New concepts for mitral valve imaging
Introduction
Profound anatomical and pathophysiological knowledge of the mitral valve (MV) and adjacent cardiac structures are essential for selecting the most appropriate surgical techniques in MV disease, especially with regards to modern minimally-invasive MV surgery and transcatheter approaches (1-4). Imaging is the key to assessing details of MV disease and to studying the lesions and dysfunction of MV according to Carpentier (5).
Imaging enables assessment of MV function, especially morphological and dynamic basics throughout the cardiac cycle, with particular consideration of the respective pathology (6). Thus, imaging is essential for decision-making and treatment planning.
While multiple modalities exist to assess MV, transthoracic echocardiography (TTE) represents the standard technique to study MV disease (6). Especially with current advances of 3-dimensional (3D) echocardiography in combination with multi-detector row computed tomography (MDCT) and cardiac magnetic resonance (CMR), improved characterization and quantification of the MV apparatus and its functional complexity has improved significantly (7-9). Most recently, geometrical and biomechanical models for analysis of MV are undergoing very early clinical evaluation (10-13).
This perspective article reports on several new concepts of MV modeling specified for MV evaluation and treatment planning.
MV anatomy and physiology
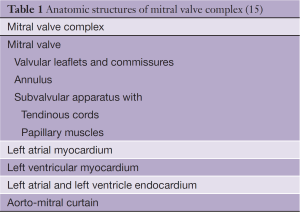
Imaging of the MV apparatus requires a detailed understanding of the anatomy and physiology (14). This is of utmost importance for clinical evaluation and subsequent surgical and/or interventional treatment. Numerous clinical and anatomical data have been collected thus far describing the MV as a complex of several adjacent structures which collectively constitute the MV complex (Table 1) (15,16). The normal function of the MV depends on the coordinated action of several interrelated anatomical elements: the left atrium (LA), the anterior and posterior leaflets, the annulus, the chordae tendineae, the papillary muscles and the left ventricular wall (15). It is of note that each of those components is important, as any alteration or lesion may cause MV dysfunction (stenosis, regurgitation) (6). Structural MV abnormalities are referred to as organic or structural MV disease. Dysfunction of the MV, which evolves secondarily to left ventricular dilatation, is referred to as functional MV disease (6). For the assessment of MV, morphological and functional indices have been established.
With regards to the complexity of MV, it is generally accepted that the physiology and pathophysiology of the MV apparatus, defined as a nonlinear system of fluid-structure interaction (FSI), are at present not fully understood (17).
Computational MV models
Computational models are defined as mathematical models in computational science that require computer simulation and thus computational resources to study the functionality of any complex system. Study objects are complex nonlinear systems for which simple and intuitive analytic solutions are not readily available. Rather than deriving a mathematical analytical solution from a given problem, experimentation with computational models is done by adjusting the parameters of the system in a stepwise fashion in order to achieve a definite approximation.
A scientific model seeks to represent a physical process in a logical and objective manner. Therefore, the process of generating a model is primarily based on key factors influencing a defined physical process. In models, real physical processes are abstracted, reduced or aggregated. Models are typically used when it is either impossible or impractical to create experimental conditions in which scientists can directly measure outcomes.
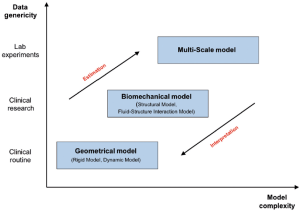
The creation of computer models in cardiovascular medicine requires close collaboration between physicians, computer scientists and engineers. In cardiovascular medicine, one can distinguish between different types of computational models such as geometric models, biomechanical models and multi-scale generic models. All models are based on the actual anatomic structure and are developed to fulfil very special requirements (Figure 1). It is important to acknowledge that increasing complexity increases the calculation time of the model. The most commonly used models in cardiovascular medicine are geometrical models and biomechanical models. Past studies have shown that these models are suitable for the description of complex morphological and biomechanical changes of the heart and great vessels. Computational models were used for accurate analysis of left and right ventricular contraction, flow simulation through artificial heart valves or shear stress analysis of the aorta with aortic aneurysms (17-22).
