Outcomes of aortic valve repair with the reimplantation technique and maintenance of commissural orientation
Introduction
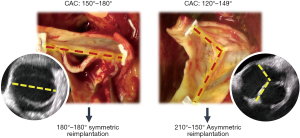
While initially developed for patients with an anatomically normal trileaflet aortic valve (TAV), valve-sparing root reimplantation (VSRR) has been increasingly utilized in those with a bicuspid aortic valve (BAV) with excellent midterm durability (1-9). Whereas aortic insufficiency (AI) in patients with a TAV is typically due to aortic root dilation alone, those with a BAV often have primary cusp pathology in addition to root aneurysms (1,5). BAV cusp morphology is highly variable, including the location and degree of cusp fusion, presence and location of a raphe, and the orientation of the two functional commissures (9). Commissural orientation is typically described as an angle with respect to the non-fused reference cusp and ranges from symmetric (160°–180°) to very asymmetric (<140°) (9,10). A more asymmetric commissural orientation has been associated with worse hemodynamics and inferior outcomes in patients undergoing BAV repair (10-12). For this reason, when performing VSRR in patients with an asymmetric BAV, some groups intentionally alter the native commissural angle and perform symmetric reimplantation with commissures at 180°–180° (8,9,13). This method decreases the tension on the conjoined cusp, which allows for primary closure of a cleft or after raphe resection (9,13). Our approach to VSRR in patients with BAV emphasizes the motion of the non-fused reference cusp, not the conjoined cusp. Conforming an asymmetric BAV to a 180°–180° symmetric reimplantation may stretch the reference cusp, decreasing its motion. Therefore, our practice is to preserve the asymmetry of BAVs with commissural orientation <140°–150° and reimplant the commissures in an asymmetric 210°–150° orientation as opposed to symmetric 180°–180° (Figure 1) (14). The objectives of this report were to: (I) demonstrate our step-by-step method of maintaining BAV commissural orientation during VSRR in a video, and (II) present the outcomes of our experience with this technique.
Methods
Patient population
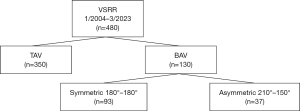
From January 1, 2004 through March 1, 2023, 483 consecutive reimplantation procedures were performed at our institution. Data were captured prospectively, maintained in a secure database, and retrospectively reviewed for this analysis. From the starting population, we excluded 2 patients with prior Ross procedures who underwent reimplantation of the pulmonary autograft, and one in which a BAV was tricuspidized, as this case was unique and not our typical practice. Of the remaining 480 patients, 350 had a TAV and 130 had a BAV. In the BAV group, 93 were reimplanted symmetrically and 37 were reimplanted asymmetrically (Figure 2). The 37 patients with asymmetric VSRR were included in this series. The median clinical follow-up was 7.7 years (IQR: 2.4–10.6), while the median echocardiographic follow-up was 5.8 years (IQR: 1.2–9.0).
Operative technique
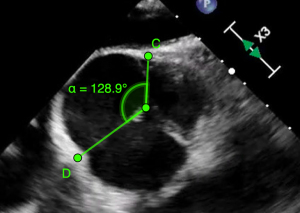
Our approach to performing VSRR in patients with asymmetric BAVs is illustrated in detail in the accompanying video. All cases are performed with transesophageal echocardiography (TEE). Pre-procedurally, TEE is used to measure annular and root diameters, identify mechanisms of AI, and describe the morphology of the BAV. To date, we have measured the commissural angle with TEE using the method described by Aicher and colleagues and de Kerchove and associates (9,10). Briefly, on short axis view in mid-diastole, lines are drawn from the two functional BAV commissures to the center of valve coaptation. The angle with respect to the reference cusp is then measured (Figure 3). After initiation of cardiopulmonary bypass, application of the aortic cross clamp, and dissection of the aortic root, the valve is examined in its native state to determine its suitability for reimplantation. This comprehensive valve analysis includes annular sizing, measurement of geometric and effective heights as described by Schäfers and colleagues (15,16), and an assessment of cusp mobility and tissue quality. We consider significant leaflet body calcification, restricted mobility of the non-fused reference cusp, large fenestrations, substantial sinus thinning, or insufficient leaflet surface area as measured by geometric height (BAV reference cusp <19–20 mm), reasons to abort VSRR and implant a prosthetic valve instead.
