interquartile range, 34–120). Most studies were published by Chinese centers (12 studies), followed by German (8 studies) and Japanese centers (7 studies). Median duration of study was 7 years, with average follow-up of 3.2 years.
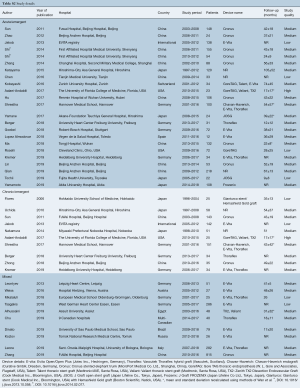
Full table
Patient characteristics
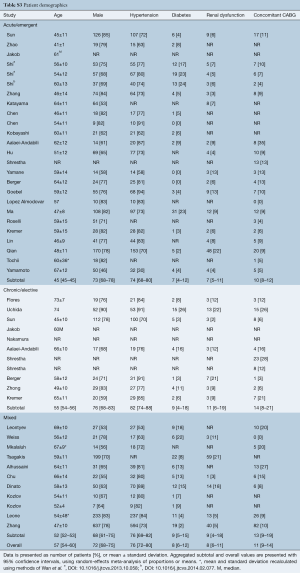
FETs were used exclusively for acute dissections in 23 studies involving 1,801 patients. In 10 studies the patient cohorts were chronic dissections or elective surgeries (698 patients). In the remaining studies there was a mixture of emergent and elective indications. A variety of stent-grafts were used, including E-Vita Open/E-Vita Open Plus (13 studies), Cronus (10 studies), Thoraflex (6 studies), GORE TAG (3 studies), Valiant (2 studies), Medtronic TX2 (2 studies), JSOG (2 studies), as well as Frozenix (1 study), Gianturco stent/Hemashield Gold graft (1 study), and Chavan-Haverich (1 study).
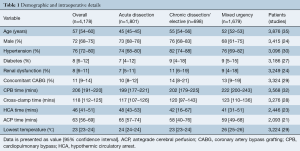
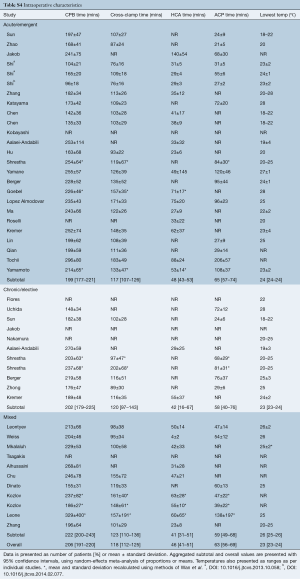
Average age of included patients was 57 years old (IQR, 54–60 years), with 72% males (Tables 1,S3). The majority of patients were hypertensive (76%), with a small proportion having diabetes (8%), and renal dysfunction (8%). Other comorbidities, such as respiratory dysfunction, Marfan’s syndrome, previous surgery, were insufficiently reported. Average cardiopulmonary bypass and cross-clamp times were 206 minutes and 118 minutes, respectively (Table S4). Average hypothermic circulatory arrest time was 46 minutes with antegrade cerebral perfusion time of 63 minutes (where reported). Circulatory arrest occurred at 23 °C on average.
Full table
Full table
Full table
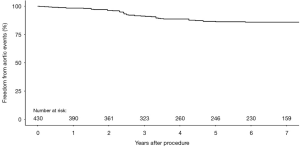
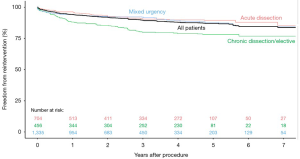
Overall survival
Overall survival at 1-, 2-, 3-, 5-, and 10-year were 89.6%, 87.1%, 85.2%, 82.0%, and 68.0%, respectively (Figure 1). Survival at 1-, 2-, 3-, 5-, and 10-year for studies that reported only acute dissections were 90.7%, 88.3%, 86.1%, 83.9%, and 73.5%, compared to 90.0%, 87.4%, 85.2%, 79.1%, and 56.0% for studies that only included chronic dissections/elective aneurysmal patients. Freedom from reintervention at 1-, 2-, 3-, and 5-year were 93.9%, 91.6%, 89.3%, and 86.8%, respectively (Figure 2). Freedom from aortic events at 1-, 2-, 3-, and 5-year were 98.3%, 96.2%, 91.3%, and 86.6%, respectively (Figure 3).