Exact modeling of MV function has not been realized in the past due to the lack of imaging techniques that enable detection of the 3D structures and their respective function. With the development of real-time 3D echocardiography (RT3DE) and 4-dimensional computed tomography (4DCT), however, the technical capabilities have been introduced to create substantial and well-defined MV models with a high probability for implementation into clinical practice (11).
Geometrical MV models
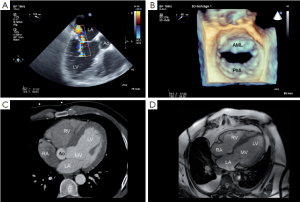
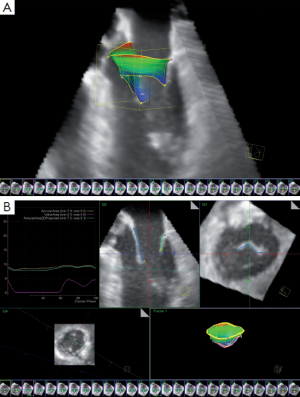
Substantial progress in surgical and percutaneous treatment of structural MV disease has reinforced the interest in non-invasive quantitative analysis of MV morphology and function. Precise morphological and functional knowledge about the MV is a prerequisite during the entire clinical workflow, including diagnosis and therapy planning (11). Currently, most non-invasive MV imaging techniques are based on 2D methodology, such as echocardiography or CT (Figure 2). Due to the complexity and dynamics of MV, accurate geometrical analysis of MV from 2D data sets using echocardiography or CT is difficult. With the introduction and increasing use of RT3DE and 4DCT, it is possible to detect comprehensive structural and dynamic information, including quantification of the MV throughout the cardiac cycle (23,24). Furthermore, with the introduction of imaging-based computational MV models, improved quantification and characterization of the MV has been realized (12,13).
The main objectives of MV modeling are (11):
- Robust conversion of imaging data sets into a virtual model which results in physiological modeling;
- Patient-specific assessment;
- Model-based quantification and visualization.
In addition, this provides an opportunity for interactive manipulation, including rotation, translation, adjustment, zoom, rendering, 2D and 3D measurements.
Rigid MV models
Rigid models are basically only static reconstructions of the MV, the principles of which have been described before (12,13). This technology is generally described as segmentation: after importing a 3D data-set, detection of major anatomic landmarks is conducted with subsequent surface modeling using a geometric mesh. Morphological quantification of MV can be computed according to the final model.
The two most commonly used software systems for MV analysis are the Mitral Valve Quantification (MVQ) program (Philips Healtcare, Inc., Andover, MA, USA) and the 4D MV assessment software (TomTec Imaging Systems GmbH, Munich, Germany) (12,13,23,25). The clinical impact of MV models is still being evaluated but their contribution to the description of MV physiology and pathophysiology is thus far undisputed (23). Rigid models have mainly been used to study dimensions of the mitral annulus in ischemic, non-ischemic and myxomatous MV disease (17,26,27). Of particular interest has been the mitral annulus after MV repair and the influence of aortic valve replacement on the mitral annulus geometry (27,28). Unfortunately, existing rigid models are limited due to static measurements at a predefined phase of the cardiac cycle, which are being performed by manual segmentation, thus preventing further development (12,13,25).
Dynamic MV models
It is widely accepted that the MV is a highly complex dynamic structure, which is directly related to hemodynamic changes subsequent to muscle contraction of the left ventricle throughout the cardiac cycle (29). Using dynamic MV models, the morphology and dynamics of MV can be reconstructed from 4D data sets, such as full volume RT3DE data, over the entire cardiac cycle. Considering the complexity of MV, the necessary estimation procedure of dynamic MV models can be divided into two tasks (11):
- Object delineation;
- Motion estimation.
