How do we use imaging to aid considerations for intervention in patients with severe mitral regurgitation?
Echo-timing for surgical intervention
The statistics don’t lie. Valvular Heart Disease (VHD) is becoming a major epidemic in industrialized countries worldwide, partially due to increasing life expectancies and comorbid conditions (1). Degenerative mitral valve disease is the most prevalent, accounting for nearly 10% of VHD in those industrialized countries.
It is well known that left untreated, significant longstanding degenerative mitral regurgitation (MR) is associated with marked morbidity and decreased quality of life. The seminal work by Sarano et al. showed that asymptomatic patients with severe degenerative MR [quantitated by a calculated effective regurgitant orifice [(ERO) of ≥40 mm2] have only a 36% chance of being alive or asymptomatic without heart failure or atrial fibrillation at five years from initial diagnosis (2). It is also recognized that approximately 30-40% of patients with severe degenerative MR managed medically will reach indications for surgical intervention within five years. At that point, patients may have developed subclinical or clinical left ventricular dysfuntion, atrial fibrillation, or even pulmonary hypertension—all of which may be difficult to reverse, even with excellent surgery (Table 1).
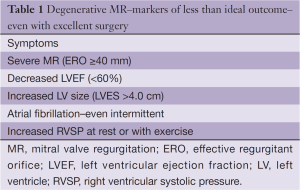
Full table
Emanating from early work by Barlow (3) and Carpentier (4) have been dramatic advances in our understanding of the pathophysiology of degenerative mitral valve disease and its effect on cardiac structure and function. Simultaneously, there have been important advances in mitral valve reparative surgery as elucidated by Carpentier, Adams, David and others (5-7).
Concurrently, there have been significant developments in diagnostic imaging as it relates to mitral valve disease. While Computerized Tomography and Magnetic Resonance Imaging have played and will continue to play important roles in the diagnosis of mitral valve disease, echocardiography is the central non-invasive procedure for the diagnosis and management of mitral valve disease. Today echocardiography encompasses Transthoracic Echocardiography (TTE, 2D and 3D), Stress Echocardiography (increasingly important in evaluation of patients with presumed “asymptomatic” VHD), and Transesophageal Echo (TEE, 2D and 3D). Utilizing all facets of echocardiography, both the clinician and the surgeon can properly diagnose primary valvular (degenerative) MR versus secondary (functional–ischemic) MR. Additionally, the echocardiographic study can determine the severity of the regurgitant lesion, its impact on left and right ventricular (RV) function and size, left atrial size and function, and importantly, the presence or absence of pulmonary-RV systolic hypertension. Echocardiography also plays an important role in evaluating the tricuspid valve and tricuspid annulus. Beyond these diagnostic capabilities, echocardiography—especially 3-D TEE—plays a critical role in the operating room in assessing the effectiveness of surgical interventions on the mitral valve, which is key to predicting long-term outcomes.
Despite these advances, there is continuing debate about the proper timing for surgical intervention, especially mitral valve repair, for significant valvular degenerative MR. In fact, appropriate surgical intervention is often delayed (8). The current guidelines (9,10) state that the onset of symptoms (Class I) and/or left ventricular dysfunction [left ventricular ejection fraction (LVEF) ≤60%] (Class I) are the appropriate timing triggers for surgical intervention, thus relegating the mitral valve repair surgeon to performing rescue surgery, not restorative surgery. Furthermore, there are many findings available on routine echocardiographic studies that can steer the physician and surgeon to appropriately time the proper interventions in these patients with degenerative MR.
Even more problematic, due to conflicting data from numerous studies, is intervention in the “asymptomatic” patient with severe degenerative MR. Bonow, in an outstanding recent publication (11), provides analysis of those studies that have looked at the question of the natural history of asymptomatic patients with severe degenerative MR and sheds light on the question of “watchful waiting”. Kang et al. (12) clearly showed that asymptomatic patients with severe degenerative MR who underwent excellent repair had dramatic survival advantages (normal lifespan) and improved quality of life compared to those that were treated conservatively. Similar conclusions have been noted by David et al. (7) in their sentinel work spanning over 20 years of mitral valve repair in a single institution by a world-recognized master surgeon. In their recent publication, David et al. concluded, “Mitral valve repair for degenerative MR restored the lifespan to normal, with the exception of patients who had advanced symptomatology and impaired left ventricular function. These findings support the recommendation of early mitral valve repair in patients with severe MR and normal ventricular function, regardless of their symptomatic status…” (7). While both Bonow (11) and David (7) point out that there is little in the way of prospective randomized trials to assess proper management of these asymptomatic patients with severe degenerative MR, retrospective analysis clearly suggests that outstanding mitral valve repair (not replacement) before the development of clinical or subclinical left ventricular dysfunction, atrial fibrillation or pulmonary hypertension improves survival and decreases morbidity.