Following the placement of the subannular (primary) suture line, the leaflets are assessed for repair. Central cusp plication or resection with primary closure using interrupted 5–0 polypropylene or PTFE (Gore-Tex, W. L. Gore & Associates, Inc, Flagstaff, AZ, USA) is most commonly used to equalize the leaflet free margins, optimize effective height, and correct prolapse. Commissuroplasty is occasionally used to improve commissural diastasis. Small fenestrations are typically ignored but occasionally are closed primarily, with a pericardial patch, or with free-margin shortening using running PTFE or polypropylene. Raphe release, decalcification/debulking, or resection with primary or pericardial patch closure is often performed to improve the mobility of the conjoined cusp.
Early on in our experience, valves were reimplanted inside a straight Dacron graft that was tailored to create neo-sinuses (n=2). The Gelweave Valsalva graft (Vascutek Ltd., Renfrewshire, Scotland) has been used subsequently in all others (n=35). Selecting a Valsalva graft size is more complicated for VSRR in patients with a BAV compared to those with a trileaflet valve. It is often not possible to size the annulus directly in a BAV case, as the leaflet orifice area may be smaller than the annular size and thus the sizer cannot pass. Our approach to sizing for VSRR in those with a BAV considers several key concepts. First, we measure the distance from an imaginary line drawn from the nadirs of the left and noncoronary cusps to the top of the left-non commissure (17). This left-non commissural height (in mm) can be used to select the equivalent sized Valsalva graft (in mm). After this measurement is made, we assess the reference cusp geometric height to determine whether the graft size should be adjusted. If the reference leaflet geometric height is large (>25–26 mm), then we will often select a Valsalva graft one size larger than what was chosen based on the left-non commissural height. By contrast, if the geometric height is on the smaller side, we may select one size smaller. We believe that the key to long-term durability is leaving the reference cusp pristine and preserving its motion. Therefore, we try to size the Valsalva graft so that the reference cusp does not prolapse and require plication. If plication is needed, then the size of Valsalva graft may be too small (and the annular reduction too great). Lastly, we try to reduce the BAV annulus to what is physiologically “normal” for the patient’s BSA. It is important to remember that after tying the primary suture line, the annular diameter will be reduced by 5–6 mm, regardless of what Valsalva graft size was selected. While we often tie over a dilator for trileaflet VSRR cases to prevent excess annular reduction, this is done only rarely in BAV cases, specifically when the annulus is very small to begin with and we do not want to reduce the annulus significantly.
After selecting a Valsalva graft, the subannular sutures are passed through the graft, which is parachuted into the root and tied down. Next, the commissures are reimplanted. Conversion of an asymmetric BAV to a symmetric 180°–180° VSRR may stretch the reference cusp, reducing its mobility. For this reason, we prefer to reimplant asymmetric BAVs with commissural angle <140°–150° in an asymmetric fashion with commissures oriented at 210°–150°. By contrast, for a more symmetric BAV with commissural angle >140°–150°, the commissures are reimplanted symmetrically at 180°–180°. After completion of the secondary suture line securing the valve complex within the Dacron graft and the coronary button anastomoses, secondary valve analysis is performed, as reimplantation may have altered the valve geometry. Additional leaflet repair is performed at this time if needed. After cross clamp removal, TEE is used to assess for any residual AI, coaptation length (goal >6 mm), and level of cusp coaptation relative to the annular plane. If more than mild AI was seen on TEE, the cross-clamp was reapplied for additional valve repair or conversion to prosthetic replacement.