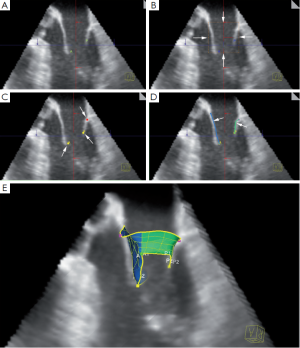
In the dynamic MV model presented herein (AutoValve Beta 10.0, Siemens Corporate Research, Princeton, USA), the modeling is hierarchically defined on three abstraction levels (11):
- Estimation of a global location of MV within a given imaging data set and segmentation of a rigid landmark motion model;
- Estimation of a non-rigid landmark motion model;
- Estimation of a mitral comprehensive model.
This method of MV dynamic modeling applying this algorithm has been described before (Figure 3) (10,11). With this model, different quantitative MV parameters, including annular circumference, leaflet area and mitral orifice area, are continuously depicted over the entire cardiac cycle (Table 2). It is important to note that the quantification potential of the proposed method is not limited. Through the consistent and comprehensive spatial and temporal representation, the introduced system offers unique analytic features, which facilitate decisions during the whole clinical workflow.
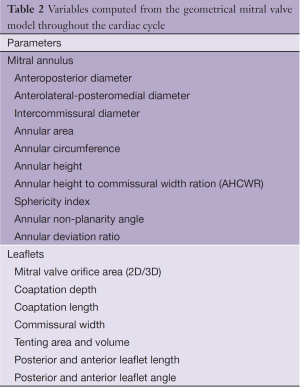
Full table
Currently, echocardiographic-based dynamic MV models are in the phase of early clinical validation. It can be expected that in the near future, dynamic MV models will significantly improve the assessment of the MV and therefore may substantially contribute to the understanding of the MV complex.
Model-based quantification of MV
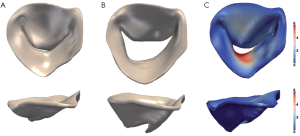
Different specific data on morphological and functional parameters of the MV complex can be derived from MV models (Figure 4). Although not clinically implemented, several benefits of such a model are (11):
- Increased level of precision, especially when studying native three-dimensional valve anatomy;
- High reproducibility due to automatic quantification;
- User independence;
- Functional assessment throughout the cardiac cycle;
- Comprehensive analysis, including complex morphology such as curvatures, deformation fields and volumetric variations.
Comprehensive valve measurements are important in regards to clinical workflow among cardiac surgeons, especially for treatment planning in percutaneous and minimally-invasive valve interventions, which require extensive non-invasive assessment. Thus MV modeling is likely to contribute most significantly to assessing the type of MV repair, the level of MV disease complexity, and improving decision-making.
Biomechanical MV models
Biomechanical and fluid dynamic analysis of the MV complex is a prerequisite in understanding MV function. While geometrical models focus on morphological and dynamic quantification of MV, biomechanical models aim to simulate the biomechanics of MV (structural models) to allow for examination and analysis of the MV structure with blood flow (FSI models). It is therefore a basic necessity to accurately assess MV and left ventricle geometry as depicted in the respective geometric models. Furthermore, biomechanical models are particularly challenging with regards to numerical algorithms that represent MV complexity as well as computational resources. Pioneering work has been presented by Kunzelmann et al. in which newly proposed models allow for detailed insights on MV function (30-32). Two categories of biomechanical MV models can be distinguished: structural models and FSI models. Previous studies have shown that structural models are more reliable for simulation of static events, but in order to accurately simulate full dynamic behaviour, FSI models are required (33).
Structural MV models
Structural models aim to simulate the biomechanics of MV without directly taking into account the blood flow (34). The most widely used model type for cardiac structures is the finite element method (FEM), a numerical approximation technique for boundary value problems. The mathematical algorithm involves accurate geometry, surface pressure and boundary conditions such as material properties and other aspects of the MV apparatus. Using FEM, shear stress of the leaflets or annulus, deformation of MV geometry throughout the cardiac cycle, or disease progression can be simulated (Figure 5) (31,35). Furthermore, it is possible to simulate—at a preliminary stage—surgical or interventional MV procedures (32,34).