Secondary outcomes
Pooled in-hospital/30-day mortality was 10.2% (Tables 2,S5). Permanent neurological deficit and spinal cord injury were 7.7% and 6.5%, respectively. Acute kidney injury, with varying definitions, was 15.5%. There were insufficient data to evaluate temporary neurological deficit and hospital and ICU length of stay.
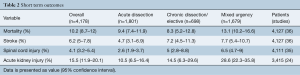
Full table
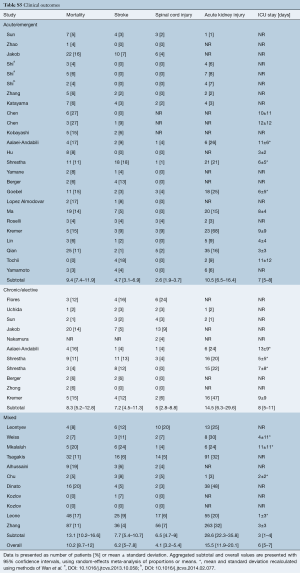
Full table
Quality assessment
The majority of studies were assessed to be medium-quality, with one high-quality and seven low-quality studies. Almost all of the studies were retrospective, single center trials, with no predetermined definitions of clinical outcomes. Loss to follow-up and the consecutive nature of patient enrolment were also inconsistently reported.
Discussion
The present systematic review examined long-term outcomes of the FET technique. Aggregation of Kaplan-Meier curves found overall survival at 1-, 3-, and 5-year were 89.6%, 85.2%, and 82.0%, respectively. In comparison, patients who received planned second-stage procedures after a classic elephant trunk had a 3-year survival rate of 75% (47). Indeed, the interval mortality between the first-stage and second-stage completion procedures ranges between 2–11% (48), with the latter operation greatly precluded by the use of the FET. Furthermore, it has been shown that a patent false lumen in the descending aorta is a predictor for late mortality and need for reintervention due to aortic expansion (49,50). In a meta-analysis of 11 cohort studies, residual patent false lumen was found to increase the risk of late mortality and aortic events in type A dissections by 71% and 179%, respectively (50). The FET’s ability to promote downstream remodelling and induce false lumen thrombosis has been well validated (2,6), therefore providing an attractive option for management of such pathologies.
The need for reintervention after the FET procedure is not negligible. The ideal length of FET remains controversial, requiring careful balance between sufficient length to achieve adequate distal false lumen occlusion and minimizing occlusion of vascular collaterals that supply the spinal cord. As such, it is often not possible to provide full distal coverage of the aortic pathology due to fear of spinal cord ischemia, thereby necessitating a second-stage procedure despite the use of FETs (43,51). However, it should be noted that the FET simplifies such reinterventions by providing a more appropriate landing zone for endovascular completion (52,53). In the present review, freedom from reintervention at 1-, 3-, and 5-year was 93.9%, 89.3%, and 86.8%, respectively, reaffirming the need for close serial follow-up after the FET procedure.
There are several limitations to the present review that must be considered when interpreting these results. First, in order to attain sufficient statistical power and increase overall representativeness of the findings, this analysis included a heterogeneous cohort of patients, with varying comorbidities, pathologies, and surgical techniques. While subgroup classifications have been made based on clinical urgency, the assortment of surgical approaches, such as the extent of surgery, management of supra-aortic vessels (e.g., debranching procedures), neuroprotection strategies, and type and length of FETs is likely to have confounded results. Secondly, the volume of practice varied between hospitals, and particularly amongst geographic regions. Finally, the average length of follow-up is only 3.2 years, with limited data available beyond this period.
