Mid-term results of the Radial Artery Patency and Clinical Outcomes randomized trial
Introduction
In the 1990s, a resurgence of interest in alternatives to the saphenous vein (SV) and an awareness of published impressive results with the radial arteries used by Carpentier’s group more than a decade earlier led to some encouraging early experience with the radial artery (RA). This was perceived as a viable alternative to the SV, or to the right internal thoracic artery (RITA), which was being studied by other groups as a second arterial conduit. A randomized trial was conceived to identify the correct place of the RA in the hierarchy of conduits.
Patients and methods
The design of the trial has been reported extensively elsewhere (1). The primary aim of Radial Artery Patency and Clinical Outcomes (RAPCO) Trial was to assess the long-term patency and clinical outcomes of the RA, free RITA and SV when grafted to the largest non-LAD (left anterior descending) target. RAPCO enrolled a total of 619 patients into two trial arms. All patients received the gold standard in situ left internal thoracic artery (LITA) to the LAD. Group 1 comprised patients aged younger than 70 years (or <60 years if diabetic) who were randomized to receive either the RA or free RITA to the largest non-LAD target. Group 2 enrolled patients ≥70 years who were randomized to either RA or SV to the largest non-LAD target. Any 3rd or 4th order grafts usually employed the SV or occasionally the RA. (See Protocol Summary: Table 1).
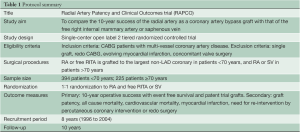
Full table
Patients receive an annual telephone and clinical review for at least 10 years after surgery. Using a second random assignment, protocol-directed angiograms were allocated at intervals of 1, 2, 5, 7 and 10 years, with the bulk weighted to the second-half of the follow-up as this was anticipated to coincide with the majority of graft occlusion events. In addition, elective angiograms at the 5- and 10-year mark were offered to all patients. Computerized tomography angiography (CTA) was offered in the minority of cases where the protocol or elective femoral angiograms were refused.
All angiograms were reported independently by three cardiac specialists, including at least one cardiologist and one cardiac surgeon. Graft failure was defined as occlusion, >80% stenosis or string sign, and recorded along with any pathologic findings at the proximal or distal anastomoses. Any disputed findings were further assessed by a fourth independent observer. Severity of native vessel disease is similarly assessed by the three observers, with the native vessels divided into proximal, mid and distal sections, and the location and percent stenosis recorded. The latter was recorded in the database as the mean of the 3 estimations.
This design has some obvious strengths and weaknesses. The use of protocol directed angiography, rather than symptom driven, allows for estimations of real world patency. By its nature, symptom-directed angiography overestimates graft failure and cannot be extrapolated to the post-operative majority who are symptom-free. The staggering of the time points of angiography from one month to 10 years allows construction of Kaplan-Meier estimates of failure or patency over time, and recognizes that graft failure may be clustered around particular periods rather than evenly distributed along a time continuum. The addition of fixed time points for supplementary angiography at 5- and 10-years provides more precise patencies at these time-points, rather than calculated estimations. However, their later addition to the protocol necessitated that these tests be optional, given that not all patients would wish to undergo more than one angiogram. These supplementary studies also offered relief and reassurance to many patients whose protocol angiogram fell very early or late in the decade of follow up, and to those anxious about the status of their coronary grafts during clinical follow up. The use of hard clinical endpoints (death, myocardial infarction, repeat revascularisation) eliminates subjectivity from clinical status and is easily standardized during the annual telephone review. However, other endpoints such as usage of antianginal medication and current NYHA class may also be reproducible during follow-up and may have provided additional evidence of clinical outcomes with different conduits.