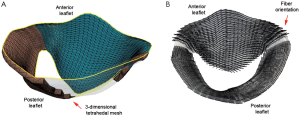
MV leaflets, annulus and chordae have been identified as non-linear tissue with anisotropic linear elasticity (30,34,36). MV biomechanics is mostly modelled using hyper-elasticity theory (37). These methods enable simulation of leaflet and annulus stress distribution during MV motion, as well as annular contraction (37-42). One example of simulation is MV edge-to-edge repair, a prominent repair technique in contemporary MV treatment (34).
Structural models are currently under clinical investigation in selected research projects (Figure 6). With the improvement of technology, integration into a clinical routine can be expected.
Structure-fluid interaction models
Fluid-structure models aim to study the interaction between the MV and the blood flow. In such models, a structural model of the MA (FEM) is combined with a computational fluid dynamic (CFD) model. This allows for analysis of flow and dynamic structures. These models currently represent the most complex modelling type.
Such models analyze the direction of blood flow, blood flow rate, blood flow volume and blood pressure while simultaneously simulating the influence of blood flow on the surrounding structures of the MV. In the last decade, initial algorithms have been established for structure-fluid interaction modelling. Using such technology, a MV specimen can be investigated in a standardized liquid environment such as a tube, box or an idealized left ventricle (33,43). However, any standardized model poorly reflects human anatomy of the LA and left ventricle (44). Nevertheless, FSI models represent thus far the most comprehensive analysis of the MV.
Limitations of computational models
Geometrical models
Geometrical models are mostly based on RT3DE data sets. Accordingly, the limitations of RT3DE also apply for geometrical models. These are R-wave gating and the existence of modeling based on a non-continuous cardiac cycle. Patient-specific modeling is highly time consuming due to visual inspections and manual corrections of landmarks.
Biomechanical models
Structural and FSI models have limitations such as calculating only one level of thickness of the MV leaflets, since they are based on linear calculation algorithms. It also requires costly computational power and time. FSI models are based on non-physiological rigid and static boundaries.
Conclusions
The complex structure and dynamic of MV apparatus throughout the cardiac cycle can be analyzed with different types of computational models. These represent substantial progress in the diagnosis of structural heart disease since MV morphology and dynamics can be studied in unprecedented detail. It is undoubtedly conceivable that MV modeling will contribute to a deeper understanding of the MV.
Acknowledgements
This work has been founded by the University Heart Center Leipzig. The authors thank Razvan I. Ionasec, Ingmar Voigt and Tommaso Mansi for their valuable assistance.
Disclosure: The authors declare no conflict of interest.
References
- Modi P, Hassan A, Chitwood WR Jr. Minimally invasive mitral valve surgery: a systematic review and meta-analysis. Eur J Cardiothorac Surg 2008;34:943-52. [PubMed]
- Cheng DC, Martin J, Lal A, et al. Minimally invasive versus conventional open mitral valve surgery: a meta-analysis and systematic review. Innovations (Phila) 2011;6:84-103. [PubMed]
- Feldman T, Foster E, Glower DD, et al. Percutaneous repair or surgery for mitral regurgitation. N Engl J Med 2011;364:1395-406. [PubMed]
- Seeburger J, Borger MA, Doll N, et al. Comparison of outcomes of minimally invasive mitral valve surgery for posterior, anterior and bileaflet prolapse. Eur J Cardiothorac Surg 2009;36:532-8. [PubMed]