It is an established fact that mitral valve repair for primary degenerative MR is preferable to mitral valve replacement if that reparative surgery is performed by an experienced surgeon, in an experienced center that has a commitment to developing outstanding long-term outcomes for their patients. Gammie et al. (13,14), Bolling et al. (15), and Kilic et al. (16) have all highlighted the importance of having experienced, high-volume surgeons at high-volume centers perform mitral valve reparative procedures, as these centers are dedicated to assessing their quality and outcomes over the lifespan of the patient. Adams et al. (5) have argued for the concept of Reference Centers for mitral valve repair surgery, as those centers will offer patients the best long-term outcomes and, hopefully, freedom from recurrent MR. David (7), in his recent publication, points out that long-term freedom from recurrent severe MR occurs in over 90% of the patients who have undergone operative repair. This statistic is very significant, because many of the patients included in this study were followed from as long ago as 1985. David (7) does go on to point out that the particular anatomic lesion (anterior leaflet prolapse etc.) and surgical technique (lack of annuloplasty ring etc.) can be independent predictors of recurrent postoperative MR. Thus, he argues that with complicated cases, repair should be undertaken by very experienced surgeons operating in high-volume centers, giving support to Adams’ concept of reference centers for mitral valve repair surgery.
Current guidelines (9,10) offer expert opinion as to when considerations for operative repair should be undertaken. However from an “outside the box” perspective, the critical question is not what the clinician or surgeon thinks of the severity of the degenerative MR, but really what the heart thinks of this severity. In other words, how is the MR affecting all components of cardiac anatomy and function?
This question can be answered by echocardiographic techniques available today. By using these diagnostic techniques, the clinician and surgeon can put together six key factors that will steer them toward making the proper decision regarding timing for surgical intervention in any given patient. These key factors are: (I) Valvular (mitral apparatus) anatomy—etiology and lesion; (II) Severity of the MR (quantitative); (III) Left ventricular chamber size and function; (IV) Left atrial chamber size; (V) Resting RV–pulmonary artery (PA) pressures; and (VI) Response of the left ventricle, as well as the pulmonary pressures, to Exercise Stress Testing (Table 2). TTE plays the major role in evaluating severity of MR, left ventricular and right ventricular size and function, left atrial size, and resting-exercise evaluation of RV pressures. A well-performed TTE gives tremendous information about mitral valve anatomy. However, TEE, especially 3D-TEE, is extremely valuable due to its surgical anatomic views of the mitral valve as it can assess the exact anatomic lesions present and help the surgeon to evaluate the effectiveness of proper mitral valve surgery.
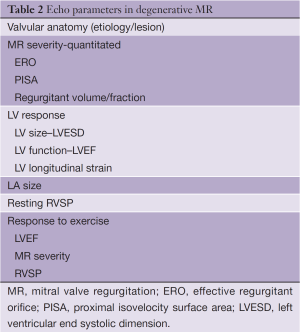
Full table
Determination of valvular anatomy (etiology and lesion)
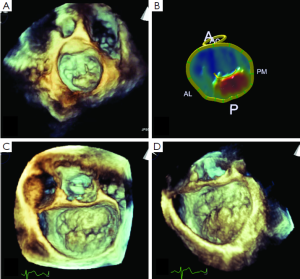
In the hands of experienced echocardiographers, TTE (2D and 3D) can often provide specific anatomic-pathologic diagnosis for the mitral valve. However, TEE, especially 3-D TEE with its enhanced “surgical” views (Figure 1), is also of great value in determining whether the anatomy represents purely fibroelastic deficiency, Barlow’s Disease, or some forme fruste thereof, as highlighted by Adams et al. (5). Knowing this exact anatomy is critical, as it not only aids the clinician and surgeons in preoperative evaluation, but may also dictate whether patients who have very complex anatomy might warrant operative repair at a high-volume Reference Center.