The present review demonstrates that survival after the FET procedure is favorable, though the need for reintervention still remains. Larger robust multi-institutional registries are required to elucidate the precise role of the FET in managing complex multisegmental aortic pathologies.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Shrestha M, Martens A, Kaufeld T, et al. Single-centre experience with the frozen elephant trunk technique in 251 patients over 15 years. Eur J Cardiothorac Surg 2017;52:858-66. [Crossref] [PubMed]
- Berger T, Kreibich M, Morlock J, et al. True-lumen and false-lumen diameter changes in the downstream aorta after frozen elephant trunk implantation. Eur J Cardiothorac Surg 2018;54:375-81. [Crossref] [PubMed]
- Koullias GJ, Wheatley GH 3rd. State-of-the-art of hybrid procedures for the aortic arch: a meta-analysis. Ann Thorac Surg 2010;90:689-97. [Crossref] [PubMed]
- Tian DH, Wan B, Di Eusanio M, et al. Short- and medium-term outcomes of the frozen elephant trunk technique in aortic arch surgery: A systematic review. Heart, Lung and Circulation 2015;24:e58-9. [Crossref]
- Lin HH, Liao SF, Wu CF, et al. Outcome of frozen elephant trunk technique for acute type A aortic dissection: as systematic review and meta-analysis. Medicine (Baltimore) 2015;94:e694. [Crossref] [PubMed]
- Takagi H, Umemoto T. A Meta-Analysis of Total Arch Replacement with Frozen Elephant Trunk in Acute Type A Aortic Dissection. Vasc Endovascular Surg 2016;50:33-46. [Crossref] [PubMed]
- Papakonstantinou NA, Antonopoulos CN, Baikoussis NG, et al. Frozen Elephant Trunk: An Alternative Surgical Weapon Against Extensive Thoracic Aorta Disease. A Three-Year Meta-Analysis. Heart Lung Circ 2019;28:213-22. [Crossref] [PubMed]
- (IHE). IoHE. Quality Appraisal of Case Series Studies Checklist. Edmonton (AB): Institute of Health Economics, 2014.
- Wan X, Wang W, Liu J, et al. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 2014;14:135. [Crossref] [PubMed]
- Guyot P, Ades A, Ouwens MJ, et al. Enhanced secondary analysis of survival data: reconstructing the data from published Kaplan-Meier survival curves. BMC Med Res Methodol 2012;12:9. [Crossref] [PubMed]
- Saluja R, Cheng S. Estimating hazard ratios from published Kaplan-Meier survival curves: A methods validation study. Res Synth Methods 2019;10:465-75. [Crossref] [PubMed]
- Sun L, Qi R, Zhu J, et al. Total arch replacement combined with stented elephant trunk implantation: a new "standard" therapy for type a dissection involving repair of the aortic arch? Circulation 2011;123:971-8. [Crossref] [PubMed]
- Zhao HP, Zhu JM, Ma WG, et al. Total arch replacement with stented elephant trunk technique for acute type B aortic dissection involving the aortic arch. Ann Thorac Surg 2012;93:1517-22. [Crossref] [PubMed]
- Jakob H, Tsagakis K. International E-vita open registry. Ann Cardiothorac Surg 2013;2:296-9. [PubMed]
- Shi E, Gu T, Yu Y, et al. Early and midterm outcomes of hemiarch replacement combined with stented elephant trunk in the management of acute DeBakey type I aortic dissection: comparison with total arch replacement. J Thorac Cardiovasc Surg 2014;148:2125-31. [Crossref] [PubMed]
- Shi E, Gu T, Yu Y, et al. Simplified total arch repair with a stented graft for acute DeBakey type I dissection. J Thorac Cardiovasc Surg 2014;148:2147-54. [Crossref] [PubMed]
- Zhang H, Lang X, Lu F, et al. Acute type A dissection without intimal tear in arch: proximal or extensive repair? J Thorac Cardiovasc Surg 2014;147:1251-5. [Crossref] [PubMed]
- Katayama A, Uchida N, Katayama K, et al. The frozen elephant trunk technique for acute type A aortic dissection: results from 15 years of experience†. Eur J Cardiothorac Surg 2015;47:355-60; discussion 360. [Crossref] [PubMed]
- Chen Q, Cheng F, Chen T, et al. Ascending aorta replacement combined with open placement of triple-branched stent graft and total arch replacement combined with stented elephant trunk implantation for treating type A aortic dissection. Int J Clin Exp Med 2016;9:16070-7.