- Carpentier A. Cardiac valve surgery--the “French correction”. J Thorac Cardiovasc Surg 1983;86:323-37. [PubMed]
- Debonnaire P, Palmen M, Marsan NA, et al. Contemporary imaging of normal mitral valve anatomy and function. Curr Opin Cardiol 2012;27:455-64. [PubMed]
- Delgado V, Tops LF, Schuijf JD, et al. Assessment of mitral valve anatomy and geometry with multislice computed tomography. JACC Cardiovasc Imaging 2009;2:556-65. [PubMed]
- Kaplan SR, Bashein G, Sheehan FH, et al. Three-dimensional echocardiographic assessment of annular shape changes in the normal and regurgitant mitral valve. Am Heart J 2000;139:378-87. [PubMed]
- Morris MF, Williamson EE, Topilsky Y, et al. Multi-imaging assessment of the congenital mitral arcade. J Am Coll Cardiol 2011;57:1856. [PubMed]
- Ionasec RI, Voigt I, Georgescu B, et al. Personalized modeling and assessment of the aortic-mitral coupling from 4D TEE and CT. Med Image Comput Comput Assist Interv 2009;12:767-75. [PubMed]
- Ionasec RI, Voigt I, Georgescu B, et al. Patient-specific modeling and quantification of the aortic and mitral valves from 4-D cardiac CT and TEE. IEEE Trans Med Imaging 2010;29:1636-51. [PubMed]
- Jassar AS, Brinster CJ, Vergnat M, et al. Quantitative mitral valve modeling using real-time three-dimensional echocardiography: technique and repeatability. Ann Thorac Surg 2011;91:165-71. [PubMed]
- Mahmood F, Karthik S, Subramaniam B, et al. Intraoperative application of geometric three-dimensional mitral valve assessment package: a feasibility study. J Cardiothorac Vasc Anesth 2008;22:292-8. [PubMed]
- McCarthy KP, Ring L, Rana BS. Anatomy of the mitral valve: understanding the mitral valve complex in mitral regurgitation. Eur J Echocardiogr 2010;11:i3-9. [PubMed]
- Muresian H. The clinical anatomy of the mitral valve. Clin Anat 2009;22:85-98. [PubMed]
- Ho SY. Anatomy of the mitral valve. Heart 2002;88 Suppl 4:iv5-10. [PubMed]
- Grewal J, Suri R, Mankad S, et al. Mitral annular dynamics in myxomatous valve disease: new insights with real-time 3-dimensional echocardiography. Circulation 2010;121:1423-31. [PubMed]
- Calleja A, Thavendiranathan P, Ionasec RI, et al. Automated quantitative 3-dimensional modeling of the aortic valve and root by 3-dimensional transesophageal echocardiography in normals, aortic regurgitation, and aortic stenosis: comparison to computed tomography in normals and clinical implications. Circ Cardiovasc Imaging 2013;6:99-108. [PubMed]
- Chandra S, Salgo IS, Sugeng L, et al. Characterization of degenerative mitral valve disease using morphologic analysis of real-time three-dimensional echocardiographic images: objective insight into complexity and planning of mitral valve repair. Circ Cardiovasc Imaging 2011;4:24-32. [PubMed]
- Mihalef V, Ionasec RI, Sharma P, et al. Patient-specific modelling of whole heart anatomy, dynamics and haemodynamics from four-dimensional cardiac CT images. Interface Focus 2011;1:286-96. [PubMed]
- Dwyer HA, Matthews PB, Azadani A, et al. Computational fluid dynamics simulation of transcatheter aortic valve degeneration. Interact Cardiovasc Thorac Surg 2009;9:301-8. [PubMed]
- Nicosia MA, Cochran RP, Einstein DR, et al. A coupled fluid-structure finite element model of the aortic valve and root. J Heart Valve Dis 2003;12:781-9. [PubMed]
- Andrawes MN, Feinman JW. 3-dimensional echocardiography and its role in preoperative mitral valve evaluation. Cardiol Clin 2013;31:271-85. [PubMed]
- Dal-Bianco JP, Levine RA. Anatomy of the mitral valve apparatus: role of 2D and 3D echocardiography. Cardiol Clin 2013;31:151-64. [PubMed]
