A meta-analysis comparing bilateral internal mammary artery with left internal mammary artery for coronary artery bypass grafting
Introduction
Coronary artery bypass grafting (CABG) still remains the most common open cardiac surgery procedure performed worldwide today. The gold standard for CABG is the left internal mammary artery (LIMA) to the left anterior descending artery (LAD), as this conduit selection provides increased survival and freedom from myocardial infarction, symptoms, and reinterventions compared to a saphenous vein graft (SVG) to the same artery (1). Additionally, angiographic studies have shown late occlusion of the LIMA to LAD to be far less than that of a SVG to the LAD (2,3). The proposed mechanism for this increased patency and subsequent improved clinical outcome is due to the inherent characteristics of the internal mammary artery endothelium and improved run-off of the LAD territory (4-6).
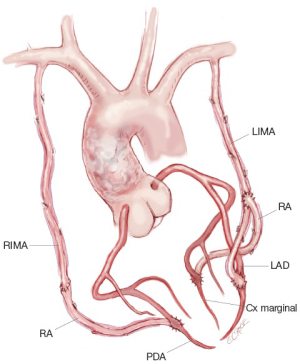
Often patients need more than one graft during a CABG procedure to bypass extensive disease in other coronary arteries. Given to the clearly demonstrated benefits of the LIMA on clinical and angiographic outcomes, the advantages and disadvantages of the bilateral internal mammary artery (BIMA) technique (Figure 1) have been rigorously studied through multiple retrospective and prospective cohort studies. A meta-analysis of seven observational studies that included 15,962 patients (11,269 LIMA and 4,693 BIMA) was performed in 2001 by Taggart et al. (7). In this landmark meta-analysis, the BIMA group demonstrated significantly better survival than the LIMA group [hazard ratio (HR), 0.81; 95% confidence interval (CI), 0.70-0.94]. This sparked an even greater number of non-randomized studies investigating long-term outcomes of BIMA versus LIMA in the general population of CABG patients as well as specific subpopulations.
Yet there still remains doubt as to whether BIMA is the better choice for patients in the long-term as the only randomized controlled trial (ART Trial) to date evaluating long-term survival is still ongoing (8). Additionally, only 4-12% of CABGs performed today use BIMA over a LIMA plus SVG, so clearly this is an example where evidence has not being translated into clinical practice (9,10). An updated meta-analysis was therefore undertaken as the studies included in the previous meta-analysis are few compared to the published literature to date and may have been confounded by patient selection bias as early use of the BIMA technique was often employed only in the young and low-risk patient populations.
We aimed to identify studies reporting clinical outcomes with BIMA versus LIMA to determine whether the use of BIMA has an increased long-term survival over other conduits. The primary outcome measured in this meta-analysis was survival.
Methods
Literature search strategy
Electronic searches were performed in three databases from January 1972 to December 2012: Medline (between 1972-2012), Embase (between 1980-2012), and the Cochrane Central Register of Controlled Trials (inception-2012). The final search was conducted on January 21, 2013. To achieve the maximum sensitivity of the search strategy and identify all studies, we searched the databases for publications containing the words: coronary, mammary or thoracic and artery; single, double, multiple, bilateral, unilateral, total or complete; and graft, bypass, revascularization, or reconstruction. These search terms included all search terms used in the original meta-analysis by Taggart et al. (7), plus additional keywords decided upon by the authors. Terms were searched in isolation or in combination with alternate forms, synonyms, abbreviations, or database indexing terms. All identified articles were systematically reviewed using the inclusion and exclusion criteria. Additionally, references from the final included studies were reviewed for further identification of potentially relevant studies that were missed in the original search.
Selection criteria
The same inclusion and exclusion criteria were used as in the original meta-analysis published by Taggart et al. (7). Eligible studies for this meta-analysis included those in which patient cohorts underwent CABG surgery utilizing the BIMA approach and the LIMA approach. We included published studies that investigated at least 100 patients in the BIMA cohort and 100 patients in the LIMA cohort. Furthermore, only those studies with a follow-up greater than 4 years were included. If multiple studies were published from the same center, only the last recorded publication with the most complete results was included. All non-English studies, duplicated studies, review articles, case reports, abstracts, conference presentations, editorials, and expert opinions were excluded.
The same endpoints and definition of endpoints were used as in the original publication. The primary outcome assessed was long-term survival and was defined as time from operation to death from any cause.