From the outset it was determined that if one wanted to study the properties and performance of a conduit, other variables needed to be eliminated. For the comparison with the RITA, this meant that both conduits would need to be used as free grafts with the same complement of proximal and distal anastomoses, given that each introduces a risk of failure. Both would need to be grafted to a similar runoff, which is difficult to achieve given variations in coronary anatomy and dominance. Rather than select a fixed target (such as the posterior descending artery or first marginal branch), a more pragmatic approach is to choose targets with comparable importance if not the same precise anatomical location. Hence it was determined to graft the trial conduit with the largest or most important non-LAD target, based on size and area of subtended myocardium.
While it is acknowledged that there were some limitations to this design, these were inevitable if other variables were to be avoided and meaningful comparisons to be made. Although the RITA was used as a free graft to right or left-sided targets, subsequent data suggest that the optimum configuration for bilateral internal thoracic arteries (ITA) is when used as in situ grafts, which have only one anastomoses and thus removes the risk of technical error at the proximal end. This may easily occur given the size and wall thickness disparity between aorta and ITA, which makes this anastomosis technically challenging. While leaving both ITAs innervated may have potential implications for synthetic and autoregulatory functions, their greatest benefit may be achieved when grafted to the left side, as discussed by Lytle, Taggart and others.
Similarly, the selection of the second target for the trial conduit has the disadvantage that each patient receives only one trial conduit, with obvious implications for power calculations. An intriguing alternative design was adopted for the contemporaneous Canadian Radial Artery Patency Study (RAPS) trial, in which the RA and SV are randomized to being grafted with the circumflex or right coronary targets respectively. As such, each patient has effectively two trial conduits, with one serving as the control and thereby eliminating many variables. A downside of their model is that it eliminates any differences in the clinical outcomes because of the identical grafts (2,3).
Results
Publication of results
The trial remains in progress and final data will not be obtained until late 2014 (recruitment having occurred 1996-2004) and is likely to be reported in 2015. The mid-term clinical outcomes of the two groups were presented and published via the Society of Thoracic Surgeons in 2007 (4), and the European Association for Cardio-Thoracic Surgery in 2008 (5). The mid-term patency results were presented and published via the American Association for Thoracic Surgery (AATS) (6). The last RAPCO interim report attracted some attention, and was listed as the leading publication for that year by the surgical division of the American Heart Association’s scientific awards for 2010. This underscores the interest in the identification of the optimal conduit strategy for what is the specialty’s benchmark and commonest procedure. It was agreed not to reinterrogate the database thereafter for primary endpoints between mid-term and trial closure, as repeated data “trawling” may further reduce the power of a trial.
Mid-term results
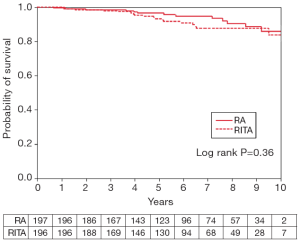
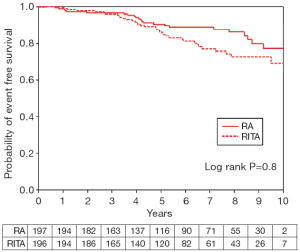
Mid-term results presented to date are detailed below. The demographic data, clinical urgency and number of grafts performed is shown in Figure 1A,B. This confirms that the arms in each group were well matched with each other. The clinical outcome data of group 1 showed equivalent actuarial survival at mean 6-year follow up, with no significant difference in all cause or cardiovascular mortality (Figure 2) (4). There were 3 and 6 myocardial infarctions in the RA and RITA arms respectively, though interestingly none of these were in the territory of the study graft. Nine and 11 patients required revascularisation, with target vessel revascularisation rates only 3 out of 198 and 4 out of 196 patients in the RA and RITA arms respectively. When clinical events and mortality were combined to calculate event-free survival, there was a trend towards superior outcomes in the RA arm (Figure 3) but this did not achieve significance, with 24 versus 37 patients reaching a clinical endpoint in the RA and RITA arms respectively.