Severity of MR
Historically, Doppler echo grading of MR severity has been done subjectively by eye. This semi-qualitative assessment of MR is not appropriate, as it is dramatically influenced by the quality of the study, the experience of the interpreter, and the blood pressure during the study (blood pressure must be taken into account and clearly listed on each echocardiographic study). These factors drastically affect not only the qualitative grading of MR, but also the reproducibility of these findings on follow-up exams. The bottom line is that qualitative assessment of MR is no longer appropriate and should not be done. Quantitative assessment of MR [calculation of ERO, Proximal Isovelocity Surface Area (PISA), regurgitant volume and fractions] should be routinely performed and can be done with fair reproducibility with the current equipment available today. New developments in 3D-TEE instrumentation have allowed for real-time quantitative assessment of MR with volumetric flow data giving measurements that are similar in accuracy to those obtained by MRI (17).
Left ventricular size and function
Both the ACC/AHA guidelines (9) and the newly-revised European guidelines (10) highlight the importance of both left ventricular function (LVEF) and left ventricular size in decision making for the management of patients with degenerative MR. It is well known that preoperative LVEF in patients with valvular degenerative MR predicts postoperative LVEF, as well as long-term symptom-free survival. Sarano et al. (18) showed that patients with preoperative LVEF of <50% had a markedly worse symptom-free survival compared to those patients who had ejection fractions of ≥60%. Current guidelines suggest that LVEF of ≤60% is a sign of abnormal LV function and, therefore, a Class I indication for surgery. However, a LVEF in the setting of severe degenerative MR should be much higher than this, since the left ventricle is unloading into the lower pressure LA. Recent work by David et al. (7) in assessing the late outcomes of their sizeable number of patients who underwent mitral valve repair, highlight that even mild preoperative left ventricular dysfunction increases the risk for late cardiac mortality. Hence, by waiting for signs of mild left ventricular dysfunction before offering mitral valve repair to asymptomatic patients, we as clinicians, are doing a disservice to these patients. Recent work by Suri et al. (19) at the Mayo Clinic showed that nearly a quarter of their patients who were being evaluated for surgical intervention developed left ventricular dysfunction during that follow-up, even if they had had less than severe MR at initial evaluation.
The accurate evaluation of left ventricular function is critical. Unfortunately, left ventricular function analysis, primarily through LVEF, has been performed subjectively and qualitatively by most echocardiographic laboratories. As with qualitative assessment of the severity of MR, this is no longer acceptable. Echocardiographic labs should offer quantitative assessment of global LVEF, either by Biplane Simpson calculation, or by currently real-time 3D volumetric TTE analysis, which will allow for accurate quantification of ejection fractions.
Many argue that LVEF is a poor surrogate for left ventricular health. New data points out that global longitudinal strain, measured by tissue Doppler on standard echocardiographic equipment, carries incremental value in assessing the health of the underlying myocardium, especially in VHD. Changes in global longitudinal strain appear to be able to detect subclinical and subtle abnormalities in global and regional left ventricular function not currently provided by standard measurements of LVEF. Work by Pandis et al. (20) has shown that abnormalities of pre-operative longitudinal strain (>-25), even in the setting of normal LVEF, may highlight ventricles that have already sustained cellular damage such that even with successful repair, their post-operative ejection fractions may be markedly diminished. Hence, assessment of longitudinal myocardial mechanics in patients with degenerative MR should be routinely measured, especially in those who are considered asymptomatic and with “normal” LVEF. This data may offer better evaluation of not only left ventricular health, but also proper timing for surgical intervention.
Left ventricular end systolic dimension (LVESD) is another important determinant of overall left ventricular health in the setting of severe MR. Work by Tribouilloy et al. (21) has shown the important ability of preoperative LVESD to predict post-operative survival. In their work, patients with LVESD of >40 mm had marked reduction in long-term survival compared to those with preoperative LVESD of <40 mmHg. Follow-up work by the same authors (22) showed the power of combining LVESD and LVEF to offer the best prognosis for post-operative LV function in patients who are undergoing mitral valve repair. Their data clearly suggest that a LVEF of >64% and a LVESD of <37 mm are the best predictors for good postoperative LV function–implying outcome. Their data suggest that one should not wait for ejection fractions to fall to <64% and/or for ventricles to enlarge to >37 mm at end systole.