- Kobayashi M, Chaykovska L, van der Loo B, et al. Long-term results of simplified frozen elephant trunk technique in complicated acute type A aortic dissection: A case-control study. Vascular 2016;24:523-30. [Crossref] [PubMed]
- Aalaei-Andabili SH, Scali S, Klodell C, et al. Outcomes of Antegrade Stent Graft Deployment During Hybrid Aortic Arch Repair. Ann Thorac Surg 2017;104:538-44. [Crossref] [PubMed]
- Hu X, Wang Z, Ren Z, et al. Simplified total aortic arch replacement with an in situ stent graft fenestration technique for acute type A aortic dissection. J Vasc Surg 2017;66:711-7. [Crossref] [PubMed]
- Yamane Y, Uchida N, Mochizuki S, et al. Early- and mid-term aortic remodelling after the frozen elephant trunk technique for retrograde type A acute aortic dissection using the new Japanese J Graft open stent graft. Interact Cardiovasc Thorac Surg 2017;25:720-6. [Crossref] [PubMed]
- Goebel N, Nagib R, Salehi-Gilani S, et al. One-stage hybrid aortic repair using the frozen elephant trunk in acute DeBakey type I aortic dissection. J Thorac Dis 2018;10:4195-203. [Crossref] [PubMed]
- López Almodóvar LF, Lima Canadas P, Enriquez Puga A, et al. Single Low-Volume Center Experience with Frozen Elephant Trunk in Acute Type A Aortic Dissections. Aorta (Stamford) 2018;6:125-9. [Crossref] [PubMed]
- Ma M, Feng X, Wang J, et al. Acute Type I aortic dissection: a propensity-matched comparison of elephant trunk and arch debranching repairs. Interact Cardiovasc Thorac Surg 2018;26:183-9. [Crossref] [PubMed]
- Roselli EE, Idrees JJ, Bakaeen FG, et al. Evolution of Simplified Frozen Elephant Trunk Repair for Acute DeBakey Type I Dissection: Midterm Outcomes. Ann Thorac Surg 2018;105:749-55. [Crossref] [PubMed]
- Kremer J, Preisner F, Dib B, et al. Aortic arch replacement with frozen elephant trunk technique - a single-center study. J Cardiothorac Surg 2019;14:147. [Crossref] [PubMed]
- Lin Y, Ma WG, Zheng J, et al. Supra-aortic vessel reconstruction in total arch replacement for acute type A dissection: Comparison of en bloc and separate graft techniques. Asian J Surg 2019;42:482-7. [Crossref] [PubMed]
- Qian SC, Ma WG, Pan XD, et al. Renal malperfusion affects operative mortality rather than late death following acute type A aortic dissection repair. Asian J Surg 2020;43:213-9. [Crossref] [PubMed]
- Tochii M, Takami Y, Ishikawa H, et al. Aortic remodeling with frozen elephant trunk technique for Stanford type A aortic dissection using Japanese J-graft open stent graft. Heart Vessels 2019;34:307-15. [Crossref] [PubMed]
- Yamamoto H, Kadohama T, Yamaura G, et al. Total arch repair with frozen elephant trunk using the "zone 0 arch repair" strategy for type A acute aortic dissection. J Thorac Cardiovasc Surg 2019. [Epub ahead of print]. [PubMed]
- Flores J, Kunihara T, Shiiya N, et al. Extensive deployment of the stented elephant trunk is associated with an increased risk of spinal cord injury. J Thorac Cardiovasc Surg 2006;131:336-42. [Crossref] [PubMed]
- Uchida N, Shibamura H, Katayama A, et al. Long-term results of the frozen elephant trunk technique for the extensive arteriosclerotic aneurysm. J Thorac Cardiovasc Surg 2010;139:913-7. [Crossref] [PubMed]
- Nakamura K, Nagahama H, Nakamura E, et al. Predictors of early and late outcome after total arch replacement for atherosclerotic aortic arch aneurysm. Gen Thorac Cardiovasc Surg 2014;62:31-7. [Crossref] [PubMed]
- Zhong YL, Qi RD, Ma WG, et al. Frozen elephant trunk with modified en bloc arch reconstruction and left subclavian transposition for chronic type A dissection. J Thorac Dis 2018;10:5376-83. [Crossref] [PubMed]
