Multi-institutional surgical outcomes of robotic single-port surgery: a Korean experience
Introduction
Since the first flexible robotic single-port system (SPS) was used in genitourinary surgery as a clinical study in France in 2014 (1), SPS has widely spread in the fields of general surgery, gynecology, genito-urology, and head and neck surgery (2-6). SPS includes three flexible instruments with the stereoscopic binocular wristed camera, all contained within a 2.8-cm-diameter cannula. However, due to its innate limitations, SPS has not widely spread in the fields of general thoracic surgery; due to the thickness of the cannula, the approaches to the lesions in the thoracic cavity, which is surrounded by rib cages, are limited, and SPS requires a 10-cm distance between the tip of the cannula and the target anatomy to triangulate the instruments and enable complete articulation of both the elbow and wrist instrument joints (7,8). To overcome these limitations, the applications of SPS in general thoracic surgery, particularly for mediastinal mass excision, were reported in the previous literature (9). In addition to the aforementioned technical limitations, as of 2022, SPS is only approved in South Korea and cannot be applied in other countries, and reports outside South Korea have not been published. In Korea, several institutions have performed SPS surgery, and sharing their experiences may be helpful for other surgeons who are preparing for SPS surgery. Therefore, this retrospective study aimed to investigate the multi-institutional surgical outcomes of SPS in South Korea.
Methods
This retrospective study included surgical data from three institutions and three thoracic surgeons who have independently performed robotic SPS surgery at their respective institutions since August 2020. Data from each institution were merged and analyzed. This retrospective study was approved by the Institutional Review Board and included 39 patients who underwent SPS surgery. Preoperative work-up included chest computed tomography, evaluations for myasthenia gravis, and pulmonary function tests. The demographic, intraoperative, and postoperative data were collected.
This was multi-institutional retrospective data from three different surgeons, so the indications of single-port (SP) surgery could be different according to the surgeons. However, as an initial experience with robotic SP thoracic surgery for three surgeons, simple mediastinal mass excision was the main indication for surgery without invading the great vessels or heart, based on radiological findings, and patients who previously underwent cardiovascular or thoracic surgery were excluded. The approaches and patients’ positions for SPS surgery were chosen according to each surgeon’s preference. The details of port placement were described in a previous paper (9). Postoperatively, the pain was assessed using a numeric pain intensity scale; the score was recorded by nurses every 8 hours until discharge (10), and the highest score during the admission periods was analyzed. The total operation time included the duration between the first skin incision for port placement and skin closure with the placement of a chest tube or drain tube. Complications were defined according to the Clavien-Dindo classification (11). Continuous variables were expressed as means ± standard deviations, and categorical variables were expressed as numbers (percentages). Statistical analyses were performed using R v2.15.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
The basic characteristics of the 39 patients who underwent robotic SPS surgery are summarized in Table 1. The patients included 16 (41.0%) males, and the mean age was 54.2±12.4 (range, 28–83) years. Thymoma (n=18) and benign cystic lesions (n=10) were the most common pathological diagnoses. The mean size of the masses was 3.8±1.8 (range, 1.2–9.7) cm.
Table 1
| Characteristics | Mean ± SD [range]/number (percentage) |
|---|---|
| Age (years) | 54.2±12.4 [28–83] |
| Males | 16 (41.0) |
| Diagnosis | |
| Thymoma | 18 (46.2) |
| Thymic carcinoma | 1 (2.6) |
| Benign cystic lesions | 10 (25.6) |
| Schwannoma | 5 (12.8) |
| Others | 5 (12.8) |
| Size (cm) | 3.8±1.8 [1.2–9.7] |
| Position | |
| Supine | 29 (74.4) |
| Lateral decubitus | 9 (23.1) |
| Semi-lateral decubitus | 1 (2.6) |
| Port for SP system | |
| SP access port | 9 (23.1) |
| Third-party port | 30 (76.9) |
| Approaches | |
| Subxiphoid | 26 (66.7) |
| Subcostal | 10 (25.6) |
| Intercostal | 3 (7.7) |
SD, standard deviation; SP, single-port.