Study design and analysis
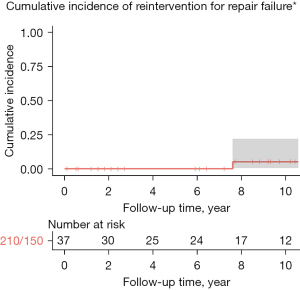
For this series, only the 37 patients with asymmetric commissural orientation who underwent asymmetric VSRR were analyzed. The primary outcome was > moderate AI. Secondary outcomes included aortic stenosis (AS), aortic valve reintervention, and survival. Of note, aortic valve reoperation for infection was excluded from the reintervention outcome analysis, as infection was not considered evidence of repair failure. Additional perioperative outcomes were defined by Society of Thoracic Surgeons criteria (18). Kaplan-Meier estimate was determined for long-term survival. Cumulative incidence functions were calculated for > moderate AI and severe AS. Lastly, a cumulative incidence function was created for reintervention with all-cause mortality as competing risk. Statistical analyses were performed with R software, version 4.1.1 (R Foundation).
Results
Baseline characteristics
The 37 included patients were mostly male [94.6% (35/37)] with mean age of 46.3 years and had low rates of comorbidities (Table 1). All procedures were elective. None were performed in the setting of aortic dissection. At least moderate AI was present in 40.5% (15/37) prior to surgery.
Table 1
| Characteristic | 210°–150° BAV VSRR (n=37) |
|---|---|
| Age (years) | 46.3 (12.4) |
| Male | 35 (94.6) |
| Hypertension | 18 (48.6) |
| Diabetes | 1 (2.7) |
| Chronic lung disease | 2 (5.4) |
| Coronary artery disease | 2 (5.4) |
| Marfan syndrome | 0 |
| Loeys-Dietz syndrome | 0 |
| Type A aortic dissection | 0 |
| Prior cardiac surgery | 0 |
| Elective procedure status | 32 (97.0) |
| LVEF (%) | 54.9 (7.86) |
| > Moderate aortic insufficiency | 15 (40.5) |
Categorical variables are presented as number (percentage). Continuous variables are presented as mean (standard deviation). BAV, bicuspid aortic valve; VSRR, valve-sparing root reimplantation; LVEF, left ventricular ejection fraction.
Operative details and early outcomes
Procedural characteristics are presented in Table 2. The mean commissural angle measured on intraoperative TEE of the 37 patients reimplanted asymmetrically was 128.2°. By contrast, the mean angle was 156.7° for the symmetric 180°–180° cohort not included in this study. All 37 asymmetric BAVs in this series were classified as Sievers Type 1. Leaflet repair was required in 81.1% (30/37), which most commonly included central plication of the conjoined cusp [96.7% (29/30)] and raphe release [73.3% (22/30)]. The majority of patients underwent concomitant procedures at the time of VSRR, which most often was hemi-arch replacement [89.3% (25/37)]. Short-term outcomes are presented in Table 3. There was no 30-day mortality or stroke. Permanent pacemaker implantation was required in 1 patient (2.7%) prior to discharge. There were no 30-day aortic valve reinterventions.
Table 2
| Characteristic | 210°–150° BAV VSRR (n=37) |
|---|---|
| Bypass time (min) | 270.9 (51.8) |
| Cross clamp time (min) | 226.7 (45.0) |
| Circulatory arrest | 25 (67.6) |
| Circ arrest time (min) | 18.3 (4.7) |
| Concomitant procedure | 28 (75.7) |
| Coronary artery bypass | 1 (3.6) |
| Hemi-arch replacement | 25 (89.3) |
| Sievers type 1 | 33 (100.0) |
| Commissural angle* | 128.2 (10.5) |
| Leaflet repair | 30 (81.8) |
| Plication | 29 (96.7) |
| Resection | 1 (3.3) |
| Decalcification/debulking | 9 (30.0) |
| Fenestration closure | 1 (3.3) |
| Raphe release | 23 (73.3) |
| Cleft closure | 6 (20.0) |
| Commissuroplasty | 1 (3.3) |
| Free margin shortening | 0 |
Categorical variables are presented as number (percentage). Continuous variables are presented as mean (standard deviation). *, commissural orientation measured on intraoperative transesophageal echocardiography in mid-diastole from the two functional commissures to the center of cusp coaptation. BAV, bicuspid aortic valve; VSRR, valve-sparing root reimplantation.
