A systematic review and meta-analysis of hybrid aortic arch replacement
Introduction
The management of patients with aortic disease that involves the ascending aorta, the aortic arch, and the descending aorta poses a technical challenge and is an area of ongoing development and innovation. Total arch replacement, although traditionally challenging and risky, has been the mainstay of therapy for aortic arch pathologies. However, this operation requires cardiopulmonary bypass and a period of profound hypothermia and circulatory arrest, which carries a substantial rate of mortality and morbidity (1,2). Protection from brain, spinal cord, cardiac, and visceral ischemia, as well as the avoidance of respiratory compromise due to prolonged circulatory arrest, are significant concerns. Despite higher standards of perioperative care, refinements in operative techniques, and the use of several protective adjuncts, the morbidity associated with total arch replacement is significant, and includes air embolism, stroke, myocardial infarct, and excessive bleeding (1,2). In addition, in cases of aortic arch involvement, entirely endovascular methods entail advanced technical skills (3), whereas the rate of neurological complications remains considerable.
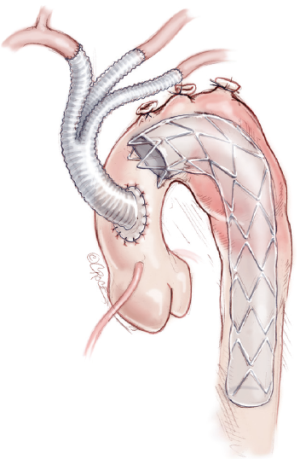
Several studies have described the use of a combined endovascular and open surgical approach to the treatment of arch pathologies, resulting in a hybrid technique, which has been considered as a less invasive method. Consequently, it represents an appealing option for high-risk patients who are unsuitable for open repairs. These “hybrid techniques” involve arch debranching, thereby creating a proximal landing zone of adequate length, followed by stenting over the aortic arch (4,5) (Figure 1). For this purpose, highly specialized arch-debranching grafts have been developed. The endovascular component can be performed either simultaneously or in a staged mode, and in an antegrade or retrograde fashion. Among the evolving hybrid procedures is the so-called “frozen” or stented elephant trunk technique (6,7). Adapted from the classical elephant trunk technique that was first described by Borst et al. (8), this approach facilitates the repair of a concomitant aortic arch and proximal descending aortic aneurysms in a single stage under circulatory arrest. This technique is increasingly being used to treat extensive thoracic aortic disease and has shown promising results (6,7).
We undertook a systematic review to identify all published reports on hybrid aortic arch replacement. Eligible studies were combined into an extensive meta-analysis to assess the safety and efficacy of this technique.
Methods
Search strategy
An extensive electronic literature search was undertaken to identify all articles that were published up to December 2012 and described hybrid aortic arch repair (HAAR). The search was performed by using “aortic arch”, “arch debranching”, “frozen elephant trunk”, “stented elephant trunk”, “endovascular”, and “hybrid” as exploded MeSH terms. Publications were retrieved via electronic search engines (Medline, Embase, Scopus, Google Scholar, Ovid, and the Cochrane Library). In addition, the reference lists of all retrieved articles were examined for further relevant series.
Definitions
Aortic arch zones are categorized according to classifications established by Mitchell and Ishimaru (9): zone 0 involves the ascending aorta proximal to the innominate artery. Zone 1 involves the aortic arch between the innominate and left common carotid artery. Zone 2 involves the aortic arch between the left common carotid artery and the left subclavian artery. Zone 3 involves the proximal descending thoracic aorta distal to the left subclavian artery. Zone 4 involves the mid-descending thoracic aorta.
Hybrid approaches are classified into three types according to the extent of aortic arch lesion and the presence of the proximal and distal landing zone:
- Type I: the debranching procedure consists of brachiocephalic bypass and endovascular repair of the aortic arch. This approach is reserved for patients with isolated aortic arch aneurysms that exhibit an adequate proximal landing zone in the ascending aorta and a distal landing zone in the descending thoracic aorta.