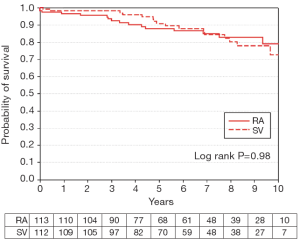
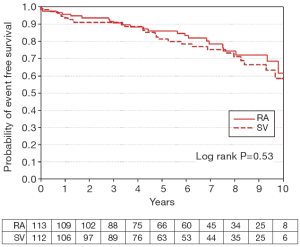
Comparable clinical outcome data for the older cohort in group 2, with mean 6-year follow up, showed similar findings when the RA was compared with SV in older patients (5). There was no difference in actuarial survival (Figure 4) with only 9 and 13 patients reaching a clinical endpoint in the RA and SV groups respectively, resulting in no difference in event-free survival (Figure 5). Although there was also no difference in myocardial infarction nor revascularization, target vessel revascularisation rates were 1 out of 113 (0.9%) versus 4 out of 110 (3.6%), but this possible excess of target vessel revascularisation in the SV group did not achieve significance due to the small numbers of events. There were 4 myocardial infarcts in each group, but only one of these was in the territory of a study graft.
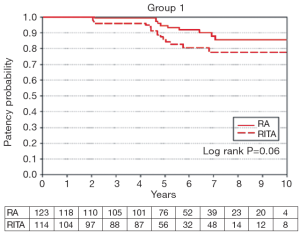
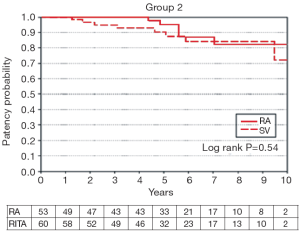
Angiographic patency at mean interval 5.5 years between surgery and restudy (range, 0.1-11.2 years) was presented at AATS 2008 (5). Graft failures were equal in Group 1 (13/122 and 12/105 for the RA and RITA respectively), with 7 of these failures in each group being due to occlusion and the remainder string sign (Figure 6). In Group 2, failures were identified in 4/51 RAs and 9/59 SVs, with RA failures equally due to occlusion and string sign, whilst all but one of the failed vein grafts were occluded, with one having high grade stenosis. The apparent small difference in graft failure rate in Group 2 did not achieve significance, but larger numbers will be available for analysis at trial termination at 10 years (Figure 7).
In summary, at mid-term no significant differences in clinical outcome or graft patency have been recorded when comparing the RA and free RITA in younger patients, or the RA and SV in older patients. The negative finding at mid-term stems primarily from the excellent performance of the vein grafts to date, which exceeded previous reports on which power calculations were based. This may be due to careful conduit selection, atraumatic handling, early pharmacological protection, secondary prevention measures and modern medical therapy, or a combination of these. Arterial conduits have performed in line with several previous reportsas well as the contemporaneous RAPS trial.
It must be recognized that the second half of the trial may be more informative, as power will improve with the bulk of the angiography occurring in this second phase. As previous reports suggest, this may be the period in which time-dependent vein graft attrition may occur. For younger patients with a life expectancy of a decade or more, the final trial results may still be highly relevant.
Discussion
The RAPCO results will need to be placed in context alongside other important recent trials (2,3,7,8) and those in progress, most notably the Arterial Revascularisation Trial (ART) of Taggart et al. (9), which randomized patients to bilateral ITA or single ITA and other conduit (commonly RA) to revascularize the left side. Not only will ART offer the best possible evidence regarding whether two ITAs grafted to the left circulation affords a superior long-term survival, it will also offer some comparative data regarding the outcome after a LITA + RA strategy, in other words a cohort within ART which is analogous to Group 1 in RAPCO. Given the greater numbers and multicenter nature of ART, this may help place RAPCO’s final results in context and define whether the findings of RAPCO (a single center trial with meticulous post operative follow-up) may be generalized to the wider international population.