Left atrial size
Enlargement of the left atrium (LA), due to longstanding severe MR, can lead to atrial fibrillation, which negates some of the beneficial effects of appropriately timed mitral valve repair. Recent work by Le Tourneau et al. (23) suggested that left atrial volume index (LAVI) of >60 mL/m2 denotes individuals with a dramatically lower 5-year survival than those with no or mild LA enlargement, especially if the patients are managed medically. Allowing a patient to develop atrial fibrillation prior to surgical intervention is associated with increased morbidity and potentially mortality. Data clearly show that indexing LA volume to body size is predictive of long-term outcomes in the setting of severe degenerative MR. LAVI of > 40 mL/m2 increases the risk of atrial fibrillation. As pointed out by Le Tourneau et al. (23), allowing the LAVI to approach 60 mL/m2 will denote a population whose 5-year survival might be a dismal 53%. Hence, quantification of LAVI is important as it appears that moderate to possibly even mild enlargement of LA carries a negative long-term prognosis. Thus, assessment of LA size and LAVI is one of the six triggers for considering proper timing for operative intervention.
RV systolic pressure
Significant degenerative MR can adversely affect pulmonary vasculature, RV function, and even tricuspid annular size. TTE, with standard Doppler, is the technique of choice for non-invasively determined right ventricular systolic pressure (RVSP) from tricuspid regurgitant (TR) jet velocity. RVSP assessment, both at rest and with exercise, is critical in the evaluation of patients with severe degenerative MR, especially those deemed asymptomatic. Work by Ghoreishi et al. (24) has shown that pre-operative pulmonary hypertension is a strong predictor of both early and late mortality after mitral valve repair. These authors found that even modest elevation of resting RVSP predicts less than ideal short-term (hospital) and long-term survival. Current guidelines suggest that new onset atrial fibrillation, or pulmonary hypertension at rest, are Class IIa indications for mitral valve repair. Ghoreishi et al. (24) showed that pre-operative RVSP of ≥40 mmHg leads to a dramatic decrease in actuarial survival. So while it is unresolved what value of resting RVSP is acceptable to allow one to “follow” a given patient, having an elevated resting RVSP (>40 mmHg) may suggest that the clinician needs to further evaluate the effects of the degenerative MR on right-sided pressures by way of Exercise Stress Testing.
Stress echocardiography
Patients with severe degenerative MR may state they are asymptomatic, but may be denying the presence of symptoms or have gradually cut back on their level of physical exertion and are now not very active at all. Exercise Stress Echo is becoming increasingly important to determine whether, in fact, patients are symptomatic, as it offers excellent prognostic information as to appropriate timing for operative repair in degenerative MR. While some use oxygen consumption with exercise testing, simple Exercise Treadmill Stress Testing or Bike Testing coupled with echocardiography can evaluate not only the functional capacity of the patient, but also the presence or absence of appropriate rise in LVEF and, importantly, the effect of exercise on RVSP.
Picano et al. (25) highlighted the important role that Exercise Stress Testing and Stress Echo play in VHD, especially in evaluating asymptomatic patients with severe MR. Magne et al. (26) clearly showed that exercise-induced pulmonary hypertension (RVSP of ≥56 mmHg) in asymptomatic patients with severe degenerative MR is a strong predictor of less than ideal 2-year symptom-free survival. In fact, patients in their series who developed exercise-induced pulmonary hypertension had a marked reduction in symptom-free survival.
The development of elevated RVSP with exercise, even in those whose baseline RV systolic pressures may be “normal”, may represent a group of “asymptomatic patients” who are not truly asymptomatic and could possibly benefit from considerations for surgical repair.
Summary
Recently, Suri et al. (27) presented data on over 2,000 patients in whom a simple TTE diagnosed the appearance of a flail mitral leaflet. These authors found that those patients with a flail mitral leaflet who were managed surgically had marked improvement in long-term survival rates compared to a propensity-matched cohort who were managed medically. While there are multiple comments that could be made about this study (86% had isolated P2 prolapse and the surgical cohort had a trend toward larger ventricles, larger LAs, etc.), these authors do make the case that early operative intervention gives patients with a flail leaflet a better long-term prognosis.
However, this author contends that using the six factors (Table 3) readily available today from standard echocardiography allows the clinician/surgeon to appropriately time interventions for surgery in patients with degenerative MR, especially those who are considered asymptomatic.
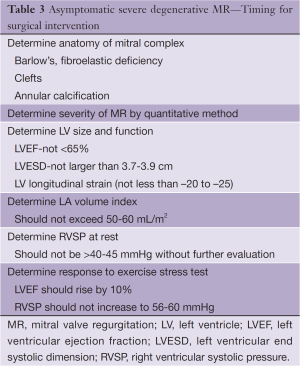
Full table
Illustrative case
A fifty-two-year-old female accountant with a history of systolic murmur described to be louder on the latest physical exam. Resting echo showed:
- Flail P2-P3 with severe anteriorly directed jet of MR-ERO 38 mm2;
- LVEF 65-70%;
- LV end diastolic/end systolic dimension 5.1/2.8 cm;
- Resting RVSP of 40 mmHg;
- LA volume index 52 mL/m2.