- Type II: this hybrid approach is designed for patients with ascending aortic lesions with a limited extension into the distal arch. A type II repair entails an open ascending aorta reconstruction that “creates” an appropriate proximal landing zone, great vessel revascularization, and endoluminal aneurysm exclusion.
- Type III: an elephant trunk procedure with a complete endovascular repair of the thoracoabdominal aorta. This technique is reserved for patients with extensive aortic lesions that involve the ascending, transverse arch, and descending thoracic aorta, or the “mega-aorta syndrome”.
Eligibility inclusion and exclusion criteria
In the present review, eligible studies were categorized into two groups: group I, which included studies on the aortic arch debranching procedure (AD group) and group II, which included studies that report on the elephant trunk (ET group) technique (i.e., either “frozen” or stented).
An eligible study for the present meta-analysis must:
- Describe intrathoracic hybrid aortic arch repair.
- Provide baseline characteristics of the recruited patients.
- State the incidence of at least one of the basic outcome criteria.
- Report on a series of at least 10 patients to prevent bias arising from small sample populations. This cutoff was chosen as the threshold criterion on the basis that experience with this technique from a center with more than 10 treated patients increases the homogeneity of the analysis, reflects institutional experience and, therefore, merits consideration.
Exclusion criteria included the following: articles in languages other than English, case reports, and series of <10 patients. When multiple publications on the same patient sample were identified or study populations overlapped, only the latest report was included unless the reported outcomes were mutually exclusive. Furthermore, in several studies, patients with combined visceral debranching and endovascular exclusion of thoracoabdominal pathologies were analyzed as a subgroup of a wider patient sample. These studies were excluded from the present meta-analysis because data regarding this subgroup of patients were not separately provided. All studies were assessed by two reviewers (K.M. and S.M.). Available data were extracted and analyzed, and a consensus was reached if discrepancies were observed.
Statistical analyses
Standard descriptive statistics (reported as means with 95% confidence intervals) were used to summarize demographic and baseline data of the recruited patients from all eligible studies. A separate meta-analysis was conducted, in accordance with the recommendations of the Meta-analysis of Observational Studies in Epidemiology (MOOSE) group, of the two cohorts (10). The primary endpoints of the meta-analysis consisted of technical success, 30-day/in-hospital mortality, spinal cord ischemia (SCI) symptoms, and pulmonary and cardiac complications. The pooled proportion was calculated as the back-transformation of the weighted mean of the transformed proportions by using the random effects model proposed by DerSimonian-Laird (11). Heterogeneity among studies was estimated by using the chi-square test and the Cochran Q score (reported as I2 and representing the percent value of the heterogeneity). Funnel plots were constructed, and the identified extreme studies were excluded to increase the robustness of our analyses. Frequency study-specific estimates were pooled and are reported as proportions with 95% confidence intervals (CI). The possibility of publication bias was assessed for both aims by using use the Begg-Mazumdar adjusted rank correlation test (12). The meta-analysis and the publication bias assessment were conducted by using the Comprehensive Meta-analysis Package (Biostat, Englewood, NJ) statistical software.
Results
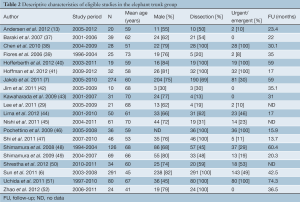
The literature search yielded 196 publications (Figure 2). After an extensive review, a total of 75 articles were considered relevant. Of these 75 articles, 29 publications were excluded in the subsequent evaluation based on the inclusion/exclusion criteria. Forty-six studies were eligible for the present meta-analysis: 26 studies, with a total of 956 patients, examined the aortic arch debranching procedure, and 20 studies, with a total of 1,316 patients, focused on a technique that involved either a “frozen” or stented elephant trunk (Tables 1,2). Demographic variables and comorbidities of the patients are detailed in Table 3.