Data extraction and critical appraisal
Two authors (AJW and SZ) independently reviewed each article and determined inclusion of the studies for final analysis. All data were extracted from the relevant article texts, tables, and figures (AJW and SZ). Discrepancies between the two reviewers were resolved by discussion and consensus with a third author (TDY). A fourth author (DPT) confirmed the final results.
Statistical analysis
We used a random-effect meta-analysis. If a study did not report a specific variable it was not included in the overall average for that variable reported in this meta-analysis: mean follow-up (2,11-15), sex (16), diabetes (17), age (2), and ejection fraction (2,11,12,16-25). The HR and CI were extracted from all studies and included in the final analysis. This was accomplished through methods described in the previous meta-analysis (26). Specifically, the HR and CI of the following studies were derived from their total occurrence numbers and log-rank P-value: Joo et al. (27), Bonacchi et al. (28), and Danzer et al. (29); the HR and CI of the following studies were derived from their Kaplan-Meier survival projections along with initial population sizes assuming a fixed rate of censoring: Pick et al. (30), Berreklouw et al. (19), Lytle et al. (20), Jones et al. (17), Tarelli et al. (31), Dewar et al. (11), and Hirotani et al. (13) The overall study results by Dewar et al. (11) were obtained through a weighted average between the less than 60 years old patient group and greater than 60 years old patient group as described previously. In all cases where the prior meta-analysis yielded the latest HR and CI, the derivations were compared and no significant differences were detected as a result of the specified HR and CI that were used. For the remainder of the studies, the HR and CI were provided. Finally, the LN (HR) and standard error (SE) of LN (HR) were obtained from the HR and CI explicitly based on the same method used within the original meta-analysis.
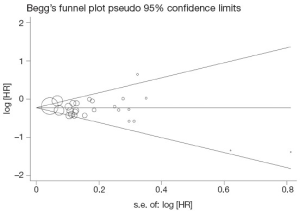
Evidence of publication bias was sought using the methods of Egger et al. (32) and Begg et al. (33). A contour-enhanced funnel plot was performed to aid in interpreting the funnel plot (34). If studies appear to be missing in areas of low statistical significance, then it is possible that the asymmetry is due to publication bias. If studies appear to be missing in areas of high statistical significance, then publication bias is a less likely cause of funnel asymmetry. Intercept significance was determined by the t-test suggested by Egger et al. (32). P<0.05 was considered representative of statistically significant publication bias. All statistical analyses were conducted with Review Manager version 5.2.1 (Cochrane Collaboration, Software Update, Oxford, United Kingdom) or STATA version 11.0 (Stata Corporation, College Station, TX).
Results
Literature search
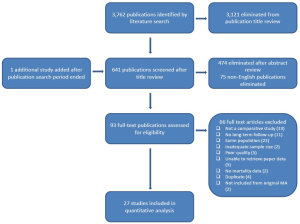
A total of 3,762 publications were identified through three electronic database searches (Figure 2). After exclusion of duplicate or irrelevant publications, 92 studies were retrieved. One additional study [Parsa et al. (15)] published after the final search was added as the authors felt its importance warranted inclusion. A thorough evaluation of all 93 studies resulted in 27 being included in the present meta-analysis (Table 1). Of these 27 studies, 25 were retrospective cohort studies and 2 were prospective cohort studies. No randomized controlled trials were eligible for inclusion in this meta-analysis. Out of the 7 studies included in the original meta-analysis by Taggart et al., 4 were included in this updated publication (the 3 studies that were not included were updated with more recent publications from the same center). The 27 studies included a total of 79,063 patients, of which 19,277 were BIMA and 59,786 were LIMA patients.