- Leontyev S, Misfeld M, Daviewala P, et al. Early- and medium-term results after aortic arch replacement with frozen elephant trunk techniques-a single center study. Ann Cardiothorac Surg 2013;2:606-11. [PubMed]
- Weiss G, Santer D, Dumfarth J, et al. Evaluation of the downstream aorta after frozen elephant trunk repair for aortic dissections in terms of diameter and false lumen status. Eur J Cardiothorac Surg 2016;49:118-24. [Crossref] [PubMed]
- Mkalaluh S, Szczechowicz M, Mashhour A, et al. Total aortic arch replacement using elephant trunk or frozen elephant trunk technique: a case-control matching study. J Thorac Dis 2018;10:6192-200. [Crossref] [PubMed]
- Tsagakis K, Wendt D, Dimitriou AM, et al. The frozen elephant trunk treatment is the operation of choice for all kinds of arch disease. J Cardiovasc Surg (Torino) 2018;59:540-6. [PubMed]
- Alhussaini M, Abdelwahab A, Arnaoutakis GJ, et al. Neurologic Outcomes in Aortic Arch Repair With Frozen Elephant Trunk Versus 2-Stage Hybrid Repair. Ann Thorac Surg 2019;107:1775-81. [Crossref] [PubMed]
- Chu MWA, Losenno KL, Dubois LA, et al. Early Clinical Outcomes of Hybrid Arch Frozen Elephant Trunk Repair With the Thoraflex Hybrid Graft. Ann Thorac Surg 2019;107:47-53. [Crossref] [PubMed]
- Dinato FJ, Dias RR, Duncan JA, et al. The learning curve effect on outcomes with frozen elephant trunk technique for extensive thoracic aorta disease. J Card Surg 2019;34:796-802. [Crossref] [PubMed]
- Kozlov BN, Panfilov DS, Saushkin VV, et al. Distal aortic remodelling after the standard and the elongated frozen elephant trunk procedure. Interact Cardiovasc Thorac Surg 2019;29:117-23. [Crossref] [PubMed]
- Leone A, Di Marco L, Coppola G, et al. Open distal anastomosis in the frozen elephant trunk technique: initial experiences and preliminary results of arch zone 2 versus arch zone 3dagger. Eur J Cardiothorac Surg 2019;56:564-71. [Crossref] [PubMed]
- Zhang L, Yu C, Yang X, et al. Hybrid and frozen elephant trunk for total arch replacement in DeBakey type I dissection. J Thorac Cardiovasc Surg 2019;158:1285-92. [Crossref] [PubMed]
- Svensson LG, Kim KH, Blackstone EH, et al. Elephant trunk procedure: newer indications and uses. Ann Thorac Surg 2004;78:109-16; discussion 116. [Crossref] [PubMed]
- Safi HJ, Miller CC 3rd, Estrera AL, et al. Staged repair of extensive aortic aneurysms: morbidity and mortality in the elephant trunk technique. Circulation 2001;104:2938-42. [Crossref] [PubMed]
- Fattouch K, Sampognaro R, Navarra E, et al. Long-term results after repair of type a acute aortic dissection according to false lumen patency. Ann Thorac Surg 2009;88:1244-50. [Crossref] [PubMed]
- Li D, Ye L, He Y, et al. False lumen status in patients with acute aortic dissection: a systematic review and meta-analysis. J Am Heart Assoc 2016;5:e003172. [Crossref] [PubMed]
- Uchida N, Kodama H, Katayama K, et al. Endovascular aortic repair as second-stage surgery after hybrid open arch repair by the frozen elephant trunk technique for extended thoracic aneurysm. Ann Thorac Cardiovasc Surg 2013;19:257-61. [Crossref] [PubMed]
- Dias RR, Duncan JA, Vianna DS, et al. Surgical treatment of complex aneurysms and thoracic aortic dissections with the Frozen Elephant Trunk technique. Rev Bras Cir Cardiovasc 2015;30:205-10. [PubMed]
- Ius F, Fleissner F, Pichlmaier M, et al. Total aortic arch replacement with the frozen elephant trunk technique: 10-year follow-up single-centre experience. Eur J Cardiothorac Surg 2013;44:949-57. [Crossref] [PubMed]