Table 3
| Characteristic | 210°–150° BAV VSRR (n=37) |
|---|---|
| Operative mortality | 0 |
| 30-day stroke | 0 |
| 30-day permanent pacemaker | 1 (2.7) |
| 30-day readmission | 4 (10.8) |
| 30-day reintervention | 0 |
Categorical variables are presented as number (percentage). Continuous variables are presented as mean (standard deviation). BAV, bicuspid aortic valve; VSRR, valve-sparing root reimplantation.
Long-term estimates
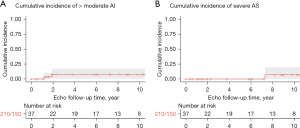
At 10 years, the cumulative incidence of > moderate AI and severe AS was 7.6% (0–17.2%) and 7.1% (0–19.7%), respectively (Figure 4). The cumulative incidence of aortic valve reintervention with all-cause mortality as competing risk was 5.3% at 10 years (Figure 5). By Kaplan-Meier estimate, 10-year survival was 100% (Figure 6).
Discussion
BAV commissural orientation exists in a spectrum from symmetric (180°) to very asymmetric (<140°) (9). Traditionally, commissural orientation has been described as an angle with respect to the non-fused reference cusp by lines drawn from the two functional commissures to the center of cusp coaptation during mid-diastole (9,10,19). To date, we have employed this method in our practice using intraoperative TEE for patients undergoing isolated BAV repair and VSRR. More recently, Froede and colleagues have developed a novel method to measure this angle by defining the geometric center of the aortic root (19). However, we have not yet applied this method in our clinical practice.
Prior study has suggested that asymmetric BAVs have worse hemodynamics and inferior outcomes after repair (10-12). In fluid-structure interaction models, Marom and colleagues found that asymmetric BAV geometry caused asymmetric flow vortices and greater shear stress on the cusps compared to symmetric BAV and TAV models (11). Similarly, Stephens and associates reported that BAV cusp morphology significantly affects flow patterns and wall shear stress after VSRR (12). Valves classified as Sievers Type 1 with left-right fusion had increased wall shear stress and flow eccentricity whereas Sievers Type 0 had comparable hemodynamics to TAV controls (12). In 316 patients undergoing BAV repair, Aicher and colleagues found that commissural orientation <160° was significantly associated with reoperation (10).
For this reason, many groups intentionally alter the commissural angle for a more symmetric repair (9,13,20). In isolated BAV repair without root replacement for valves with commissural angle 130°–150°, Schneider and colleagues described plication of the fused sinuses to an angle between 160°–180° (20). The 35 patients who underwent this procedure had a mean increase in commissural angle of 24°±5° and had significantly improved freedom from recurrent AI and reoperation compared to a historic control group that did not undergo sinus plication (20). In patients with significant aortic root dilation undergoing remodeling procedures, Schäfers and colleagues described tailoring the graft with two nearly symmetric tongues for a 170° to 180° repair orientation (21). Similarly, for VSRR procedures, de Kerchove and associates described the intentional placement of the subannular sutures and commissures to create a symmetric 180°–180° repair (8,9). This technique decreases the tension on the conjoined cusp, which facilitates primary closure of a cleft or after raphe resection without the use of a pericardial patch (9,13).