Full table
Demographics
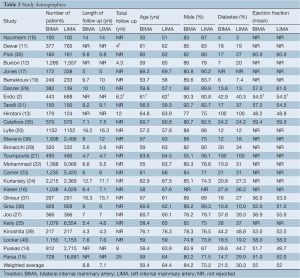
The studies consisted of on-pump CABG (n=11), off-pump CABG (n=2), and mixed (n=8) as the primary means for performing the operation. Six studies did not report how the procedure was performed (Table 1). Six of the 27 studies consisted of patient subsets, including: diabetic patients only (n=2), elderly patients only (n=2), unstable angina patients only (n=1), and right coronary artery anastomoses only (n=1). The exclusion criteria for each study are reported in Table 1. Table 2 details BIMA and LIMA demographics for all included studies. The majority of patients in these studies were male (76.8%): the BIMA group (84.2%) and the LIMA group (74.4%). The average age for all patients included was 63.2 years (BIMA 59.4 vs. LIMA 64.4 years). Diabetes was present in 28.1% of the entire population (BIMA 21.5% vs. LIMA 30.3%). Although not presented in 15 out of the 27 studies, the mean ejection fraction (EF) for the studies that did report this number was 0.53 (BIMA 0.55 vs. LIMA 0.52). The overall average length of follow-up for all studies that reported this result was 7.6 years: 8.8 years for BIMA patients and 7.1 years for LIMA patients.
Full table
Outcomes
Figure 3 presents the individual HRs for survival for all studies comparing BIMA versus LIMA. Of the 27 studies included in this meta-analysis, 13 had a statistically significant HR below unity. One study reported a statistically significant harmful effect for patients receiving a BIMA operation (35). However, after recalculating the results from this study we concluded that this was only a trend and not statistically significant (see Figure 3 Calafiore 2004). The results of the studies combined indicated a statistically significant benefit in survival for patients receiving BIMA versus LIMA for CABG (HR 0.78, CI: 0.72-0.84, I2=45%, P<0.00001).

Begg’s funnel plot and Egger’s test were performed to assess publication bias in the literature. All 27 included studies yielded a Begg’s test score of P=0.692 and an Egger’s test score of P=0.286, while inspection of the contour-enhanced funnel plot (Figure 4) showed no significant asymmetry. These results suggest that publication bias was not an influencing factor.
Discussion
The use of the internal mammary artery (IMA) for conduit selection has changed greatly since its initial introduction in the 1950s and 1960s. Initially, conduit choice favored SVGs over the IMA until seminal work by Loop et al. (1) in 1986 showed a distinct clinical advantage in favor of the LIMA. This led to the LIMA-LAD anastomosis to become the gold standard for CABG patients. With the survival benefit demonstrated by the LIMA-LAD, a small number of centers began using BIMAs more often as a grafting strategy since it was thought that the same benefit from the LIMA could be extrapolated to BIMA. Following this idea, a number of retrospective studies (12,20,36) demonstrated a survival advantage in patients receiving a BIMA. In this updated meta-analysis involving 27 observational studies comparing patients receiving BIMA versus LIMA grafts, we also show a statistically significant reduction in long-term mortality in the BIMA group.
This finding is in agreement with the previous meta-analysis by Taggart et al., who also demonstrated a survival benefit, albeit with only 7 studies and one-fifth of the 79,000 patients included in this current version. The studies that were included in this meta-analysis averaged almost 8 years of follow-up, with the longest study having follow-up at 25 years (15). Simply put, patients are living longer on average than ever before, and thus, it is important that they are given the additional benefit in long-term survival seen with a BIMA operation. Additionally, there was a combination of both on-pump and off-pump CABG procedures performed in the included studies. Two studies in this meta-analysis only included off-pump CABG patients, with one finding a statistically significant reduction in mortality and the other showing no difference (27,39). Although the debate about on-pump versus off-pump surgery is beyond the scope of this meta-analysis, it is interesting to note that the BIMA operation can be performed safely and possibly advantageously both ways.
In this meta-analysis, patients who received a BIMA as their primary graft strategy were on average younger, male, and non-diabetic. BIMA patients also had a slightly better mean EF (0.55 vs. 0.52) than those who only received a LIMA. The patient demographics of the original meta-analysis by Taggart et al. reflected surgical practice at the time, where BIMA was mostly performed in non-diabetic young patients. Our current study reflects a more state-of-the-art practice since close to one-third of all patients were diabetic, a risk factor often cited as a reason to preclude a BIMA. Despite this, the BIMA technique still demonstrated increased survival.
So with increasing evidence that shows long-term survival advantage for patients receiving BIMAs, why are so few patients undergoing this operation? The most often cited reason reported by cardiac surgeons is the belief that BIMA is associated with increased early morbidity and mortality (41,42), specifically the occurrence of deep sternal wound infection (DSWI) and the well-documented increased risk of death that accompanies it. DSWI has been reported to occur in as low as 0.3% and as high as 14% of BIMA procedures and is thought to be a result of the decreased sternal perfusion exacerbated by bilateral versus unilateral harvest of the IMA (38,43).