Studies within RAPCO
The value of RAPCO has already extended beyond the primary trial, and several completed sub-studies and some others in progress. The database provides a defined pool of patients whose preoperative demographics, angiographic findings, and operative details (including configuration of grafts and quality of targets) are known. Post-operative angiography has recorded the state of the grafts and of the native circulation. Coronary segments are identified and numbered, such that changes in lesions from the preoperative angiogram over time can be identified. Pre and post-operative angiograms have been separately reported by three observers, and an average estimation of disease taken to minimize single observer bias without the prohibitive time and cost constraints of quantitative computerized image analysis. Supplementary post-operative information has been obtained by researchers regarding continued smoking, new diabetes and annual serum lipid measurements, which can be correlated with the progression and regression of native vessel disease and the fate of coronary grafts. Several of these substudies are briefly summarized.
All comers coronary graft patency at 5 years: observational data from a randomized trial (10)
This studied analyzed the 5-year angiographic findings, derived from both optional mid-term supplementary angiograms and protocol-directed angiography, recognizing that with different triggers for the angiography, the findings might be different. In summary, in protocol angiography scheduled at the 5-year mark, patency of the in situ ITA grafts and free arterial grafts was 95.5% (210 of 220) and 91.4% (150 of 164) respectively, which did not differ significantly (P=0.13). SV graft patency was 83.0% (191 of 230) with a trend to higher failure rate compared with free arterial grafts (P=0.07), and was significantly lower than that of in situ ITA grafts (P=0.01). In the optional 5-year supplementary angiograms, outcomes were similar to the protocol-directed findings, with patency of in situ left and right ITA grafts of 95.8% (204 of 213), which was significantly greater than that of the other two groups (P=0.02 and P<0.001 respectively). Patency of free arterial conduits and SV grafts was 89.1% (139 of 156) and 82.4% (201 of 244), respectively, which did not differ significantly (P=0.09) at 5 years.
This sub-study provided hard, real world data for all conduits of first to fourth order grafts and thereby offered an observational overview of likely graft patency in the current era of predominately asymptomatic patients, in contrast to symptom-directed studies that may overestimate the incidence of graft failure. Interestingly, despite being the earliest substudy of all RAPCO related publications, its simple figures and data are the most widely reproduced in other presentations or publications pertaining to coronary graft patency.
The fate of moderate lesions, grafted and ungrafted (11)
Lesions of 40-69% were identified in 10% (386/3,816) of coronary vessels for which pre- and post-operative angiography was available. The majority of these (323/386) were grafted. In all territories, grafted vessels had a much greater risk of disease progression than ungrafted equivalents (43.4% vs. 10.5%, P<0.001). Moderate lesions behaved differently from more severe counterparts as they were more likely to remain unchanged on follow-up angiography (52.6% vs. 31.1%, P<0.001). Only 1 in 7 moderate lesions in the ungrafted right coronary artery exhibited significant progression during followup, whereas the likelihood of progression in left-sided counterparts approached 50%. Arterial and vein grafts to left-sided moderately stenosed vessels had excellent patency (83% and 77% at 8 years respectively), which was significantly better than that of right-sided grafts. Placement of a graft for a moderate lesion was associated with significantly greater incidence of disease progression, most marked in the right coronary territory. We concluded that during primary coronary artery bypass grafting (CABG), it was reasonable to graft left-sided moderate lesions, given that almost half of them will progress and the graft will likely have a high degree of patency. In contrast, right-sided lesions could be left ungrafted given their low risk of progression if left untouched and the poorer patency of the graft (whose effect may also be to substantially increase disease progression elsewhere in the vessel). This finding was presented in a plenary session of the AATS 2012 meeting and published thereafter with its discussion by Joseph Sabik (11).