Our approach to VSRR in patients with BAV places supreme importance on the non-fused reference cusp, not the conjoined cusp. Conforming an asymmetric BAV with native commissural angle <140°–150° to a 180°–180° symmetric reimplantation may stretch or “banjo string” the reference cusp, decreasing its motion. Therefore, our institutional practice has been to maintain the asymmetry of BAVs with commissural angle <140°–150° during VSRR by reimplanting these valves in an asymmetric 210°–150° orientation. Ensuring pristine reference cusp motion is the key attribute toward long-term durability. Even more important than commissural orientation is the geometric height of the reference cusp, which is measured intraoperatively. de Kerchove and colleagues reported a correlation between increased asymmetry and smaller reference cusp geometric height (9). Preserving asymmetry is therefore particularly important for valves with a smaller reference cusp geometric height measuring close to 19–20 mm, which is the minimum required for repair. Others have described the conversion of BAVs with commissural orientation <130° to trileaflet valves during repair (9,20). However, the tricuspidization of very asymmetric BAVs is not our practice. We instead prefer to reimplant these BAVs in asymmetric 210°–150° orientation.
In this series, we report the procedural details and outcomes of 37 patients with asymmetric BAVs with mean commissural angle of 128.2° who underwent VSRR with commissural reimplantation in an asymmetric 210°–150° orientation. The majority of patients in this series required leaflet repair (81.1%), which mostly included central plication of the conjoined cusp (96.7%) and raphe release (73.3%). Those requiring cleft closure (6/30), or raphe resection (1/30), were closed primarily with interrupted sutures as opposed to a pericardial patch. The 37 patients in this series had excellent short-term outcomes without mortality or stroke. At 10 years, the cumulative incidences of > moderate AI, severe AS, and aortic valve reintervention were 7.6%, 7.1%, and 5.3%, respectively.
During the entire duration of the study period, 3 patients underwent aortic valve reintervention. In one, the aortic root was replaced at 3 years for a non-tuberculosis mycobacterium graft infection. At the time of reoperation, the previously repaired BAV was noted to be without significant AS or AI. Two patients required reintervention for severe AS at 8 and 14 years postoperatively who were treated with surgical aortic valve replacement and transcatheter aortic valve implantation, respectively. The development of significant AS remains a conceptual limitation of BAV repair in very asymmetric commissural orientations, regardless of repair strategy, especially for those with smaller reference cusp geometric height. While the first decade is quite promising, the incidence and clinical significance of AS following VSRR in patients with asymmetric BAVs requires further study as more patients reach the second decade of follow-up.
Limitations
As a single center series, our sample size is small, and the patients were highly selected. Moreover, these cases were performed by a small number of surgeons at a tertiary referral center, which limits the generalizability of our findings. This retrospective analysis is also limited by the availability of data recorded in the medical record. Several patients were lost to follow-up or were missing TTE data, especially those who live non-locally.
Conclusions
This series demonstrates excellent 10-year clinical outcomes of maintaining commissural orientation in asymmetric BAV reimplantation procedures. These findings suggest that our algorithm for approaching BAV patients undergoing VSRR is effective. However, further study with additional patients, longer follow-up, and direct comparison with the symmetric reimplantation of similar BAV phenotypes is required.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bavaria JE, Desai N, Szeto WY, et al. Valve-sparing root reimplantation and leaflet repair in a bicuspid aortic valve: comparison with the 3-cusp David procedure. J Thorac Cardiovasc Surg 2015;149:S22-8. [Crossref] [PubMed]