The patient stated that she was asymptomatic, but due to left atrial size and RV pressures, Exercise Stress Test was performed. The patient was able to exercise eight minutes, reaching the 3rd Stage of the Bruce Test, at a workload of 9 METS, with test stopped, due to marked dyspnea. The patient achieved a peak heart rate of 162 (96% of age-predicted max). No ischemic symptoms or EKG signs were noted.
Immediate post-exercise echo showed:
- Normal rise in EF to 80-85;
- Severe MR remained;
- RV systolic pressures rose to 68-75 mmHg.
Disposition
The patient was felt to be markedly symptomatic with exercise, and because she had left atrial enlargement and showed significant elevation of right-sided pressures with exercise, mitral valve repair was deemed appropriate. The patient underwent successful mitral valve repair and tricuspid annuloplasty and is doing well.
The future of echocardiographic imaging as it relates to mitral valve repair
Dramatic developments are occurring with real-time modeling of 3D-TEE images (28) to create outstanding images of the entire mitral apparatus, annulus, aortic mitral curtain and aortic annulus. These images can and will be utilized by surgeons to preoperatively plan the appropriate intervention and sizing of devices, such as the annuloplasty ring (Figure 2). Similarly, these models may be utilized to create simulation techniques, which will hopefully allow for much better operative outcomes. Additionally, recent work by Rim et al. (29) shows that by using 3D-TEE to obtain volumetric morphology of the mitral valve apparatus, additional computational simulation techniques can provide virtual mitral valve models that demonstrate deformation and stress distribution on the mitral valve structure across the cardiac cycle. These authors point out that being able to assess stress distribution on the mitral leaflets, even in patients who do not currently demonstrate severe MR, may allow identification of patients who are most likely to develop pathophysiologic alterations in the mitral valve structure. Thus, we will be able to predict in these patients who may be more likely to develop potential chordal ruptures or annular dilatations. The ability to determine the exact location of stress distribution on pathologic mitral valve leaflets should provide the surgeon with a roadmap to better plan operative intervention, one that might prevent technical failures in the future.

Acknowledgements
The author (Randolph P. Martin) serves on the Speaking Bureaus of Medtronic, Inc., Edwards Lifesciences LLC, and Sorin Group U.S.A. Inc and receives research grant funding from Siemens Ultrasound.
Disclosure: The author declares no conflict of interest.
References
- d’Arcy JL, Prendergast BD, Chambers JB, et al. Valvular heart disease: the next cardiac epidemic. Heart 2011;97:91-3. [PubMed]
- Enriquez-Sarano M, Avierinos JF, Messika-Zeitoun D, et al. Quantitative determinants of the outcome of asymptomatic mitral regurgitation. N Engl J Med 2005;352:875-83. [PubMed]
- BARLOW JB, POCOCK WA. The significance of late systolic murmurs and mid-late systolic clicks. Md State Med J 1963;12:76-7. [PubMed]
- Carpentier A, Lacour-Gayet F, Camilleri J. Fibroelastic dysplasia of the mitral valve: an anatomic and clinical entity. Circ 1982;3:307.
- Adams DH, Rosenhek R, Falk V. Degenerative mitral valve regurgitation: best practice revolution. Eur Heart J 2010;31:1958-66. [PubMed]
- Carpentier A, Adams D, Fisoufi F. eds. Carpentier’s reconstructive valve surgery: from valve analysis to valve reconstruction. New York: W.B. Saunders, 2010.