Additionally, due to referral patterns and changing patient demographics, more patients with diabetes, a risk factor often cited for DSWI, are undergoing CABG surgery than ever before. However, in diabetic patients, increased use of skeletonized harvesting techniques when performing a BIMA operation along with other infection prevention strategies have shown a reduction in DSWIs comparable to that seen in LIMA patients (44). The same reduction did not occur in BIMA operations performed through a pedicled harvest (44). Therefore, although the complexity of the operation increases with a skeletonized versus a pedicled harvest, the benefits of a BIMA operation can be realized while still maintaining a similar rate of DSWI seen in LIMA harvests.
While the success of the LIMA to LAD graft is well established, the decision as to where the right internal mammary artery (RIMA) should be used (right coronary artery versus circumflex) and how the RIMA should be used (in situ vs. free graft vs. ‘Y’ graft) has proven to be less straightforward. Traditionally, inferior rates of RIMA patency versus LIMA patency have been documented regardless of choice of graft site (45). A recent report by Kurlansky et al. demonstrated no difference in patients receiving an in situ RIMA to the left or right coronary system (46). Despite this, most surgeons will agree that if a RIMA is used in addition to a LIMA, the target vessel should have a significant stenosis with a good runoff in order to maintain long-term conduit patency.
Currently, the majority of patients still receive only LIMA, despite the fact that the best available evidence shows increased survival in patients receiving BIMAs. Although mostly speculative, and touched upon further in this issue by Lytle et al., the incentives for long-term prognosis often take a backseat to the more tightly regulated short-term morbidity and mortality. The BIMA operation is by all accounts a more arduous operation that requires more patience and surgical skill. In addition, the intense scrutiny of immediate patient outcomes following CABG surgery may force the surgeon to perform an operation that may be less beneficial in the long term but less risky in the short term. Lastly, the BIMA operation, along with total arterial revascularization strategies, are not easily taught as social and political pressures force the eldest, most experienced surgeon to perform the surgery instead of allowing younger surgeons to gain the required repetition necessary for excellence.
The present meta-analysis is limited by the nature of the studies included. No randomized controlled trials have yet to be reported with full long-term follow up and thus, only retrospective and prospective cohort studies were included in the final analysis. Whether taken singular or combined in a meta-analysis, observational studies suffer from a lack of control of confounding factors. The long-term results of the ART trial should provide more definitive answers, as it will be the first randomized controlled trial with long-term results comparing the outcomes between BIMA and LIMA patients. Additionally, as stated earlier, the group of patients that received BIMA grafting strategies tended to be younger, male, and non-diabetic, thus possibly biasing towards a better prognosis.
In conclusion, we demonstrate an increased survival among patients receiving BIMA versus those receiving LIMA for CABG surgery in a meta-analysis of 27 studies involving over 79,000 patients. Although it is important to tailor the operation to each individual patient, the benefit from this operative strategy can no longer be ignored and with decreasing rates of short-term morbidity (i.e., DSWI) via improved operative techniques, BIMA bypass grafting for patients needs to become a first-line option for patients receiving revascularization.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Loop FD, Lytle BW, Cosgrove DM, et al. Influence of the internal-mammary-artery graft on 10-year survival and other cardiac events. N Engl J Med 1986;314:1-6. [PubMed]