The impact of post-operative lipid exposure on arterial and venous coronary grafts (12)
Serum lipid assays were obtained retrospectively from pathology databases and the mean annualized lipid exposure for each patient was calculated. Angiographic and clinical data were analyzed against lipid exposure. Overall, only HDL cholesterol levels were inversely correlated with graft failure, with total cholesterol and LDL showing no associations in a mixed pool of arterial and venous grafts. Venous graft failure was associated with increased total cholesterol/HDL (P=0.006) and LDL/HDL (P=0.032). In contrast, elevated total cholesterol correlated with a reduced risk of arterial graft failure (or for graft failure 0.705, P=0.023) with increasing LDL cholesterol following a similar trend (OR for graft failure 0.729, P=0.051). The findings of this sub-study suggest that arterial grafts are superior to veins in terms of their lipid resistance. Given that patients may not achieve national lipid targets in clinical practice, this data further supports the greater use of arterial conduits in coronary revascularization. These findings were presented at the European Society of Cardiology in 2012.
Prevalence of disease regression after primary coronary surgery (13)
We identified 1,760 individual native coronary vessels with pre-operative stenosis of at least 40% and characterized patterns of disease regression within these vessels. The overall prevalence of disease regression was 19.5%, corresponding with 45.2% of all patients demonstrating regression in one or more native coronary arteries. The presence of an arterial graft increased the likelihood of native vessel disease regression (21.2% compared with 15.9% for venous bypassed vessels, P=0.012), as did location in the left circulation (22.4% compared with 13.7% for the right circulation, P<0.001) and increased severity (≥70%) of the pre-existing lesion (21.9% regression rate compared with 9.8% for moderate lesions of 40-69% stenosis, P<0.001). Native vessel disease regression after CABG is common and affected by conduit type, vessel location and pre-operative lesion severity. These factors may offer some guidance for surgeons when assessing requirement for bypass grafts in a borderline lesion.
Patient satisfaction with RA and SV harvest sites (14)
Patients from RAPCO were asked to complete a questionnaire regarding their satisfaction with RA or SV harvest pre-operatively, at three months and after almost 10 years post-operatively (mean 9.3 years). Responses were graded and compared between each of the time points. In patients who had received a RA graft group, 92% to 99% reported no significant symptoms after 9.3 years. The most frequent concerns were related to pain and numbness (8% each), but this was not significantly higher than in those who had not had a RA harvested. Among the RA group, mean scores for scar appearance and discomfort at the harvest site were 0.95 and 0.93 respectively (where 1 = no concern), suggesting satisfactory cosmesis and no impact on function. Symptom severity was significantly worse in 6 out of 7 questions when compared to pre-operative responses and in 4 out of 7 items compared to the 3-month follow up, indicating a general deterioration in function over long term follow up. In those who had both a RA and SV graft, patients reported more scar discomfort associated with SV harvest both at 3 months (1.69 vs. 1.34, P<0.001) and after long term follow up (1.21 vs. 0.97, P=0.002). We conclude that RA harvesting is associated with higher patient satisfaction and less scar discomfort than SV removal. Overall, upper limb functionality declines with time but this is not different to those without artery removal and may therefore be unrelated to the effects of surgery.
Attainment of lipid targets after coronary artery bypass surgery (15)
In this study, we examined the proportion of patients who achieved National Heart Foundation lipid targets during almost a decade of follow up after coronary artery surgery. Target levels for total cholesterol, HDL-C, LDL-C and triglycerides were attained pre-operatively by 16%, 64%, 14% and 39% respectively. After follow up, these figures remained suboptimal at 24%, 83%, 20% and 53%. Of the 141 diabetic patients, target attainment was significantly higher for total cholesterol (31%; P=0.038) and LDL-C (28%; P=0.006) but lower for HDL-C (75%; P=0.002) and triglycerides (40%; P<0.001) compared to non-diabetic patients. Despite some improvements during careful surveillance of a cohort of CABG patients, the majority have not achieved non-HDL national lipid targets in their cumulative lipid exposure during a decade of follow up, with half of the cohort remaining above recommended levels at last review.