Full table
Full table
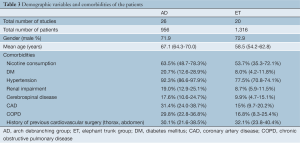
Full table
Arch debranching group
The majority of the patients (62.0%) underwent arch debranching attributable to degenerative aneurysms, with 28.6% attributable to aortic dissection, 2.2% attributable to a pseudoaneurysm or traumatic transection, and 7.2% attributable to other aortic pathologies such as penetrating ulcers, intramural hematomas, aortobronchial fistula, intracranial aneurysm, endoleak correction after thoracic aortic aneurysm, and floating thrombus in the aortic arch. Zone 0 was involved in 342/820 (41.7%) patients, Zone 1 in 237/820 (28.9%) patients, and Zone 2 in 241/820 (29.4%). Almost 74% of the patients were referred for elective treatment, with the remainder operated on in an emergent/urgent setting. A single-stage approach was implemented in 52.9% of patients, while 47.1% underwent a staged procedure with a mean intra-procedural interval of 18.5 days (95% CI: 7.6-29.4 days). Cardiac arrest was utilized in 9.2% (67/731) of the patients. Mean ICU stay was 2 days (95% CI: 1.1-3.0 days), and mean length of hospital stay was 12.1 days (95% CI: 8.2-15.9 days). Mean follow-up period was 22.1 months (95% CI: 18.2-26.1 months).
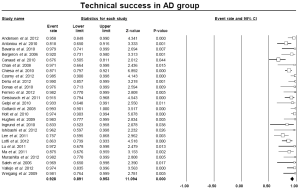
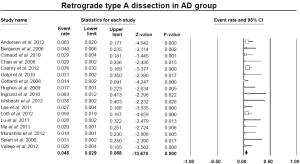
With respect to the primary technical success, which was defined as complete aortic arch debranching and successful stent-graft deployment, the pooled estimate was 92.8% (95% CI: 89.1-95.3%) (Figure 3). Of the 894 patients for whom both stages of the procedure were completed, 149 (16.6%) experienced an endoleak. In particular, 165 endoleaks were detected in follow-up CT scans: 106 type I, 51 type II, and 8 type III. Among 17 studies which provided relative data, retrograde type A dissection was observed with a pooled rate of 4.5% (95% CI: 2.9-6.8%) (Figure S1).
Mortality and morbidity in the arch debranching group
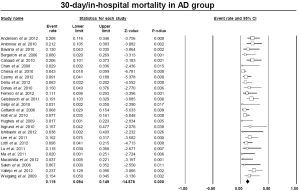
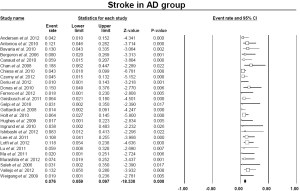
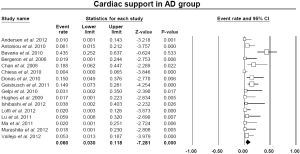
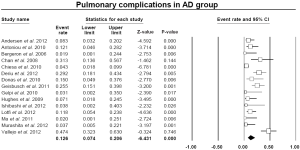
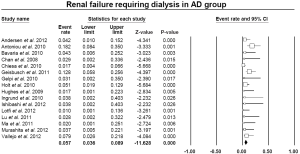
The pooled estimate for 30-day/in-hospital mortality was 11.9% (95% CI: 9.4-14.9%) (Figure 4). A cerebrovascular event of any severity was found to occur postoperatively at a pooled rate of 7.6% (95% CI: 5.9-9.7%) (Figure 5). Irreversible SCI symptoms were present at a pooled estimate of 3.6% (95% CI: 2.5-6.1%) (Figure 6). Data regarding the need for cardiac support were available in 16 out of the 26 AD studies, with a pooled cardiac complications rate of 6.0% (95% CI: 3.0-11.8%) (Figure S2). Additionally, the pooled estimate for pulmonary complications among 15 studies which provided adequate data was 12.6% (95% CI: 7.4-20.6%) (Figure S3). However, there was a substantial level of heterogeneity between studies (I2=68% and I2=75% for cardiac and pulmonary complications, respectively). Renal failure requiring dialysis was found at a pooled rate of 5.7% (95% CI: 3.6-8.9%) (Figure 7).

