Totally thoracoscopic left upper lobe tri-segmentectomy
With continued growing interest in sublobar resections from the international surgical community (1,2), mastering thoracoscopic segmentectomy is an important challenge for the surgeon. With respect to sublobar resections of the left upper lobe, it is now considered that for T1 tumors, a lingual-sparing upper lobectomy is oncologically equivalent to an upper lobectomy (3).
The main segmental resections involving the left upper lobe are: tri-segmentectomy (S1 + S2 + S3) (lingula-sparing lobectomy), apicoposterior segmentectomy (S1 + S2) and lingulectomy (S4 + S5). In this article, we will describe the technique of a full thoracoscopic approach and illustrate it with a video. Lymph node dissection is similar to lymphadenectomy for an upper lobectomy and hence will not be described here.
Clinical summary
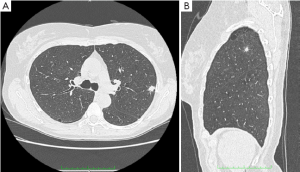
The presenting case is a 66-year-old female patient who had an incidental finding of a nodule during follow-up of a severe chronic obstructive pulmonary bronchitis. The nodule was 1 cm in diameter and was located at the junction between the posterior and apical segments of the left upper lobe (Figure 1). PET-CT revealed an isolated tumor (SUVmax: 2.7). As the patient was fragile and had a FEV1 of 61% predicted, it was decided to perform a sublobar resection.
Anatomical landmarks
The landmarks are obtained from CT-scans with 3-dimensional reconstruction (Figure 2). The use of CT reconstruction can be helpful at the beginning of a thoracoscopic experience (4,5).

Bronchi
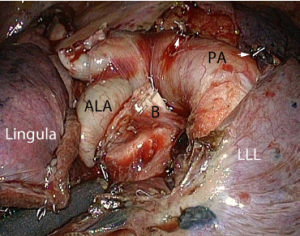
The segmental bronchi are concealed by arteries which must be divided first (Figure 2A). The upper lobe bronchus splits immediately into the lingular bronchus and a common stem which separates into an anterior bronchus and an apicoposterior bronchus. These segmental bronchi have short courses which can make their dissection and identification difficult.
Arteries
The truncus anterior, posterior and lingular arteries supply the left upper lobe (Figure 2B). The truncus anterior is often broad and short and supplies the apico-posterior and anterior segments. The posterior segmental arteries originate in the fissure and distribute themselves over the curve of the pulmonary artery. Their number varies from 1 to 5, but most often from 2 to 3. All but the lingular artery, must be divided.
Veins
The superior pulmonary vein usually has three major tributaries (Figure 2C). The superior branch drains the apicoposterior segments and frequently blocks access to the apicoposterior arteries. The middle branch drains the anterior segment and the lowermost branch drains the lingula. The latter must be preserved.
Technique
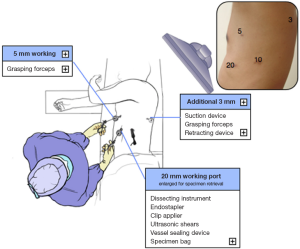
The procedure is performed under general anesthesia with split ventilation using a double-lumen endotracheal tube. Patients are positioned in the right lateral decubitus position. We use a deflectable scope housing a distal CCD (LTF, Olympus, Tokyo, Japan) connected to a high definition camera system (HDTV) (Exera II, Olympus, Tokyo, Japan). Only endoscopic instruments are used. These are inserted through 3 to 4 trocars, depending on whether an additional lymph node dissection is performed. Ports are inserted as indicated in Figure 3.
The procedure is similar to a left upper lobectomy, sparing the lingular vessels and the anterior portion of the fissure.
Step 1: division of the fissure and arteries
The lobes are separated to expose the middle portion of the fissure. The upper lobe is gently pulled forward, avoiding any undue traction which could injure the vessels. Dissection is conducted cephalad and all encountered posterior arteries are divided by turn. Traction helps exposing the first segmental artery whose dissection is usually easy. It is controlled by clipping, with a vessel sealing device or with a combination of both.
As the posterior segmental arteries are sequentially divided, the upper lobe unfolds and uncovers the posterior aspect of the truncus anterior which can be approached posteriorly. It is then also dissected from above and from the front, using various views thanks to the deflectable scope. Gentle blunt dissection is used to clear the origin of the trunk. If the trunk bifurcates into two large branches, these are dissected with caution and stapled independently.