The approach used for the SPS cannula included subxiphoid, subcostal, and intercostal in 26 (66.7%), 10 (25.6%), and 3 (7.7%) patients, respectively. Subxiphoid approaches were performed in supine positions, and intercostal or subcostal approaches were performed in semi-lateral or lateral decubitus positions. SP access port was used in 9 (23.1%) patients, whereas third-party ports were used for 30 (77.0%) patients.
The operation outcomes were summarized in Table 2. The mean operation time and peak pain score were 121.4±45.4 (range, 58–250) min and 3.1±1.1 (range, 1–6), respectively. The mean duration of in situ chest tube and hospital stay was 1.28±0.56 and 2.92±1.24 days, respectively. All surgeries were successfully completed without conversion to conventional multiport robotic surgery or thoracoscopic surgery. No operative morbidities and mortalities were noted.
Table 2
| Variables | Mean ± SD [range] |
|---|---|
| Operation time (minutes) | 121.4±45.4 [58–250] |
| Duration of in situ chest tube (days) | 1.3±0.6 [1–3] |
| Hospital stay duration (days) | 2.9±1.2 [1–7] |
| Peak pain score during the admission | 3.1±1.1 [1–6] |
SD, standard deviation.
Discussion
This retrospective study investigated the surgical outcomes of SPS in three Korean institutions. Despite the indications being highly selected and applications of SPS being confined to simple cases, SPS showed acceptable surgical outcomes. All surgeries were completed without conversion to open thoracotomy or multiport robotic surgery, and no operative mortalities and morbidities were noted.
Although SPS has improved compared with the robotic single-site system, such as flexible instruments that allow for complex movements and meticulous dissection, reduced collision and interference of instruments due to parallel entrance of the SPS instruments through a single port, and freedom to use additional instruments (three instruments simultaneously), the current indications and applications of SPS are limited to simple mass excision (either anterior or posterior mediastinal tumors), which does not require complex reconstruction or vascular approaches. Although there is no consensus on the indications and contraindications of SPS, in the case of thymic mass, clinically T3 thymoma with suspicious invasion to the veins and lungs is not frequently regarded as an indication for the SPS system due to technical and oncologic reasons. Concomitant resection and reconstruction of the pericardium are technically demanding but feasible (supplementary video). Regarding the size of the mass, large masses could be removed using the SPS system. In this series, the biggest lesion that was removed using the SPS system was a 9.7-cm sized cystic lesion.
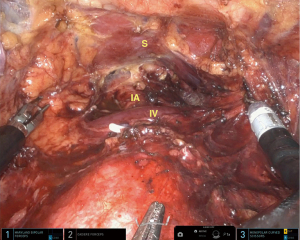
Appropriate selection of approaches is essential for a successful SPS surgery due to the thick cannula (a large outer diameter of 2.8 cm) of the SPS system. In this study, surgeries were mainly performed using subxiphoid approaches in the supine position, and intercostal or subcostal approaches were performed based on the target lesions. The supine position using subxiphoid approaches is appropriate for lesions located in the anterior mediastinum, whereas the semi-lateral or lateral decubitus position using intercostal or subcostal approaches is appropriate for lesions located in the posterior mediastinum. Furthermore, esophageal procedures, including esophagectomy, can be performed in the semi-prone position (12). Particularly, access to the upper poles of the thymus could be possible, suggesting that subxiphoid approaches using SPS could be applied for complete thymectomy, whereas approaches for the bilateral lower poles were limited (Figure 1). In our previous reports, one of the limitations of using SPS is maintaining carbon dioxide (CO2) insufflation preoperatively (9). We mainly used a third-party port designed for SP thoracoscopic or laparoscopic surgery instead of the SP access port for the SPS because the SP access port was introduced and approved in 2021. The SP access port enables the floating technique and CO2 insufflation more effectively than third-party ports preoperatively.