Elephant trunk group (ET)
The indication for ET in 72.4% of patients was chronic or acute aortic dissection that involved the ascending aorta, a degenerative atherosclerotic aneurysm in 27.3% of patients, and 0.3% was due to other aortic pathologies. The treatment was elective in 58.4% of the patients, with the remainder operated on in an emergency or urgent setting. The mean cardiopulmonary bypass (CPB) time was 193 minutes (95% CI: 171-214 minutes), mean ICU stay was 5.7 days (95% CI: 1.0-10.7 days), mean length of the hospital stay was 21 days (95% CI: 17.1-24.8 days), and the mean follow-up period was 43.7 months (95% CI: 34.2-53.2 months).
Mortality and morbidity in the elephant trunk group
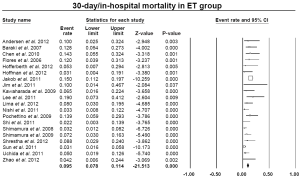
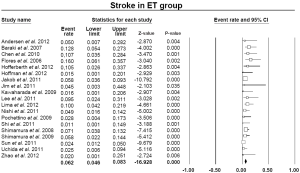
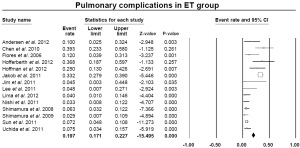
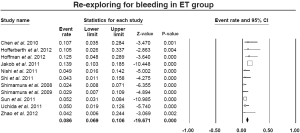
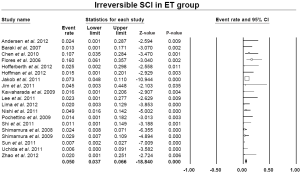
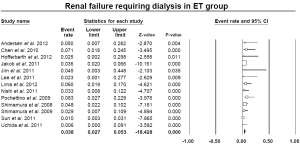
The pooled estimate for 30-day/in-hospital mortality was 9.5% (95% CI: 7.8-11.4%) (Figure 8). A cerebrovascular event of any severity was found to occur postoperatively at a pooled rate of 6.2% (95% CI: 4.6-8.3%) (Figure 9). However, irreversible SCI symptoms were present at a pooled estimate of 5.0% (95% CI: 3.7-6.6%) (Figure 10). The pooled rates for renal failure that required dialysis and pulmonary complications were 3.8% (95% CI: 2.7-5.3%) and 19.7% (95% CI: 17.1-22.1%), respectively (Figure 11, Figure S4). In 11 studies within the elephant trunk group, data regarding re-exploration for bleeding were provided. A separate meta-analysis of these studies revealed a pooled incidence of the secondary intervention due to bleeding of 8.6% (95% CI: 6.9-10.6%) (Figure S5).
Discussion
Our study aims to review the results of hybrid techniques which have been applied for the treatment of aortic arch pathologies and extensive arch lesions. Although the hybrid approach is considered appropriate for high-risk patients and has been applied within urgent and emergency settings, varied lesion patterns and patient characteristics result in a significant heterogeneity among reported studies. With the intention of pooling the published results, we have classified these methods into two separate categories according to the need for ascending aorta reconstruction: the “total arch debranching procedure”, and “elephant trunk” technique and its variation (i.e., the “stented elephant trunk” procedure). Both methods consist of two steps: the open surgical portion and the endovascular component. They can be conducted either as one- or two-stage procedures. The elimination of the need for extensive arch and thoracic aorta dissection and the reduced time of total circulatory arrest, which is not required in all cases of hybrid reconstruction, generate significant appeal for this strategy in selected patients.
The above-referenced debranching procedure was most commonly used for the treatment of degenerative arch aneurysms in Zone 0 and/or Zone 1. Several points have been studied in this meta-analysis. The 30-day mortality rate for the “debranching” procedures was 11.9%. The stroke rate was 7.6% and the spinal cord ischemia rate was 3.6%, while pulmonary complications were observed on average in 12.6% of patients. Cardiac complications, such as myocardial infarction and cardiac arrhythmias, were present in 6.0% and renal insufficiency requiring permanent hemodialysis occurred in 5.7% of patients within the studies. The spinal cord ischemia rate of 3.6% indicates a fairly low incidence that can likely be explained by two main reasons. Firstly, during debranching procedures, there is no need for total aortic cross-clamping, which eliminates the ischemia time of the spinal cord. Secondly, for arch aneurysms, the length of aortic coverage with the endo-graft is relatively short. Thus, the intercostal arteries remain intact while the left subclavian artery and consequently, the left internal mammary artery, are revascularized.