The final results of RAPCO will provide the first long-term randomized comparison of the RA, free RITA and SV as the second graft. This is needed as the results of non-randomized series have suffered from selection bias with RA being used in preference to SV in younger fitter patients for which propensity matching can only incompletely account. Furthermore, RAs and RITAs are being used in different institutions with multiple practice differences, thus confounding any interpretation of discrepancy in outcomes. As such, the final results of RAPCO are eagerly awaited. In addition, the trial database has facilitated studies of various subsets and offered a valuable insight into the natural history of grafted and ungrafted coronary artery disease, findings which may prove to be as important as the trial results themselves.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Buxton BF, Raman JS, Ruengsakulrach P, et al. Radial artery patency and clinical outcomes: five-year interim results of a randomized trial. J Thorac Cardiovasc Surg 2003;125:1363-71. [PubMed]
- Desai ND, Naylor CD, Kiss A, et al. Impact of patient and target-vessel characteristics on arterial and venous bypass graft patency: insight from a randomized trial. Circulation 2007;115:684-91. [PubMed]
- Deb S, Cohen EA, Singh SK, et al. Radial artery and saphenous vein patency more than 5 years after coronary artery bypass surgery: results from RAPS (Radial Artery Patency Study). J Am Coll Cardiol 2012;60:28-35. [PubMed]
- Hayward PA, Hare DL, Gordon I, et al. Which arterial conduit? Radial artery versus free right internal thoracic artery: six-year clinical results of a randomized controlled trial. Ann Thorac Surg 2007;84:493-7; discussion 497. [PubMed]
- Hayward PA, Hare DL, Gordon I, et al. Effect of radial artery or saphenous vein conduit for the second graft on 6-year clinical outcome after coronary artery bypass grafting. Results of a randomised trial. Eur J Cardiothorac Surg 2008;34:113-7. [PubMed]
- Hayward PA, Gordon IR, Hare DL, et al. Comparable patencies of the radial artery and right internal thoracic artery or saphenous vein beyond 5 years: results from the Radial Artery Patency and Clinical Outcomes trial. J Thorac Cardiovasc Surg 2010;139:60-5; discussion 65-7. [PubMed]
- Collins P, Webb CM, Chong CF, et al. Radial artery versus saphenous vein patency randomized trial: five-year angiographic follow-up. Circulation 2008;117:2859-64. [PubMed]
- Goldman S, Sethi GK, Holman W, et al. Radial artery grafts vs saphenous vein grafts in coronary artery bypass surgery: a randomized trial. JAMA 2011;305:167-74. [PubMed]
- Taggart DP, Altman DG, Gray AM, et al. Randomized trial to compare bilateral vs. single internal mammary coronary artery bypass grafting: 1-year results of the Arterial Revascularisation Trial (ART). Eur Heart J 2010;31:2470-81. [PubMed]
- Hayward PA, Buxton BF. Contemporary coronary graft patency: 5-year observational data from a randomized trial of conduits. Ann Thorac Surg 2007;84:795-9. [PubMed]
- Hayward PA, Zhu YY, Nguyen TT, et al. Should all moderate coronary lesions be grafted during primary coronary bypass surgery? An analysis of progression of native vessel disease during a randomized trial of conduits. J Thorac Cardiovasc Surg 2013;145:140-8; discussion 148-9. [PubMed]
- Zhu YY, Hayward PA, Hare DL, et al. Lipid management in high risk coronary patients: how effective are we at secondary intervention? Heart Lung Circ 2012;21:82-7. [PubMed]
- Zhu YY, Trong NT, Buxton BF, et al. Regression of coronary disease after bypass surgery: urban myth or common finding? Insights from angiographic surveillance in a randomised trial of coronary bypass surgery. J Thorac Cardiovasc Surg. [Epub ahead of print].
- Zhu YY, Hayward PA, Hadinata IE, et al. Long-term impact of radial artery harvest on forearm function and symptoms: a comparison with leg vein. J Thorac Cardiovasc Surg 2013;145:412-9. [PubMed]
- Zhu YY, Hayward PA, Hare DL, et al. Effect of lipid exposure on graft patency and clinical outcomes: arteries and veins are different. Eur J Cardiothorac Surg 2013. [Epub ahead of print]. [PubMed]