- Endo M, Nishida H, Tomizawa Y, et al. Benefit of bilateral over single internal mammary artery grafts for multiple coronary artery bypass grafting. Circulation 2001;104:2164-70. [PubMed]
- Dion R, Glineur D, Derouck D, et al. Long-term clinical and angiographic follow-up of sequential internal thoracic artery grafting. Eur J Cardiothorac Surg 2000;17:407-14. [PubMed]
- Gurné O, Chenu P, Buche M, et al. Adaptive mechanisms of arterial and venous coronary bypass grafts to an increase in flow demand. Heart 1999;82:336-42. [PubMed]
- Glineur D, Poncelet A. Fractional flow reserve of pedicled internal thoracic artery and saphenous vein grafts 6 months after bypass surgery. Eur J Cardiothorac Surg 2007;31:376-81. [PubMed]
- Walpoth BH, Schmid M, Schwab A, et al. Vascular adaptation of the internal thoracic artery graft early and late after bypass surgery. J Thorac Cardiovasc Surg 2008;136:876-83. [PubMed]
- Taggart DP, D’Amico R, Altman DG. Effect of arterial revascularisation on survival: a systematic review of studies comparing bilateral and single internal mammary arteries. Lancet 2001;358:870-5. [PubMed]
- Taggart DP, Altman DG, Gray AM, et al. Randomized trial to compare bilateral vs. single internal mammary coronary artery bypass grafting: 1-year results of the Arterial Revascularisation Trial (ART). Eur Heart J 2010;31:2470-81. [PubMed]
- Kappetein AP, Dawkins KD, Mohr FW, et al. Current percutaneous coronary intervention and coronary artery bypass grafting practices for three-vessel and left main coronary artery disease. Insights from the SYNTAX run-in phase. Eur J Cardiothorac Surg 2006;29:486-91. [PubMed]
- ElBardissi AW, Aranki SF, Sheng S, et al. Trends in isolated coronary artery bypass grafting: an analysis of the Society of Thoracic Surgeons adult cardiac surgery database. J Thorac Cardiovasc Surg 2012;143:273-81. [PubMed]
- Dewar LR, Jamieson WR, Janusz MT, et al. Unilateral versus bilateral internal mammary revascularization. Survival and event-free performance. Circulation 1995;92:II8-13. [PubMed]
- Buxton BF, Ruengsakulrach P, Fuller J, et al. Bilateral internal thoracic artery grafting may improve outcome of coronary artery surgery. Risk-adjusted survival. Circulation 1998;98:II1-6. [PubMed]
- Hirotani T, Nakamichi T, Munakata M, et al. Risks and benefits of bilateral internal thoracic artery grafting in diabetic patients. Ann Thorac Surg 2003;76:2017-22. [PubMed]
- Puskas JD, Sadiq A, Vassiliades TA, et al. Bilateral internal thoracic artery grafting is associated with significantly improved long-term survival, even among diabetic patients. Ann Thorac Surg 2012;94:710-5; discussion 715-6. [PubMed]
- Parsa CJ, Shaw LK, Rankin JS, et al. Twenty-five-year outcomes after multiple internal thoracic artery bypass. J Thorac Cardiovasc Surg 2013;145:970-5. [PubMed]
- Kieser TM,Lewin AM,Graham MM, et al. Outcomes associated with bilateral internal thoracic artery grafting: the importance of age. Ann Thorac Surg 2011;92:1269-75; discussion 1275-6. [PubMed]
- Jones JW, Schmidt SE, Miller CC 3rd, et al. Bilateral internal thoracic artery operations in the elderly. J Cardiovasc Surg (Torino) 2000;41:165-70. [PubMed]
- Naunheim KS, Barner HB, Fiore AC. 1990: Results of internal thoracic artery grafting over 15 years: single versus double grafts. 1992 update. Ann Thorac Surg 1992;53:716-8. [PubMed]
- Berreklouw E, Rademakers PP, Koster JM, et al. Better ischemic event-free survival after two internal thoracic artery grafts: 13 years of follow-up. Ann Thorac Surg 2001;72:1535-41. [PubMed]
- Lytle BW, Blackstone EH, Sabik JF, et al. The effect of bilateral internal thoracic artery grafting on survival during 20 postoperative years. Ann Thorac Surg 2004;78:2005-12; discussion 2012-4.