Another point that merits consideration from the present results is the low mortality rate in this sensitive group of patients. These patients are considered unfit for the traditional open repair of arch aneurysms which precludes total circulatory arrest and deep hypothermia. In our study, almost all of the patients of the AD group were hypertensive or taking anti-hypertensive agents, with one in five patients suffering from diabetes, renal impairment or cerebrovascular disease, and one in three patients having a history of coronary artery disease or previous cardiovascular surgery. The debranching procedure is believed to be less invasive as there is no need for aortic cross clamping and cardiopulmonary bypass. Furthermore, we found a pooled rate of 92.8% for the technical success of this method. Although such an outcome seems to be reasonable, we could not neglect the considerable rate of endoleaks (16.6%), the majority of which were type I, as well as the fact that postoperative retrograde type A dissection was presented in 4.5% of the patients. These findings could be attributed to the quality of the ascending aorta. Residual atherosclerosis or retrograde dissection may jeopardize this procedure.
The “frozen” or stented elephant trunk technique was adapted from the classic elephant trunk technique. According to this method the repair of concomitant aortic arch and proximal descending aortic aneurysms can be performed in a single stage under circulatory arrest, eliminating the need for a second posterolateral thoracotomy. In our review, 72.4% of the procedures were conducted in order to treat aortic dissections, leaving 27.3% for the repair of aneurismal disease and 0.3% for other pathologies (e.g., pseudoaneurysm repair of the aortic arch). A great number of urgent procedures (41.6%) were performed with the above technique, which may be responsible for the variability of the results among the different series. We observed significant heterogeneity of results between the eligible studies, especially with respect to the 30-day mortality rate and incidence of spinal cord ischemia complications. This heterogeneity can be partially explained by the differences between elective and urgent operations and because the elephant trunk technique was mostly used for the treatment of aortic dissections. Despite the severity of the pathologies, the pooled 30-day mortality rate was approximately 9.5%, which is an acceptable outcome. In addition, the stroke rate ranged around 6.2%.
With regard to the other outcomes in the ET group, the fact that surgical prosthetic material provides a safe landing zone for the stent-graft in ET procedures eliminates the risk for type Ia endoleak. However, the re-exploration rate for bleeding was estimated at approximately 8.6%, which is not a negligible rate. The main cause for postoperative bleeding is the coagulopathy disorders attributed to deep hypothermia and the heparin administration during total circulatory arrest. In addition, pulmonary complications in the present meta-analysis occurred at a pooled rate of 19.7%, leading to a prolonged stay in the ICU. In contrast, a relatively low incidence of irreversible spinal cord ischemia and permanent renal insufficiency were observed. In fact, the pooled estimate for SCI symptoms and renal impairments requiring dialysis were 5% and 3.8%, respectively. Both complications are main concerns when extensive reconstructions of large aortic segments, such as thoracoabdominal aneurysms, are required. We believe that the cooling of the patient, decreased ischemic time during the application of the trunk and central anastomosis, together with the application of various adjunctive measures such as CSF drainage, may result in a minimized risk of permanent spinal cord or renal injury.
Our study is the largest up-to-date review on the hybrid approach for aortic arch diseases. However, it has the inherent limitations associated with meta-analyses. The great heterogeneity among studies regarding the patient’s characteristics and surgical methods are potential factors that can attenuate the pooled estimates. Furthermore, the lack of raw patient data is a prohibitive impediment for subset analysis (e.g., differences in outcomes in different aortic pathologies). In addition, a direct comparison between the two groups could not be appropriate as the applied methods have separate indications. However, a noteworthy observation is that despite the difference in terms of risk stratification between the two patients sets (as shown in Table 3), the outcomes were comparable.