- David TE, Armstrong S, McCrindle BW, et al. Late outcomes of mitral valve repair for mitral regurgitation due to degenerative disease. Circulation 2013;127:1485-92. [PubMed]
- Bach DS, Awais M, Gurm HS, et al. Failure of guideline adherence for intervention in patients with severe mitral regurgitation. J Am Coll Cardiol 2009;54:860-5. [PubMed]
- Bonow RO, Carabello BA, Chatterjee K, et al. 2008 focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1998 guidelines for the management of patients with valvular heart disease). Endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol 2008;52:e1-142. [PubMed]
- Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC), European Association for Cardio-Thoracic Surgery (EACTS), Vahanian A, et al. Guidelines on the management of valvular heart disease (version 2012). Eur Heart J 2012;33:2451-96. [PubMed]
- Bonow RO. Chronic mitral regurgitation and aortic regurgitation: have indications for surgery changed? J Am Coll Cardiol 2013;61:693-701. [PubMed]
- Kang DH, Kim JH, Rim JH, et al. Comparison of early surgery versus conventional treatment in asymptomatic severe mitral regurgitation. Circulation 2009;119:797-804. [PubMed]
- Gammie JS, O’Brien SM, Griffith BP, et al. Influence of hospital procedural volume on care process and mortality for patients undergoing elective surgery for mitral regurgitation. Circulation 2007;115:881-7. [PubMed]
- Gammie JS, Sheng S, Griffith BP, et al. Trends in mitral valve surgery in the United States: results from the Society of Thoracic Surgeons Adult Cardiac Surgery Database. Ann Thorac Surg 2009;87:1431-7; discussion 1437-9. [PubMed]
- Bolling SF, Li S, O’Brien SM, et al. Predictors of mitral valve repair: clinical and surgeon factors. Ann Thorac Surg 2010;90:1904-11; discussion 1912.
- Kilic A, Shah AS, Conte JV, et al. Operative outcomes in mitral valve surgery: Combined effect of surgeon and hospital volume in a population-based analysis. J Thorac Cardiovasc Surg 2013;146:638-46. [PubMed]
- Thavendiranathan P, Phelan D, Thomas JD, et al. Quantitative assessment of mitral regurgitation: validation of new methods. J Am Coll Cardiol 2012;60:1470-83. [PubMed]
- Enriquez-Sarano M, Schaff HV, Orszulak TA, et al. Valve repair improves the outcome of surgery for mitral regurgitation. A multivariate analysis. Circulation 1995;91:1022-8. [PubMed]
- Suri RM, Aviernos JF, Dearani JA, et al. Management of less-than-severe mitral regurgitation: should guidelines recommend earlier surgical intervention? Eur J Cardiothorac Surg 2011;40:496-502. [PubMed]
- Pandis D, Sengupta PP, Castillo J, et al. Assessment of longitudinal myocardial mechanics in patients with degenerative mitral valve regurgitation predicts post-operative deterioration of left ventricular function. J Am Soc Echocardiogr 2012;25:B43.
- Tribouilloy C, Grigioni F, Avierinos JF, et al. Survival implication of left ventricular end-systolic diameter in mitral regurgitation due to flail leaflets a long-term follow-up multicenter study. J Am Coll Cardiol 2009;54:1961-8. [PubMed]
- Tribouilloy C, Rusinaru D, Szymanski C, et al. Predicting left ventricular dysfunction after valve repair for mitral regurgitation due to leaflet prolapse: additive value of left ventricular end-systolic dimension to ejection fraction. Eur J Echocardiogr 2011;12:702-10. [PubMed]
- Le Tourneau T, Messika-Zeitoun D, Russo A, et al. Impact of left atrial volume on clinical outcome in organic mitral regurgitation. J Am Coll Cardiol 2010;56:570-8. [PubMed]
- Ghoreishi M, Evans CF, DeFilippi CR, et al. Pulmonary hypertension adversely affects short- and long-term survival after mitral valve operation for mitral regurgitation: implications for timing of surgery. J Thorac Cardiovasc Surg 2011;142:1439-52. [PubMed]
- Picano E, Pibarot P, Lancellotti P, et al. The emerging role of exercise testing and stress echocardiography in valvular heart disease. J Am Coll Cardiol 2009;54:2251-60. [PubMed]
- Magne J, Lancellotti P, Piérard LA. Exercise pulmonary hypertension in asymptomatic degenerative mitral regurgitation. Circulation 2010;122:33-41. [PubMed]
- Suri RM, Vanoverschelde JL, Grigioni F, et al. Association between early surgical intervention vs watchful waiting and outcomes for mitral regurgitation due to flail mitral valve leaflets. JAMA 2013;310:609-16. [PubMed]
- Ionasec RI, Voigt I, Georgescu B, et al. Patient-specific modeling and quantification of the aortic and mitral valves from 4-D cardiac CT and TEE. IEEE Trans Med Imaging 2010;29:1636-51. [PubMed]
- Rim Y, Laing ST, Kee P, et al. Evaluation of mitral valve dynamics. JACC Cardiovasc Imaging 2013;6:263-8. [PubMed]