An inferior branch of the truncus anterior is present in one-quarter of patients (Figure 4). It is usually impossible to predict whether this branch supplies the anterior segment or the lingula or both. When in doubt, it is advisable to preserve it.
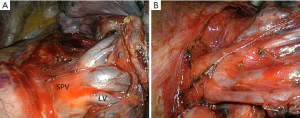
Step 2: division of the segmental veins
The upper lobe is retracted posteriorly. The mediastinal pleura is then incised posterior to the phrenic nerve. Dissection of the vein is achieved by a combination of blunt dissection and bipolar electrocautery. Only the two superior branches are divided using either a stapler, or clips or a vessel sealing device, depending on their diameter. The inferior tributary which drains the lingula is preserved (Figure 5).
Step 3: division of the bronchial trunk and parenchyma
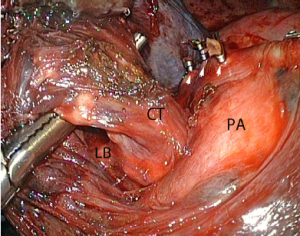
Once the arteries and veins have been divided, traction on the parenchyma helps to expose the segmental bronchi. The origin of the lingular bronchus is visualized and the upper trunk—which separates into an anterior bronchus and an apico-posterior bronchus—is exposed, cleared using a blunt tip dissector and stapled as a stem (Figure 6).
The parenchyma must be stapled between the lingula and the upper division. A clamp is applied on the parenchyma, the lung is reventilated to identify the intersegmental plane and the parenchymal division is then performed using an endostapler loaded with thick-tissue staples.
The specimen is removed in the usual fashion and the inferior pulmonary ligament is divided.
Comments
A left trisegmentectomy is similar in conduct to a right upper lobectomy. However, control of the truncus anterior may be more difficult on the left side because there are more anatomical variations and because the artery can be short.
Possible risks of the procedure are as follows:
- Inadvertent injury of the lingular vein when the distribution of the superior pulmonary vein comprises multiple small branches, as shown in Figure 5B;
- Twisting of the lingular segments when the anterior part of the fissure is loose. If in doubt, the lingula must be anchored to the lower lobe;
- Confusion between the anterior bronchus (B3) of the common trunk and the lingular bronchus;
- Ignorance of an accessory lingular artery that could be mistaken for a branch of the truncus anterior (Figure 4).
Some authors advocate against using stapling for division of the parenchyma because this can impair the expansion of the lingular segments (6). As shown in the video, this has not been an issue in our practice. Although stapling can slightly reduce the volume of the lingula, it has the major advantage of minimizing postoperative air leaks. In our series of 129 thoracoscopic segmentectomies, with stapling of the intersegmental plane, the mean postoperative stay was 4.9 days and only one patient had a prolonged air-leak. Miyasaka et al. failed to demonstrate a difference in postoperative complications and pulmonary function, between stapling of the intersegmental plane and division with electrocautery (7).
Acknowledgements
Disclosure: The author declares no conflict of interest.
References
- Yamashita S, Tokuishi K, Anami K, et al. Thoracoscopic segmentectomy for T1 classification of non-small cell lung cancer: a single center experience. Eur J Cardiothorac Surg 2012;42:83-8. [PubMed]
- Gossot D, Ramos R, Brian E, et al. A totally thoracoscopic approach for pulmonary anatomic segmentectomies. Interact Cardiovasc Thorac Surg 2011;12:529-32. [PubMed]
- Soukiasian HJ, Hong E, McKenna RJ Jr. Video-assisted thoracoscopic trisegmentectomy and left upper lobectomy provide equivalent survivals for stage IA and IB lung cancer. J Thorac Cardiovasc Surg 2012;144:S23-6. [PubMed]
- Yamada S, Suga A, Inoue Y, et al. Use of multi-detector row angiography for the arrangement of video-assisted modified segmental resection. Eur J Cardiothorac Surg 2009;36:727-30. [PubMed]
- Fukuhara K, Akashi A, Nakane S, et al. Preoperative assessment of the pulmonary artery by three-dimensional computed tomography before video-assisted thoracic surgery lobectomy. Eur J Cardiothorac Surg 2008;34:875-7. [PubMed]
- Segmentectomy of the left upper lobe. In: Nomori H, Okada M. eds. Illustrated anatomical segmentectomy for lung cancer. Tokyo: Spinger, 2011:137-92.
- Miyasaka Y, Oh S, Takahashi N, et al. Postoperative complications and respiratory function following segmentectomy of the lung - comparison of the methods of making an inter-segmental plane. Interact Cardiovasc Thorac Surg 2011;12:426-9. [PubMed]