It is still debatable whether a hybrid technique is comparable to total open repair, as the former strategy is reserved for high-risk patients who are unable to withstand an open repair. According to the available literature and taking into account the less invasive nature of hybrid repair, it could be speculated that short-term mortality and morbidity should appear to be reduced in hybrid repair patients. A recent meta-analysis attempted to elucidate this issue (53). However, it was based on four non-randomized observational studies, which makes the analysis prone to selection and patient profile biases. Surprisingly, this study showed that a hybrid repair did not significantly improve operative mortality, whereas it was associated with a slight but non-significant increase in permanent neurologic deficits. A non-significant trend towards increased late mortality was observed in the hybrid group.
Conclusions
Hybrid arch techniques provide a safe alternative to open repair with acceptable short- and mid-term results. However, stroke and mortality rates remain noteworthy. Future prospective trials that compare open conventional techniques with the hybrid method or the entirely endovascular method are needed.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Bachet J, Guilmet D, Goudot B, et al. Antegrade cerebral perfusion with cold blood: a 13-year experience. Ann Thorac Surg 1999;67:1874-8; discussion 1891-4.
- Di Eusanio M, Schepens MA, Morshuis WJ, et al. Separate grafts or en bloc anastomosis for arch vessels reimplantation to the aortic arch. Ann Thorac Surg 2004;77:2021-8. [PubMed]
- Yang J, Xiong J, Liu X, et al. Endovascular chimney technique of aortic arch pathologies: a systematic review. Ann Vasc Surg 2012;26:1014-21. [PubMed]
- Czerny M, Weigang E, Sodeck G, et al. Targeting landing zone 0 by total arch rerouting and TEVAR: midterm results of a transcontinental registry. Ann Thorac Surg 2012;94:84-9. [PubMed]
- Holt PJ, Johnson C, Hinchliffe RJ, et al. Outcomes of the endovascular management of aortic arch aneurysm: implications for management of the left subclavian artery. J Vasc Surg 2010;51:1329-38. [PubMed]
- Sun L, Qi R, Zhu J, Liu Y, et al. Total arch replacement combined with stented elephant trunk implantation: a new “standard” therapy for type a dissection involving repair of the aortic arch? Circulation 2011;123:971-8. [PubMed]
- Jakob H, Tsagakis K, Pacini D, et al. The International E-vita Open Registry: data sets of 274 patients. J Cardiovasc Surg (Torino) 2011;52:717-23. [PubMed]
- Borst HG, Walterbusch G, Schaps D. Extensive aortic replacement using “elephant trunk” prosthesis. Thorac Cardiovasc Surg 1983;31:37-40. [PubMed]
- Mitchell RS, Ishimaru S, Ehrlich MP, et al. First International Summit on Thoracic Aortic Endografting: roundtable on thoracic aortic dissection as an indication for endografting. J Endovasc Ther 2002;9:II98-105. [PubMed]
- Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000;283:2008-12. [PubMed]
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177-88. [PubMed]
- Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088-101. [PubMed]
- Andersen ND, Williams JB, Hanna JM, et al. Results with an algorithmic approach to hybrid repair of the aortic arch. J Vasc Surg 2013;57:655-67; discussion 666-7. [PubMed]
- Antoniou GA, Mireskandari M, Bicknell CD, et al. Hybrid repair of the aortic arch in patients with extensive aortic disease. Eur J Vasc Endovasc Surg 2010;40:715-21. [PubMed]
- Bavaria J, Milewski RK, Baker J, et al. Classic hybrid evolving approach to distal arch aneurysms: toward the zone zero solution. J Thorac Cardiovasc Surg 2010;140:S77-80; discussion S86-91.