- Veronesi F, Corsi C, Sugeng L, et al. A study of functional anatomy of aortic-mitral valve coupling using 3D matrix transesophageal echocardiography. Circ Cardiovasc Imaging 2009;2:24-31. [PubMed]
- Lee AP, Hsiung MC, Salgo IS, et al. Quantitative analysis of mitral valve morphology in mitral valve prolapse with real-time 3-dimensional echocardiography: importance of annular saddle shape in the pathogenesis of mitral regurgitation. Circulation 2013;127:832-41. [PubMed]
- Mahmood F, Subramaniam B, Gorman JH 3rd, et al. Three-dimensional echocardiographic assessment of changes in mitral valve geometry after valve repair. Ann Thorac Surg 2009;88:1838-44. [PubMed]
- Vergnat M, Levack MM, Jackson BM, et al. The effect of surgical and transcatheter aortic valve replacement on mitral annular anatomy. Ann Thorac Surg 2013;95:614-9. [PubMed]
- Silbiger JJ. Anatomy, mechanics, and pathophysiology of the mitral annulus. Am Heart J 2012;164:163-76. [PubMed]
- Kunzelman KS, Cochran RP, Chuong C, et al. Finite element analysis of the mitral valve. J Heart Valve Dis 1993;2:326-40. [PubMed]
- Kunzelman KS, Reimink MS, Cochran RP. Annular dilatation increases stress in the mitral valve and delays coaptation: a finite element computer model. Cardiovasc Surg 1997;5:427-34. [PubMed]
- Kunzelman KS, Reimink MS, Cochran RP. Flexible versus rigid ring annuloplasty for mitral valve annular dilatation: a finite element model. J Heart Valve Dis 1998;7:108-16. [PubMed]
- Lau KD, Diaz V, Scambler P, et al. Mitral valve dynamics in structural and fluid-structure interaction models. Med Eng Phys 2010;32:1057-64. [PubMed]
- Mansi T, Voigt I, Georgescu B, et al. An integrated framework for finite-element modeling of mitral valve biomechanics from medical images: application to MitralClip intervention planning. Med Image Anal 2012;16:1330-46. [PubMed]
- Kunzelman KS, Quick DW, Cochran RP. Altered collagen concentration in mitral valve leaflets: biochemical and finite element analysis. Ann Thorac Surg 1998;66:S198-205. [PubMed]
- Schievano S, Kunzelman K, Nicosia MA, et al. Percutaneous mitral valve dilatation: single balloon versus double balloon. A finite element study. J Heart Valve Dis 2009;18:28-34. [PubMed]
- Prot V, Haaverstad R, Skallerud B. Finite element analysis of the mitral apparatus: annulus shape effect and chordal force distribution. Biomech Model Mechanobiol 2009;8:43-55. [PubMed]
- Krishnamurthy G, Itoh A, Swanson JC, et al. Regional stiffening of the mitral valve anterior leaflet in the beating ovine heart. J Biomech 2009;42:2697-701. [PubMed]
- Prot V, Skallerud B, Sommer G, et al. On modelling and analysis of healthy and pathological human mitral valves: two case studies. J Mech Behav Biomed Mater 2010;3:167-77. [PubMed]
- Skallerud B, Prot V, Nordrum IS. Modeling active muscle contraction in mitral valve leaflets during systole: a first approach. Biomech Model Mechanobiol 2011;10:11-26. [PubMed]
- Stevanella M, Krishnamurthy G, Votta E, et al. Mitral leaflet modeling: Importance of in vivo shape and material properties. J Biomech 2011;44:2229-35. [PubMed]
- Stevanella M, Votta E, Redaelli A. Mitral valve finite element modeling: implications of tissues’ nonlinear response and annular motion. J Biomech Eng 2009;131:121010. [PubMed]
- Ma X, Gao H, Griffith BE, et al. Image-based fluid-structure interaction model of the human mitral valve. Computers&Fluids 2013;71:417-25.
- Voigt I, Mansi T, Mihalef V, et al. Patient-specific model of left heart anatomy, dynamics and hemodynamics from 4D TEE: a first validation study. Proceedings of the 6th international conference on Functional imaging and modeling of the heart. Springer-Verlag Berlin, Heidelberg, 2011:341-9.