- Toumpoulis IK, Anagnostopoulos EC, Balaram S, et al. Does bilateral internal thoracic artery grafting increase long-term survival of diabetic patients? Ann Thorac Surg 2006;81:599-606. [PubMed]
- Mohammadi S, Dagenais F, Doyle D, et al. Age cut-off for the loss of benefit from bilateral internal thoracic artery grafting. Eur J Cardiothorac Surg 2008;33:977-82. [PubMed]
- Carrier M, Cossette M, Pellerin M, et al. Statin treatment equalizes long-term survival between patients with single and bilateral internal thoracic artery grafts. Ann Thorac Surg 2009;88:789-95; discussion 795. [PubMed]
- Kurlansky PA, Traad EA, Dorman MJ, et al. Thirty-year follow-up defines survival benefit for second internal mammary artery in propensity-matched groups. Ann Thorac Surg 2010;90:101-8. [PubMed]
- Kelly R, Buth KJ, Legare JF. Bilateral internal thoracic artery grafting is superior to other forms of multiple arterial grafting in providing survival benefit after coronary bypass surgery. J Thorac Cardiovasc Surg 2012;144:1408-15. [PubMed]
- Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med 1998;17:2815-34. [PubMed]
- Joo HC, Youn YN, Yi G, et al. Off-pump bilateral internal thoracic artery grafting in right internal thoracic artery to right coronary system. Ann Thorac Surg 2012;94:717-24. [PubMed]
- Bonacchi M, Maiani M, Prifti E, et al. Urgent/emergent surgical revascularization in unstable angina: influence of different type of conduits. J Cardiovasc Surg (Torino) 2006;47:201-10. [PubMed]
- Danzer D, Christenson JT, Kalangos A, et al. Impact of double internal thoracic artery grafts on long-term outcomes in coronary artery bypass grafting. Tex Heart Inst J 2001;28:89-95. [PubMed]
- Pick AW, Orszulak TA, Anderson BJ, et al. Single versus bilateral internal mammary artery grafts: 10-year outcome analysis. Ann Thorac Surg 1997;64:599-605. [PubMed]
- Tarelli G, Mantovani V, Maugeri R, et al. Comparison between single and double internal mammary artery grafts: results over ten years. Ital Heart J 2001;2:423-7. [PubMed]
- Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-34. [PubMed]
- Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088-101. [PubMed]
- Palmer TM, Peters JL, Sutton AJ, et al. Contour-enhanced funnel plots for meta-analysis. Stata J 2008;8:242-54.
- Calafiore AM, Di Giammarco G, Teodori G, et al. Late results of first myocardial revascularization in multiple vessel disease: single versus bilateral internal mammary artery with or without saphenous vein grafts. Eur J Cardiothorac Surg 2004;26:542-8. [PubMed]
- Stevens LM, Carrier M, Perrault LP, et al. Single versus bilateral internal thoracic artery grafts with concomitant saphenous vein grafts for multivessel coronary artery bypass grafting: effects on mortality and event-free survival. J Thorac Cardiovasc Surg 2004;127:1408-15. [PubMed]
- Glineur D, D’hoore W, Price J, et al. Survival benefit of multiple arterial grafting in a 25-year single-institutional experience: the importance of the third arterial graft. Eur J Cardiothorac Surg 2012;42:284-90; discussion 290-1. [PubMed]
- Grau JB, Ferrari G, Mak AWC, et al. Propensity matched analysis of bilateral internal mammary artery versus single left internal mammary artery grafting at 17-year follow-up: validation of a contemporary surgical experience. Eur J Cardiothorac Surg 2012;41:770-5; discussion 776. [PubMed]
- Kinoshita T, Asai T, Suzuki T, et al. Off-pump bilateral skeletonized internal thoracic artery grafting in elderly patients. Ann Thorac Surg 2012;93:531-6. [PubMed]
- Locker C, Schaff HV, Dearani JA, et al. Multiple arterial grafts improve late survival of patients undergoing coronary artery bypass graft surgery: analysis of 8622 patients with multivessel disease. Circulation 2012;126:1023-30. [PubMed]
- Catarino PA, Black E, Taggart DP. Why do UK cardiac surgeons not perform their first choice operation for coronary artery bypass graft? Heart 2002;88:643-4. [PubMed]
- Mastrobuoni S, Gawad N, Price J, et al. Use of bilateral internal thoracic artery during coronary artery bypass graft surgery in Canada: The bilateral internal thoracic artery survey. J Thorac Cardiovasc Surg 2012;144:874-9. [PubMed]
- Kai M, Hanyu M, Soga Y, et al. Off-pump coronary artery bypass grafting with skeletonized bilateral internal thoracic arteries in insulin-dependent diabetics. Ann Thorac Surg 2007;84:32-6. [PubMed]
- Deo SV, Shah IK, Dunlay SM, et al. Bilateral internal thoracic artery harvest and deep sternal wound infection in diabetic patients. Ann Thorac Surg 2013;95:862-9. [PubMed]
- Galbut DL, Traad EA, Dorman MJ, et al. Seventeen-year experience with bilateral internal mammary artery grafts. Ann Thorac Surg 1990;49:195-201. [PubMed]
- Kurlansky PA, Traad EA, Dorman MJ, et al. Location of the second internal mammary artery graft does not influence outcome of coronary artery bypass grafting. Ann Thorac Surg 2011;91:1378-83; discussion 1383-4. [PubMed]