- Bergeron P, Mangialardi N, Costa P, et al. Great vessel management for endovascular exclusion of aortic arch aneurysms and dissections. Eur J Vasc Endovasc Surg 2006;32:38-45. [PubMed]
- Canaud L, Hireche K, Berthet JP, et al. Endovascular repair of aortic arch lesions in high-risk patients or after previous aortic surgery: midterm results. J Thorac Cardiovasc Surg 2010;140:52-8. [PubMed]
- Chan YC, Cheng SW, Ting AC, et al. Supra-aortic hybrid endovascular procedures for complex thoracic aortic disease: single center early to midterm results. J Vasc Surg 2008;48:571-9. [PubMed]
- Chiesa R, Melissano G, Tshomba Y, et al. Ten years of endovascular aortic arch repair. J Endovasc Ther 2010;17:1-11. [PubMed]
- Donas KP, Rancic Z, Lachat M, et al. Novel sutureless telescoping anastomosis revascularization technique of supra-aortic vessels to simplify combined open endovascular procedures in the treatment of aortic arch pathologies. J Vasc Surg 2010;51:836-41. [PubMed]
- Deriu G, Grego F, Frigatti P, et al. Unusual inflow sources and device introduction sites in aortic arch debranching. J Cardiovasc Surg (Torino) 2012;53:143-51. [PubMed]
- Ferrero E, Ferri M, Viazzo A, et al. Is total debranching a safe procedure for extensive aortic-arch disease? A single experience of 27 cases. Eur J Cardiothorac Surg 2012;41:177-82. [PubMed]
- Geisbüsch P, Kotelis D, Müller-Eschner M, et al. Complications after aortic arch hybrid repair. J Vasc Surg 2011;53:935-41. [PubMed]
- Gelpi G, Vanelli P, Mangini A, et al. Hybrid aortic arch repair procedure: reinforcement of the aorta for a safe and durable landing zone. Eur J Vasc Endovasc Surg 2010;40:709-14. [PubMed]
- Gottardi R, Funovics M, Eggers N, et al. Supra-aortic transposition for combined vascular and endovascular repair of aortic arch pathology. Ann Thorac Surg 2008;86:1524-9. [PubMed]
- Hughes GC, Daneshmand MA, Balsara KR, et al. “Hybrid” repair of aneurysms of the transverse aortic arch: midterm results. Ann Thorac Surg 2009;88:1882-7; discussion 1887-8.
- Ingrund JC, Nasser F, Jesus-Silva SG, et al. Hybrid procedures for complex thoracic aortic diseases. Rev Bras Cir Cardiovasc 2010;25:303-10. [PubMed]
- Ishibashi H, Ishiguchi T, Ohta T, et al. Partial debranching hybrid stent graft for distal aortic arch aneurysms. Surg Today 2012;42:765-9. [PubMed]
- Lee CW, Beaver TM, Klodell CT Jr, et al. Arch debranching versus elephant trunk procedures for hybrid repair of thoracic aortic pathologies. Ann Thorac Surg 2011;91:465-71. [PubMed]
- Lotfi S, Clough RE, Ali T, et al. Hybrid repair of complex thoracic aortic arch pathology: long-term outcomes of extra-anatomic bypass grafting of the supra-aortic trunk. Cardiovasc Intervent Radiol 2013;36:46-55. [PubMed]
- Lu Q, Jing Z, Zhao Z, et al. Endovascular stent graft repair of aortic dissection type B extending to the aortic arch. Eur J Vasc Endovasc Surg 2011;42:456-63. [PubMed]
- Ma H, Yang HY, Zou JJ, et al. Management with the insufficient proximal landing zone for endovascular repair in aortic dissection. Chin Med J (Engl) 2011;124:3003-7. [PubMed]
- Murashita T, Matsuda H, Domae K, et al. Less invasive surgical treatment for aortic arch aneurysms in high-risk patients: a comparative study of hybrid thoracic endovascular aortic repair and conventional total arch replacement. J Thorac Cardiovasc Surg 2012;143:1007-13. [PubMed]
- Saleh HM, Inglese L. Combined surgical and endovascular treatment of aortic arch aneurysms. J Vasc Surg 2006;44:460-6. [PubMed]
- Vallejo N, Rodriguez-Lopez JA, Heidari P, et al. Hybrid repair of thoracic aortic lesions for zone 0 and 1 in high-risk patients. J Vasc Surg 2012;55:318-25. [PubMed]
- Weigang E, Parker J, Czerny M, et al. Endovascular aortic arch repair after aortic arch de-branching. Ann Thorac Surg 2009;87:603-7. [PubMed]
- Baraki H, Hagl C, Khaladj N, et al. The frozen elephant trunk technique for treatment of thoracic aortic aneurysms. Ann Thorac Surg 2007;83:S819-23; discussion S824-31.
