Systematic review of outcomes of combined proximal stentgrafting with distal bare stenting for management of aortic dissection
Abstract
Objective: Available data on outcomes of combined proximal stent-grafting with distal bare stenting for management of aortic dissection are limited. The objective of this study was to provide a systematic review of outcomes of this approach.
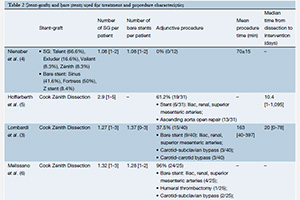
Methods: Studies involving combined proximal stent-grafting with distal bare stenting for management of aortic dissection were systematically searched and reviewed through MEDLINE databases.
Results: A total of four studies were included: 108 patients treated for management of acute (n=54) and chronic (n=54) aortic dissection. The technical success rate was 95.3% (range, 84-100%). The 30-day mortality rate was 2.7% (range from 0% to 5%). The morbidity rate occurring within 30 days was 51.8% (range from 0% to 65%) and included stroke (2.7%), paraplegia (2.7%), retrograde dissection (1.8%), renal failure (14.8%), severe cardiopulmonary complications (5.5%) and bowel ischemia (0.9%). The incidence of type I endoleak was 9.2% (10/108). During follow-up, 5 (4.6%) deaths were related to aortic rupture or aortic repair. Mean re-intervention rate was 12.9%. Two cases (1.9%) of delayed retrograde type A dissection and one case of aortobronchial fistula (0.9%) were reported. The most common delayed complication was thoracic stent-graft migration (4.7%). The rate of device failure was 9.2%. Favorable aortic remodeling was observed: studies reporting midterm follow-up of the true lumen demonstrated a high rate of both false lumen regression and true lumen expansion. At 12 months, complete false lumen thrombosis was observed at the thoracic level in 70.4% and at the abdominal level in 13.5% of patients.
Conclusions: Combined proximal stent-grafting with distal bare stenting appears to be a feasible approach for the management of Type B aortic dissection. Although this approach clearly improved true lumen perfusion and diameter, it failed to completely suppress false lumen patency. However, it should be acknowledged that contemporary data on this approach is limited to small studies with variable results.
Cover