Among the three institutions included in this study, one institution performs SPS surgery actively; however, the other institutions are not actively performing. The major problem in expanding the applications of the SPS system is that the candidate surgeries could be performed using multiport or SP thoracoscopic surgery even within a shorter time and lower cost. Under the National Health Insurance System in Korea, all robotic surgeries are not reimbursed by the government, and patients must pay the operation cost by themselves, or through a private insurance system. Regarding economics, SPS could not gain popularity among thoracic surgeons if it cannot show definite medical benefits over other thoracoscopic surgeries. Other obstacles are technical limitations, as previously mentioned, including the absence of staplers and energy devices.
This study had some limitations. First, the data analyzed did not cover all surgical cases in Korea; several institutions performed a few cases of SPS, and these data were not included in the analysis. However, the number of those surgeries may be small, and the data of this study may include almost all cases of SPS in Korea. Second, no comparisons with thoracoscopic SP surgery or robotic single-site surgery were noted. In the future, clinical trials must be performed to evaluate the benefits of SPS over other platforms. Third, the patients in Korea are usually thinner than Western patients, and the experiences of SP surgery in high body mass index (BMI) patients were not included in this analysis. We think that operation itself with SP system might be possible even though making the subxiphoid incision might be challenging in patients with high BMI.
In conclusion, the Korean multi-institutional data showed that the operative outcomes of SPS were acceptable. To apply this system to more complex thoracic surgeries and gain popularity among other thoracic surgeons, advances in instrumentation and reductions of costs, as well as more clinical experience, are required.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kaouk JH, Haber GP, Autorino R, et al. A novel robotic system for single-port urologic surgery: first clinical investigation. Eur Urol 2014;66:1033-43. [Crossref] [PubMed]
- Shin HJ, Yoo HK, Lee JH, et al. Robotic single-port surgery using the da Vinci SP® surgical system for benign gynecologic disease: A preliminary report. Taiwan J Obstet Gynecol 2020;59:243-7. [Crossref] [PubMed]
- Cianci S, Rosati A, Rumolo V, et al. Robotic Single-Port Platform in General, Urologic, and Gynecologic Surgeries: A Systematic Review of the Literature and Meta-analysis. World J Surg 2019;43:2401-19. [Crossref] [PubMed]
- Covas Moschovas M, Bhat S, Rogers T, et al. Applications of the da Vinci single port (SP) robotic platform in urology: a systematic literature review. Minerva Urol Nephrol 2021;73:6-16. [Crossref] [PubMed]
- Salem JF, Agarwal S, Schoonyoung H, et al. Initial clinical experience with Single-Port robotic (SP r) left colectomy using the SP surgical system: description of the technique. Surg Endosc 2021;35:4022-7. [Crossref] [PubMed]
- Kim K, Kang SW, Kim JK, et al. Robotic Transaxillary Hemithyroidectomy Using the da Vinci SP Robotic System: Initial Experience With 10 Consecutive Cases. Surg Innov 2020;27:256-64. [Crossref] [PubMed]
- Park SY, Stein H, Heo SY. Preclinical, cadaveric study of the application of da Vinci single port system in thoracic surgery. J Thorac Dis 2019;11:5586-91. [Crossref] [PubMed]
- Gonzalez-Rivas D, Ismail M. Subxiphoid or subcostal uniportal robotic-assisted surgery: early experimental experience. J Thorac Dis 2019;11:231-9. [Crossref] [PubMed]
- Park SY, Lee JH, Stein H, et al. Initial experience with and surgical outcomes of da Vinci single-port system in general thoracic surgery. J Thorac Dis 2022;14:1933-40. [Crossref] [PubMed]
- Rodriguez CS. Pain measurement in the elderly: a review. Pain Manag Nurs 2001;2:38-46. [Crossref] [PubMed]
- Dindo D. The Clavien-Dindo classification of surgical complications. In: Cuesta MA, Bonjer HJ. editors. Treatment of postoperative complications after digestive surgery. London: Springer; 2014:13-7.
- Park SY. First Case of Esophagectomy Using a Robotic Single-Port System for Laryngo-Esophagectomy. J Chest Surg 2022;55:168-70. [Crossref] [PubMed]