- Chen X, Huang F, Xu M, et al. The stented elephant trunk procedure combined total arch replacement for Debakey I aortic dissection: operative result and follow-up. Interact Cardiovasc Thorac Surg 2010;11:594-8. [PubMed]
- Flores J, Kunihara T, Shiiya N, et al. Extensive deployment of the stented elephant trunk is associated with an increased risk of spinal cord injury. J Thorac Cardiovasc Surg 2006;131:336-42. [PubMed]
- Hofferberth SC, Newcomb AE, Yii MY, et al. Hybrid proximal surgery plus adjunctive retrograde endovascular repair in acute DeBakey type I dissection: superior outcomes to conventional surgical repair. J Thorac Cardiovasc Surg 2013;145:349-54; discussion 354-5. [PubMed]
- Hoffman A, Damberg AL, Schälte G, et al. Thoracic stent graft sizing for frozen elephant trunk repair in acute type A dissection. J Thorac Cardiovasc Surg 2013;145:964-9. [PubMed]
- Jim J, Moon MR, Rubin BG, et al. Hybrid repair of distal arch aortic aneurysms: endovascular elephant trunk completion. Ann Vasc Surg 2011;25:598-604. [PubMed]
- Kawaharada N, Kurimoto Y, Ito T, et al. Hybrid treatment for aortic arch and proximal descending thoracic aneurysm: experience with stent grafting for second-stage elephant trunk repair. Eur J Cardiothorac Surg 2009;36:956-61. [PubMed]
- Lima B, Roselli EE, Soltesz EG, et al. Modified and “reverse” frozen elephant trunk repairs for extensive disease and complications after stent grafting. Ann Thorac Surg 2012;93:103-9; discussion 109. [PubMed]
- Nishi H, Mitsuno M, Tanaka H, et al. Spinal cord injury in patients undergoing total arch replacement: a cautionary note for use of the long elephant technique. J Thorac Cardiovasc Surg 2011;142:1084-9. [PubMed]
- Pochettino A, Brinkman WT, Moeller P, et al. Antegrade thoracic stent grafting during repair of acute DeBakey I dissection prevents development of thoracoabdominal aortic aneurysms. Ann Thorac Surg 2009;88:482-9; discussion 489-90. [PubMed]
- Shi E, Gu T, Yu L, et al. Repair of Stanford type A aortic dissection with ascending aorta and hemiarch replacement combined with stent-graft elephant trunk technique by using innominate cannulation. J Thorac Cardiovasc Surg 2011;142:1458-63. [PubMed]
- Shimamura K, Kuratani T, Matsumiya G, et al. Long-term results of the open stent-grafting technique for extended aortic arch disease. J Thorac Cardiovasc Surg 2008;135:1261-9. [PubMed]
- Shimamura K, Kuratani T, Matsumiya G, et al. Hybrid endovascular aortic arch repair using branched endoprosthesis: the second-generation “branched” open stent-grafting technique. J Thorac Cardiovasc Surg 2009;138:46-52; discussion 52-3. [PubMed]
- Shrestha M, Pichlmaier M, Martens A, et al. Total aortic arch replacement with a novel four-branched frozen elephant trunk graft: first-in-man results. Eur J Cardiothorac Surg 2013;43:406-10. [PubMed]
- Uchida N, Katayama A, Tamura K, et al. Frozen elephant trunk technique and partial remodeling for acute type A aortic dissection. Eur J Cardiothorac Surg 2011;40:1066-71. [PubMed]
- Zhao HP, Zhu JM, Ma WG, et al. Total arch replacement with stented elephant trunk technique for acute type B aortic dissection involving the aortic arch. Ann Thorac Surg 2012;93:1517-22. [PubMed]
- Benedetto U, Melina G, Angeloni E, et al. Current results of open total arch replacement versus hybrid thoracic endovascular aortic repair for aortic arch aneurysm: a meta-analysis of comparative studies. J Thorac Cardiovasc Surg 2013;145:305-6. [PubMed]