- Levine D, Patel P, Zhao Y, et al. Bicuspid aortic valve durability with valve-sparing aortic root replacement: comparison to tricuspid valve. Eur J Cardiothorac Surg 2023;63:ezad030. [Crossref] [PubMed]
- Mokashi SA, Rosinski BF, Desai MY, et al. Aortic root replacement with bicuspid valve reimplantation: Are outcomes and valve durability comparable to those of tricuspid valve reimplantation? J Thorac Cardiovasc Surg 2022;163:51-63.e5. [Crossref] [PubMed]
- David TE, David CM, Feindel CM, et al. Reimplantation of the aortic valve at 20 years. J Thorac Cardiovasc Surg 2017;153:232-8. [Crossref] [PubMed]
- Ouzounian M, Feindel CM, Manlhiot C, et al. Valve-sparing root replacement in patients with bicuspid versus tricuspid aortic valves. J Thorac Cardiovasc Surg 2019;158:1-9. [Crossref] [PubMed]
- Kayatta MO, Leshnower BG, McPherson L, et al. Valve Sparing Root Replacement Provides Similar Midterm Outcomes in Bicuspid and Trileaflet Valves. Ann Thorac Surg 2019;107:54-60. [Crossref] [PubMed]
- Beckmann E, Martens A, Krüger H, et al. Aortic valve-sparing root replacement in patients with bicuspid aortic valve: long-term outcome with the David I procedure over 20 years. Eur J Cardiothorac Surg 2020;58:86-93. [Crossref] [PubMed]
- de Meester C, Vanovershelde JL, Jahanyar J, et al. Long-term durability of bicuspid aortic valve repair: a comparison of 2 annuloplasty techniques. Eur J Cardiothorac Surg 2021;60:286-94. [Crossref] [PubMed]
- de Kerchove L, Mastrobuoni S, Froede L, et al. Variability of repairable bicuspid aortic valve phenotypes: towards an anatomical and repair-oriented classification. Eur J Cardiothorac Surg 2019;ezz033. [Crossref] [PubMed]
- Aicher D, Kunihara T, Abou Issa O, et al. Valve configuration determines long-term results after repair of the bicuspid aortic valve. Circulation 2011;123:178-85. [Crossref] [PubMed]
- Marom G, Kim HS, Rosenfeld M, et al. Fully coupled fluid-structure interaction model of congenital bicuspid aortic valves: effect of asymmetry on hemodynamics. Med Biol Eng Comput 2013;51:839-48. [Crossref] [PubMed]
- Stephens EH, Hope TA, Kari FA, et al. Greater asymmetric wall shear stress in Sievers' type 1/LR compared with 0/LAT bicuspid aortic valves after valve-sparing aortic root replacement. J Thorac Cardiovasc Surg 2015;150:59-68. [Crossref] [PubMed]
- de Kerchove L, Boodhwani M, Glineur D, et al. Valve sparing-root replacement with the reimplantation technique to increase the durability of bicuspid aortic valve repair. J Thorac Cardiovasc Surg 2011;142:1430-8. [Crossref] [PubMed]
- Siki MA, Habertheuer A, Bavaria JE, et al. Two different geometric orientations for aortic neoroot creation in bicuspid aortic valve repair with root reimplantation. J Thorac Cardiovasc Surg 2020;160:47-57. [Crossref] [PubMed]
- Schäfers HJ, Schmied W, Marom G, et al. Cusp height in aortic valves. J Thorac Cardiovasc Surg 2013;146:269-74. [Crossref] [PubMed]
- Schäfers HJ, Bierbach B, Aicher D. A new approach to the assessment of aortic cusp geometry. J Thorac Cardiovasc Surg 2006;132:436-8. [Crossref] [PubMed]
- Boodhwani M, El Khoury G, de Kerchove L. Graft sizing for aortic valve sparing surgery. Ann Cardiothorac Surg 2013;2:140-3. [Crossref] [PubMed]
- Society of Thoracic Surgeons. STS Adult Cardiac Surgery Database Data Specifications Version 2.9. Published online February 13, 2017. Accessed January 8, 2023. Available online: https://www.sts.org/sites/default/files/documents/ACSD_DataSpecificationsV2_9.pdf
- Froede L, Schäfers S, Wagenpfeil G, et al. Simplified determination of commissural orientation in bicuspid aortic valves. Eur J Cardiothorac Surg 2020;58:1153-60. [Crossref] [PubMed]
- Schneider U, Schmied W, Aicher D, et al. Sinus Plication to Improve Valve Configuration in Bicuspid Aortic Valve Repair-Early Results. Ann Thorac Surg 2017;103:580-5. [Crossref] [PubMed]
- Schäfers HJ, Kunihara T, Fries P, et al. Valve-preserving root replacement in bicuspid aortic valves. J Thorac Cardiovasc Surg 2010;140:S36-40; discussion S45-51. [Crossref] [PubMed]







